Abstract
Pre-eclampsia is associated with postnatal cardiac dysfunction; however, the nature of this relationship remains uncertain. This multicentre retrospective cohort study aimed to determine the prevalence of pre-eclampsia in women with pre-existing cardiac dysfunction (left ventricular ejection fraction < 55%) and explore the relationship between pregnancy outcome and pre-pregnancy cardiac phenotype. In this cohort of 282 pregnancies, pre-eclampsia prevalence was not significantly increased (4.6% [95% C.I 2.2–7.0%] vs. population prevalence of 4.6% [95% C.I. 2.7–8.2], p = 0.99); 12/13 women had concurrent obstetric/medical risk factors for pre-eclampsia. The prevalence of preterm pre-eclampsia (< 37 weeks) and fetal growth restriction (FGR) was increased (1.8% vs. 0.7%, p = 0.03; 15.2% vs. 5.5%, p < 0.001, respectively). Neither systolic nor diastolic function correlated with pregnancy outcome. Antenatal ß blockers (n = 116) were associated with lower birthweight Z score (adjusted difference − 0.31 [95% C.I. − 0.61 to − 0.01], p = 0.04). To conclude, this study demonstrated a modest increase in preterm pre-eclampsia and significant increase in FGR in women with pre-existing cardiac dysfunction. Our results do not necessarily support a causal relationship between cardiac dysfunction and pre-eclampsia, especially given the population’s background risk status. The mechanism underpinning the relationship between cardiac dysfunction and FGR merits further research but could be influenced by concomitant ß blocker use.
Similar content being viewed by others
Introduction
There is abundant observational data linking pre-eclampsia with postnatal maternal cardiac dysfunction1,2,3 and long-term cardiovascular risk4,5,6,7,8,9,10,11,12,13,14,15. However, the mechanistic link between cardiac dysfunction and pre-eclampsia remains inconclusive: it is unclear whether it is causal16,17 or consequential18,19. There is evidence to support a pre-eclampsia dose–effect: the more severe pre-eclampsia phenotypes (determined by presence of severe features5,8,11,12,13,20, gestation at onset4,6,7,10, reduced fetal size13,21 and recurrence8,22 are associated with increased future cardiovascular risk. Indeed, preterm pre-eclampsia (< 37 weeks’ gestation) is associated with worse maternal diastolic dysfunction3,23 and potentially worse cardiac remodelling24, although evidence for the latter is more conflicted3,25.
Animal studies have also sought to investigate the direction of causation, with mixed results26,27,28,29,30. An alternative approach is to examine pre-eclampsia rates in women with pre-existing cardiac dysfunction. Pre-eclampsia and fetal growth restriction (FGR) are presumed to be placental in origin31,32,33,34. In this way, if inadequate cardiac function contributes significantly to impaired placental development, women with pre-existing cardiac dysfunction should have disproportionately increased pre-eclampsia and FGR rates. A number of large retrospective registry studies35,36,37,38,39,40,41,42,43 have previously investigated obstetric outcomes in women with known cardiac disease. However, pre-eclampsia prevalence was not the primary focus of these studies, and therefore to our knowledge, no one has correlated pre-pregnancy cardiac parameters with pregnancy outcome and pre-eclampsia risk factors have largely been overlooked.
The aim of this study was to determine the prevalence of pre-eclampsia and FGR (clinical proxies for placental dysfunction) in women with pre-existing cardiac dysfunction, aiming to improve:
-
1.
Our understanding of the relationship between cardiac and placental function, to inform future preventative and therapeutic strategies;
-
2.
Counselling of women with cardiac disease and their families, before and during pregnancy.
Results
The study cohort included 282 pregnancies from 244 women (Fig. 1). Supplementary Table S1 describes the spread of participants from different sites. Results were derived from the 282 pregnancies but were not altered by only including each woman’s first pregnancy.
Demographics and baseline characteristics
Distribution of baseline characteristics of the cohort are summarised in Table 1. Left ventricular ejection fraction (LVEF) data were derived from early pregnancy (< 12 weeks) in 16/282 (5.7%) women, where pre-pregnancy echocardiography data were not available. DCM affected 156/282 (55.3%) of the cohort. Of those with dilated cardiomyopathy (DCM), 50/156 (32.1%) were familial, 3/156 (1.9%) were idiopathic, 63/156 (40.4%) were acquired and 35/156 (22.4%) were due to previous PPCM.
The majority of women were New York Heart Association (NYHA) functional classification I (109/282 [38.7%]); 64/282 (22.7%) were class II; 14/282 (5.0%) were class III, and 95/282 (33.7%) were unknown. Table 2 summarises the baseline echocardiography parameters of the cohort. Thirty-two (11.3%) women had severe systolic dysfunction (LVEF ≤ 35%); 110/282 (39.0%) had impaired LVEF and 140/282 (49.6%) had borderline LVEF. Echocardiography data, beyond LVEF was not available for every participant. Concentric remodelling/hypertrophy affected 13/126 (10.3%) and eccentric hypertrophy affected 51/126 (40.5%) women.
ß blockers were taken by 116/243 (47.7%) women antenatally. Information on the type of ß blocker was available for 77/116 (66.4%) women; bisoprolol was the most commonly prescribed ß blocker (68/77, 88.3%). Antenatal aspirin was taken in 102/257 (39.7%) pregnancies (Supplementary Table S2). All women with ischaemic heart disease (n = 12) took aspirin during pregnancy.
Pregnancy outcomes
Table 3 summarises the pregnancy outcomes of the cohort. The median gestation at delivery was 3822,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42 completed weeks and 123/273 (45.0%) delivered by Caesarean section. Thirteen (4.6%) women developed pre-eclampsia. Five (38.5%) of these women delivered before 37 weeks, 3/13 (23.1%) before 34 weeks and 12/13 (92.3%) had risk factors for pre-eclampsia (including hypertension, renal disease, antiphospholipid syndrome, obesity, nulliparity and diabetes; Supplementary Table S3). Within the cohort, 74/279 (26.5%) met the criteria for antenatal aspirin44. For those women where antenatal aspirin was indicated due to pre-eclampsia risk factors44 and for whom pre-eclampsia risk factors and aspirin use were known, 45/69 (65.2%) took aspirin antenatally. Pre-eclampsia prevalence observed in this cohort was not significantly increased compared with the general population45 (4.6% [95%C.I 2.2–7.0%] vs. 4.6% [95% C.I. 2.7–8.2], p = 0.99). On the other hand, preterm pre-eclampsia prevalence was increased relative to population prevalence46 (1.8% [95% C.I. 0.2–3.3] vs. 0.7% [95% C.I. 0.6–0.8], p = 0.03); this did not retain statistical significance when only women with DCM were included (Supplementary Table S4). Three (60.0%) of those with preterm pre-eclampsia had co-existent FGR. Prevalence of FGR and small for gestational age (SGA) in women with pre-existing cardiac impairment were higher than that of the background population (FGR: 15.2% [95% C.I. 10.9–19.5%] vs. 5.5% [95% C.I. 5.3–5.7], p < 0.001; SGA: 32.0% [95% C.I. 26.4–37.5%] vs. 18.2% [95% C.I. 17.9–18.6], p < 0.001).
Of the 13 women with pre-eclampsia, six were nulliparous. There was no significant difference in pregnancy outcome between nulliparous and multiparous women in this cohort (pre-eclampsia: 7.2% vs. 3.5%, p = 0.18; preterm pre-eclampsia: 2.4% vs. 1.5%, p = 0.27; FGR: 19.8% vs. 13.3%, p = 0.18; preterm FGR: 11.3% vs. 5.7%, p = 0.11). Similarly, when only nulliparous women were included in the analysis (n = 83), pre-eclampsia prevalence remained comparable with background population (7.2% [95% C.I. 1.6–12.8%] vs. 4.6% [95% C.I. 2.7–8.2], p = 0.65). Pre-eclampsia and preterm pre-eclampsia rates in the nulliparous women were also comparable with the SCOPE study47, which included nulliparous low-risk women (pre-eclampsia: 7.2% [95% C.I. 1.6–12.8%] vs. 5.3% [95% C.I. 4.6–6.0%], p = 0.44; preterm pre-eclampsia: 2.4% [95% C.I. − 0.9–5.7%] vs. 1.3% [95% C.I. 1.0–1.7%], p = 0.40). Pre-eclampsia rates were also comparable with the SCOPE study47 when the whole cohort was included (pre-eclampsia: 4.6% [95% C.I. 2.2–7.1%] vs. 5.3% [95% C.I. 4.6–6.0%], p = 0.62; preterm pre-eclampsia: 1.8% [95% C.I. 0.2–3.3%] vs. 1.3% [95% C.I. 1.0–1.7%], p = 0.54).
Preterm delivery and preterm FGR were also more prevalent than in the background population (preterm delivery: 26.3% [95% C.I. 21.1–31.4%] vs. 8.2% [95% C.I. 8.0–8.5], p < 0.001; preterm FGR: 7.4% [95% C.I. 4.3–10.6%] vs. 1.5% [95% C.I. 1.4–0.2], p < 0.001). Pre-eclampsia affected 2/6 (33.3%) women with early-onset (< 34 weeks) FGR. Fifty-eight (21.3%) women had iatrogenic delivery < 37 weeks, of whom 45/58 (77.6%) were indicated by routine obstetric factors/maternal disease only. None of the women who suffered placental abruption (n = 4) had evidence of pre-eclampsia. Figure 2 illustrates the distribution of birthweight Z score and gestation at delivery in this cohort compared with the background population.
Histograms of (A) birthweight Z score in this cohort; (B) birthweight Z score in the background population; (C) gestation at delivery (completed weeks) in this cohort; and (D) gestation at delivery (completed weeks) in the background population. Background population distributions were derived from 5-year data (2016–2020) from St Mary’s Hospital, Manchester, UK.
Relationship between cardiac parameters and pregnancy outcome
Severity of left ventricular (LV) impairment did not correlate with prevalence of pre-eclampsia (Supplementary Table S5, p = 0.35), SGA (p = 0.24), FGR (p = 0.67), or preterm delivery < 34 weeks (p = 0.26). LV impairment severity also did not correlate with birthweight Z score or gestation at delivery. Ischaemic heart disease was not associated with pre-eclampsia prevalence but was associated with earlier gestation at delivery and lower birthweight Z score (log-transformed difference − 0.08 days [95% C.I. − 0.14 to − 0.03], p = 0.002 and difference -0.84 [95% C.I. − 1.50 to − 0.17], p = 0.01, respectively). The relationship between ischaemic heart disease and birthweight Z score did not persist after adjustment for smoking (adjusted difference -0.65 [95% C.I. − 1.34–0.03], p = 0.06). Neither DCM, valvular nor hypertensive cardiomyopathy correlated with pregnancy outcome (including pre-eclampsia diagnosis, birthweight Z score and gestation at delivery). NYHA status was not associated with prevalence of pre-eclampsia (p = 0.62) or FGR (p = 0.15).
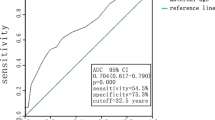
In terms of pre-pregnancy echocardiography parameters, LV systolic and diastolic function did not correlate with pregnancy outcome (Table 4 and Supplementary Tables S6 and S7). Increased LV mass index (LVMi) weakly correlated with increased pre-eclampsia prevalence (5 g/m2 increase in LVMi: OR 1.18 [95% C.I. 1.01–1.38], p = 0.04; Table 4). This did not persist after adjustment for pre-eclampsia risk factors and booking mean arterial pressure (MAP; adjusted OR 1.16 [95% C.I. 0.98–1.37], p = 0.08). Aortic and mitral stenosis and pulmonary regurgitation were also associated with increased pre-eclampsia prevalence (OR 6.0 [95% C.I. 1.42–25.33], p = 0.02; OR 6.86 [95% C.I. 1.24–37.80], p = 0.02; and OR 4.00 [95% C.I. 1.10–14.57], respectively), but statistical significance was lost after adjustment as above (Supplementary Table S8). No pre-pregnancy echocardiography parameters correlated with birthweight Z score or gestation at delivery, except presence of concentric hypertrophy, which was associated with earlier gestation at delivery (log-transformed difference: -0.10 days [95% C.I. − 0.18 to − 0.03], p = 0.01) and tricuspid annular plane systolic excursion (TAPSE; a measure of right ventricular function) which weakly correlated with birthweight z score (coefficient: 0.04 [95% C.I. 0.00–0.08]).
Pre-eclampsia prevalence was not associated with any antenatal medication. SGA and FGR were more prevalent in women taking ß blockers antenatally (SGA: 49/127 [38.6%] vs. 37/138 [26.8%], p = 0.04; FGR: 28/127 [22.0%] vs. 13/138 [9.4%], p = 0.005). Antenatal exposure to heparin was associated with a higher prevalence of FGR (16/65 [24.6%] vs. 22/196 [11.2%], p = 0.008). The relationship between heparin and birthweight Z score was lost after adjustment for pre-existing hypertension, underlying cardiac diagnosis and LV impairment severity (adjusted difference: − 0.29 [95% C.I. − 0.61–0.04], p = 0.09). Antenatal ß blocker use was associated with lower birthweight Z score, even after adjustment for pre-existing hypertension, underlying cardiac diagnosis and severity of LV impairment (adjusted difference − 0.31 [95% C.I. − 0.61 to − 0.01], p = 0.04). Furthermore, this relationship persisted after adjustment for smoking (adjusted difference − 0.38 [95% C.I. − 0.67 to − 0.09], p = 0.01) and when only those known to have taken bisoprolol were included (difference − 0.43 [95% C.I. − 0.76 to − 0.10], p = 0.01). Exploratory analyses comparing birthweight Z score in women who took bisoprolol antenatally with those who were known to take alternative ß blockers (n = 17) demonstrated no difference (difference 1.12 [95% C.I. − 0.42–2.68], p = 0.15). The association between antenatal ß blockers and earlier gestation at delivery was lost after adjustment for LVEF (adjusted log-transformed difference: − 0.02 [95% C.I. − 0.04–0.00], p = 0.09). Supplementary Table S9 compares maternal characteristics between those exposed to ß blockers antenatally and those not.
Cardiac outcomes
Major adverse cardiovascular events (MACE) occurred in 3/282 (1.1%) pregnancies: one woman with LV non-compaction cardiomyopathy had a transient ischaemic attack and there were two maternal deaths (drug overdose and valvular thrombosis one month postpartum associated with a mechanical aortic valve). Thirty-six (12.8%) women developed acute heart failure and 14/282 (5.0%) developed pulmonary oedema. Sustained arrhythmia complicated 13/282 (4.6%) pregnancies. Table 5 summarises the prevalence of adverse cardiac outcomes according to severity and cause of cardiac dysfunction. Acute heart failure was most common in those with DCM (19.5%) and severely impaired LVEF (41.9%).
Discussion
This study describes a large retrospective cohort of pregnancies affected by pre-existing maternal heart disease. Pre-eclampsia prevalence was not increased compared to the general population, however preterm pre-eclampsia, SGA and FGR prevalence were. Routinely indicated preterm and early term delivery and Caesarean sections were common in this cohort. The severity of LV impairment did not correlate with any pregnancy outcome and there was only one case of pre-eclampsia amongst the pregnancies complicated by severely impaired baseline LVEF.
Antenatal ß blocker use was consistently associated with adverse pregnancy outcome, including increased SGA and FGR and reduced birthweight centile, despite adjustment for confounders. In those who were prescribed ß blockers, bisoprolol was the most commonly used agent.
Adverse cardiac events, although less frequent than previous reports in the literature38,39, were by no means uncommon, thereby endorsing close antenatal and postnatal surveillance in this high-risk group. Women with valvular disease were at particular increased risk of MACE and those with severely impaired LVEF had the highest risk of acute heart failure.
This was a relatively large multicentre study comprising data from 13 sites across the UK and Australia. Inclusion of 282 pregnancies affected by maternal cardiomyopathy allowed correlation of pre-existing cardiac parameters with pregnancy outcome. To our knowledge, this is the first study of women with pre-existing cardiac disease, in which the primary outcome is pre-eclampsia, thereby ensuring adjustment for pre-eclampsia risk factors, where appropriate. Although the retrospective nature of the study has its limitations, variables were pre-specified and confirmed by the clinical care team following careful review of clinical records. Heterogeneity of the cohort was compensated by subgroup analyses of women with DCM (thereby limiting confounding effects of structural heart disease on cardiac output (CO), LV geometry and function); these subgroup analyses demonstrated consistent findings with the whole cohort.
Unfortunately, background prevalence data for adverse pregnancy outcomes were not available from all sites; for this reason, the prevalence of SGA, FGR, preterm delivery and preterm FGR was estimated from five-year birth data from Saint Mary’s Hospital, Manchester. Although a tertiary centre with a high-risk population, Saint Mary’s Hospital was deemed an appropriate comparator as it contributed a large proportion of the cohort (99/282) and 11/13 of the sites are tertiary centres for Cardiology or Obstetrics. Pre-eclampsia is not reliably coded in UK hospital maternity information systems and therefore comparisons of rates of pre-eclampsia could only be made to published studies from comparable populations45,46,47. To compensate for this limitation, the influence and proportion of nulliparity and pre-eclampsia risk factors were explored.
If the link between cardiac dysfunction and pre-eclampsia is due to a problem with cardiovascular supply rather than demand, CO would be a useful pre-pregnancy parameter to determine this. Unfortunately, CO is not routinely reported in echocardiography and therefore it is not possible to explore the link between CO and pregnancy outcome, within this dataset. Additionally, the relatively mild LV functional impairment seen in this cohort (49.6% had LVEF 50–54%) may not have been enough to cause a significant drop in CO, thereby limiting any potential effect on uteroplacental perfusion. On the other hand, severity of LV impairment did not correlate with any measure of placental dysfunction, including pre-eclampsia, indicating a lack of causation.
Finally, for the purpose of this study, pre-eclampsia and FGR were considered clinical proxies for placental dysfunction, in the absence of confirmatory placental histology. This is due to the widely accepted theory of their mutual placental origin31,32,33,34, however this limits the ability to link pre-pregnancy cardiac parameters with distinct placental pathologies.
Pre-eclampsia prevalence was not increased in this cohort. However, routinely indicated early delivery in these women could have masked term pre-eclampsia. Additionally, frequent use of ß blockers could have masked late hypertension, thereby preventing a diagnosis of pre-eclampsia being made. On the other hand, the lack of association between systolic or diastolic function and pre-eclampsia, suggests that the cardiac dysfunction following pre-eclampsia3,48,49 is unlikely to be solely a consequence of pre-existing impairment. In contrast, increased LVMi was weakly associated with higher pre-eclampsia rates. This likely reflects pre-existing comorbidities, supported by the loss of relationship between LVMi and pre-eclampsia after adjustment for booking MAP and pre-eclampsia risk factors.
Although preterm pre-eclampsia rates were increased compared with those reported in the ASPRE trial46, this could in part be attributed to the increased prevalence of pre-eclampsia risk factors in this cohort (26.5% [95% C.I. 21.3–31.7%] vs. 4.0% [95% C.I. 3.8–4.2%], p < 0.001).
The high SGA and FGR rates in this cohort could be a consequence of reduced uteroplacental blood supply due to the underlying cardiomyopathy50 or concurrent medication (ß blockers)51,52, or contributed to by high smoking rates (20%). Alternatively, despite its ß1 cardio-selective nature53, bisoprolol could have a direct effect on the placental vasculature. This is supported by evidence of ß1 receptors54,55 in placental vasculature and placental vasoconstriction seen following exposure to ß blockers in vitro56,57. The potential negative effect of antenatal ß blocker use on fetal growth has long been considered51,58,59,60,61. A recent meta-analysis including 13 cohort studies demonstrated a significant increase in SGA associated with antenatal ß blocker use (OR 1.72 [95% C.I. 1.59–1.85], p < 0.001)58. It has been proposed that ß blocker subtypes are associated with varying risk51,59. Labetalol, which is an α and ß antagonist and partial ß2 agonist57,62,63, is commonly used as a first-line antihypertensive in pregnancy44. It is possible that the partial ß2 agonistic properties of labetalol induce vasodilation in placental and umbilical vasculature, thereby favourably increasing placental blood flow57,64,65. However atenolol, which selectively blocks ß1 adrenergic receptors, is not recommended in pregnancy44 due to negative associations with fetal growth60,66,67. The impact of bisoprolol, which was the most commonly prescribed ß blocker in this cohort, on fetal growth is less understood.
The rationale for ß blocker use in the context of cardiac dysfunction is to protect the heart against the deleterious effects of increased adrenergic activity, by reducing heart rate, blood pressure and myocardial oxygen demand68. It is therefore likely that continued antenatal use of ß blockers indicates a particular cardiac phenotype or degree of severity. However, the relationship between ß blockers and birthweight Z score persisted after adjustment for FGR risk factors and cardiac phenotype, indicating a direct mechanistic link between the two.
The relationship between antenatal heparin exposure and FGR was unexpected due to the wealth of existing data demonstrating no harmful effect of antenatal heparin on fetal growth69,70,71,72. Given the loss of significance after adjustment for confounders, this is unlikely to represent a causal relationship.
The lack of association between any measure of pre-pregnancy cardiac impairment and birthweight Z score/FGR makes a causal role of cardiac dysfunction in the development of FGR unlikely. Furthermore, if preterm FGR in this cohort shared the presumed aetiology of preterm pre-eclampsia, in which early placentation is affected by defective spiral artery remodelling31, the prevalence of co-existing hypertension (i.e. pre-eclampsia) should be higher. A third of women with early-onset FGR developed pre-eclampsia in this cohort, compared with 52–60% women in the early-onset FGR cohorts in TRUFFLE73 and STRIDER74. The lower-than-expected rate of pre-eclampsia in women with FGR suggests that late placental failure, rather than early placentation defects, may be a more significant cause of FGR in this cohort. This would also be supported by the association with ß blockers affecting third trimester growth51. In order to explore this further, measures of early placentation (including uterine artery Doppler, pregnancy-associated plasma protein-A, placental growth factor and placental pathology) need to be investigated in future cohorts.
In conclusion, this study provides valuable information to aid clinicians with pre-conception and antenatal counselling for women with cardiomyopathy. These women can be reassured that their risk of pre-eclampsia does not appear to be significantly increased, however serial ultrasound scanning is likely warranted to monitor for FGR. Preconception counselling should include information on the increased risk of acute heart failure in pregnancy for those with pre-existing cardiomyopathy (in particular severely impaired LVEF). The mechanism linking FGR and cardiac dysfunction remains unknown, however it could be attributed to reduced uteroplacental perfusion as a consequence of the underlying cardiac disease or concomitant ß blocker use. Further study is required to explore the effect of bisoprolol on the placenta. Finally, the absence of dose–effect demonstrated by lack of correlation between severity of cardiac dysfunction and pregnancy outcome does not support a causal role of cardiovascular dysfunction in the development of pre-eclampsia. Further study is needed to explore the mechanistic link between cardiac dysfunction and FGR.
Methods
This was a multicentre retrospective cohort study, including 12 UK sites and one Australian site. Research was limited to use of previously collected, non-identifiable information. For this reason, it was approved by the UK Health Research Authority (HRA; IRAS ID 261380) and the Australian Human Research Ethics Committees (HREC/60940/MonH-2020-203642) without the need for UK Research Ethical Committee review (as per the UK Integrated Research Application System [IRAS]).
The need for informed consent was waived by the HRA and Australian Human Research Ethics Committee, as identifiable patient data were not accessed outside of the primary clinical care team. All methods were carried out in accordance with the "Caldicott Principles", the Data Protection Act and the General Data Protection Regulation. Patients were not involved in the conduct of this study.
Study population
Women aged ≥ 16 years with pre-existing LV systolic impairment (LVEF < 55%), who had a pregnancy between January 2008 and December 2020, were included in the study. Women were excluded if they delivered before 22 weeks’ gestation or insufficient data were available. Data were collated from 13 sites in England, Scotland and Australia (Fig. 3).
Map of participating sites in (A) UK and (B) Australia. Blue stars highlight the 13 hospitals that collected data for the study. Maps are modified from Bruce Jones Design85.
Eligible participants were identified using different methods across sites, including via cardiac obstetric databases, clinic lists and ICD-10 codes (including heart failure and cardiomyopathy). Eligibility was checked following review of echocardiography reports, online clinical reports, clinic letters and case notes. Each site was given identical excel spreadsheets with pre-determined data fields to complete (Supplementary Table S10). Minimum data criteria included presence/absence of pre-eclampsia and evidence of LVEF < 55% pre-pregnancy or < 12 weeks’ gestation.
Cardiac classifications
LV impairment was categorised, as per British Society of Echocardiography (BSE) guidelines75, as borderline (50–54%), impaired (36–49%) and severely impaired (≤ 35%). DCM was defined as a combination of dilated left ventricle (LV internal diameter in end-diastole [LVIDd] > 5.2 cm)76 and systolic dysfunction, or evidence of DCM diagnosis by a cardiologist in the case notes. DCM was further categorised into familial, idiopathic, acquired (secondary to infection, chemotherapy, alcohol or iron overload) and previous peripartum cardiomyopathy (PPCM). As per the American Heart Association (AHA)77 and BSE guidance78, congenital, ischaemic, valvular and hypertensive heart disease were not included in the DCM definition, irrespective of LV cavity size.
Relative wall thickness (RWT) was calculated in end-diastole by: (interventricular septal wall thickness [IVSd] + posterior wall thickness [PWd])/LVIDd. Left ventricular mass (LVM) was derived from the following equation: 0.8(1.04[LVIDd + PWd + IVSd]3 − [LVIDd]3) + 0.6. Remodelling measures were then indexed to body surface area (BSA). BSA was calculated using the Mosteller formula79: Body surface area (BSA) = square root of (height (cm) × weight (kg)/3600). Concentric remodelling was defined as RWT ≥ 0.42 and hypertrophy was defined as LVMi > 95 g/m275,76. Left atrial dilatation was defined using the American and European 201576 (using indexed measures, if available) and 2006 guidelines80 (when indexed measures were not available). This definition is summarised in Supplementary Table S11.
Echocardiography parameters were used from the most recent pre-pregnancy scan or, when this was not available, < 12 weeks’ gestation.
Obstetric classifications
Pre-eclampsia was confirmed by documented diagnosis in the case notes or clinic letters. All cases met the International Society for the Study of Hypertension in Pregnancy (ISSHP) criteria for diagnosis81: new or worsening hypertension > 20 weeks and proteinuria or other suggestive features (abnormal haematological or biochemical parameters or FGR). Severe pre-eclampsia was defined as maximum blood pressure ≥ 160/110 mmHg, alanine aminotransferase > 100U/L, creatinine > 100 µmol/L or platelets < 100 × 109/L. Data for birthweight centile customisation was not available for all women. Therefore, the World Health Organization (WHO) population Z score was used82. Small-for-gestational-age (SGA; birthweight < 10th centile) equated to a Z score < − 1.282 and FGR (birthweight < 3rd centile)83 equated to a Z score < − 1.88182.
Population pre-eclampsia prevalence of 4.6% was derived from Abalos et al.’s systematic review45. Preterm pre-eclampsia prevalence (requiring delivery < 37 weeks; 0.7%) was derived from the ASPRE trial46, in which 4.0% of the population were high-risk for pre-eclampsia, according to NICE44. Population rates of SGA (18.2%), FGR (9.5%), preterm delivery (< 37 weeks; 8.2%) and preterm FGR (< 37 weeks; 1.5%) were derived from 5-year data (2016–2020) from Saint Mary’s Hospital, Manchester, UK84.
Outcomes
The primary outcome was to determine the prevalence of pre-eclampsia in women with pre-existing cardiac impairment, compared with the general population. Pre-specified secondary outcomes included: (1) the prevalence of FGR and SGA in women with pre-existing cardiac impairment, compared with the general population; the prevalence of pre-eclampsia, FGR and SGA depending on (2) primary cardiac diagnosis and (3) severity of LV impairment (by LVEF); (4) the relationship between gestation at birth/birthweight Z score and primary cardiac diagnosis/severity of LV impairment/other echocardiography parameters. An appropriate published core outcome set was not available and therefore not used in this study.
Cardiovascular endpoints included acute heart failure, pulmonary oedema, sustained arrhythmia, stroke, angina, myocardial infarction and cardiac arrest. Major adverse cardiovascular event (MACE) was defined by a composite outcome of stroke, myocardial infarction or maternal death.
Statistical analysis
Statistical analyses were performed using Stata v.14.2. Baseline characteristics of the cohort were represented as mean ± standard deviation/median (range) as appropriate for continuous data, or counts (percentage) for categorical data. Prevalence of primary and secondary outcomes were compared against quoted population prevalence, as described in the literature45,46, using equality of proportions test. Prevalence of these outcomes was also compared between groups using Chi-square test. Univariate analysis was used to identify those factors significantly associated with pregnancy outcome. Heavily skewed variables were log-transformed prior to analysis. Multivariable regression analyses allowed adjustment for confounding factors. Analyses were performed for the whole cohort and repeated for the DCM subgroup, aiming to reduce heterogeneity (in particular, by removing the functional and haemodynamic consequences of structural heart disease).
The prevalence of pre-eclampsia in the general population is 4.6%45. In order to identify a twofold increase in pre-eclampsia in this cohort (≥ 9.2%) compared with the general population, a sample size of 245 women was required at 80% power, α 0.05. From the initial single centre cohort study at Saint Mary’s Hospital 66 eligible cases were identified. It was therefore anticipated that 12 additional sites would be needed (recruiting 15 per site) to reach the target sample size.
Ethics approval
The protocol was approved by the UK HRA (without need for ethical committee review; IRAS ID 261380), the Australian Human Research Ethics Committees (HREC/60940/MonH-2020-203642) and the Research and Innovation teams at each site.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
De Haas, S. et al. Cardiac remodeling in normotensive pregnancy and in pregnancy complicated by hypertension: Systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 50(6), 683–696 (2017).
Evans, C. S. et al. Cardiovascular system during the postpartum state in women with a history of preeclampsia. Hypertension 58(1), 57–62 (2011).
Melchiorre, K., Sutherland, G. R., Liberati, M. & Thilaganathan, B. Preeclampsia is associated with persistent postpartum cardiovascular impairment. Hypertension 58(4), 709–715 (2011).
Irgens, H. U., Reisæter, L., Irgens, L. M. & Lie, R. T. Long term mortality of mothers and fathers after pre-eclampsia: Population based cohort study. Br. Med. J. 323(7323), 1213–1217 (2001).
Grandi, S. M. et al. Cardiovascular disease-related morbidity and mortality in women with a history of pregnancy complications: Systematic review and meta-analysis. Circulation 139(8), 1069–1079 (2019).
Arnott, C. et al. Maternal cardiovascular risk after hypertensive disorder of pregnancy. Heart 106(24), 1927–1933 (2020).
Smith, G. C. S., Pell, J. P. & Walsh, D. Pregnancy complications and maternal risk of ischaemic heart disease: A retrospective cohort study of 129 290 births. Lancet 357(9273), 2002–2006 (2001).
Wikström, A. K., Haglund, B., Olovsson, M. & Lindeberg, S. N. The risk of maternal ischaemic heart disease after gestational hypertensive disease. BJOG Int. J. Obstet. Gynaecol. 112(11), 1486–1491 (2005).
Mongraw-Chaffin, M. L., Cirillo, P. M. & Cohn, B. A. Preeclampsia and cardiovascular disease death: Prospective evidence from the child health and development studies cohort. Hypertension 56(1), 166–171 (2010).
Leon, L. J. et al. Preeclampsia and cardiovascular disease in a large UK pregnancy cohort of linked electronic health records: A CALIBER study. Circulation 140(13), 1050–1060 (2019).
McDonald, S. D., Malinowski, A., Zhou, Q., Yusuf, S. & Devereaux, P. J. Cardiovascular sequelae of preeclampsia/eclampsia: A systematic review and meta-analyses. Am. Heart J. 156(5), 918–930 (2008).
Lykke, J. A. et al. Hypertensive pregnancy disorders and subsequent cardiovascular morbidity and type 2 diabetes mellitus in the mother. Hypertension 53(6), 944–951 (2009).
Lykke, J. A., Langhoff-Roos, J., Lockwood, C. J., Triche, E. W. & Paidas, M. J. Mortality of mothers from cardiovascular and non-cardiovascular causes following pregnancy complications in first delivery. Paediatr. Perinat. Epidemiol. 24(4), 323–330 (2010).
Egeland, G. M. et al. Pregnancy-related risk factors are associated with a significant burden of treated hypertension within 10 years of delivery: Findings from a population-based Norwegian Cohort. J. Am. Heart Assoc. 7(10), e008318 (2018).
Akhter, T. et al. Association between angiogenic factors and signs of arterial aging in women with pre-eclampsia. Ultrasound Obstet. Gynecol. 50(1), 93–99 (2017).
Thilaganathan, B. Cardiovascular origins of Preeclampsia. Pregnancy Hypertens. Int. J. Women’s Cardiovasc. Health 7, 62–63 (2017).
Foo, F. L. et al. Association between prepregnancy cardiovascular function and subsequent preeclampsia or fetal growth restriction. Hypertension 72(2), 442–450 (2018).
Garrido-Gimenez, C. et al. Angiogenic factors and long-term cardiovascular risk in women that developed preeclampsia during pregnancy. Hypertension 76(6), 1808–1816 (2020).
Shahul, S. et al. Circulating antiangiogenic factors and myocardial dysfunction in hypertensive disorders of pregnancy. Hypertension 67(6), 1273–1280 (2016).
Bellamy, L., Casas, J. P., Hingorani, A. D. & Williams, D. J. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: Systematic review and meta-analysis. Br. Med. J. 335(7627), 974–977 (2007).
Riise, H. K. R. et al. Incident coronary heart disease after Preeclampsia: Role of reduced fetal growth, preterm delivery, and parity. J. Am. Heart Assoc. 6(3), e004158 (2017).
Auger, N. et al. Recurrent pre-eclampsia and subsequent cardiovascular risk. Heart 103(3), 235–243 (2017).
Soma Pillay, P. et al. Cardiac diastolic function after recovery from pre-eclampsia. Cardiovasc. J. Afr. 29(1), 26–31 (2018).
Vaddamani, S., Keepanasseril, A., Pillai, A. A. & Kumar, B. Maternal cardiovascular dysfunction in women with early onset preeclampsia and late onset preeclampsia: A cross-sectional study. Pregnancy Hypertens. 1(10), 247–250 (2017).
Boardman, H. et al. Variations in cardiovascular structure, function, and geometry in midlife associated with a history of hypertensive pregnancy. Hypertension 75(6), 1542–1550 (2020).
Pruthi, D. et al. Exposure to experimental preeclampsia in mice enhances the vascular response to future injury. Hypertension 65(4), 863–870 (2015).
Bytautiene, E. et al. Long-term alterations in maternal plasma proteome after sFlt1-induced preeclampsia in mice. Am. J. Obstet. Gynecol. 208(5), 388.e1-388.e10 (2013).
Bytautiene, E. et al. Long-term maternal cardiovascular function in a mouse model of sFlt-1-induced preeclampsia. Am. J. Physiol. Heart Circ. Physiol. 298(1), H189–H193 (2010).
Miralles, F. et al. Long-term cardiovascular disorders in the STOX1 mouse model of preeclampsia. Sci. Rep. 9(1), 1–13 (2019).
Garrett, N. et al. Pravastatin therapy during preeclampsia prevents long-term adverse health effects in mice. JCI Insight 3(8), e120147 (2018).
Staff, A. C. The two-stage placental model of preeclampsia: An update. J. Reprod. Immunol. 1(134–135), 1–10 (2019).
Sebire, N. J. Implications of placental pathology for disease mechanisms; methods, issues and future approaches. Placenta 52, 122–126 (2017).
Levytska, K. et al. Placental pathology in relation to uterine artery doppler findings in pregnancies with severe intrauterine growth restriction and abnormal umbilical artery doppler changes. Am J Perinatol. 34(5), 451–457 (2017).
Burton, G. J. & Jauniaux, E. Pathophysiology of placental-derived fetal growth restriction. Am. J. Obstet. Gynecol. 218, S745–S761 (2018).
Campanharo, F. F. et al. The impact of cardiac diseases during pregnancy on severe maternal morbidity and mortality in Brazil. PLoS ONE 10(12), e0144385 (2015).
Koutrolou-Sotiropoulou, P. et al. Impact of heart disease on maternal and fetal outcomes in pregnant women. Am. J. Cardiol. 116(3), 474–480 (2015).
Hayward, R. M., Foster, E. & Tseng, Z. H. Maternal and fetal outcomes of admission for delivery in women with congenital heart disease. JAMA Cardiol. 2(6), 664–671 (2017).
Lima, F. V., Parikh, P. B., Zhu, J., Yang, J. & Stergiopoulos, K. Association of cardiomyopathy with adverse cardiac events in pregnant women at the time of delivery. JACC Heart Fail. 3(3), 257–266 (2015).
Lima, F. V., Yang, J., Xu, J. & Stergiopoulos, K. National trends and in-hospital outcomes in pregnant women with heart disease in the United States. Am. J. Cardiol. 119(10), 1694–1700 (2017).
Siu, S. C. et al. Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation 104(5), 515–521 (2001).
Hink, E. & Bolte, A. C. Pregnancy outcomes in women with heart disease: Experience of a tertiary center in the Netherlands. Pregnancy Hypertens. 5(2), 165–170 (2015).
Beaton, A. et al. Impact of heart disease on maternal, fetal and neonatal outcomes in a low-resource setting. Heart 105(10), 755–760 (2019).
Owens, A. et al. Neonatal and maternal outcomes in pregnant women with cardiac disease. J. Am. Heart Assoc. 7(21), e009395 (2018).
Hypertension in pregnancy: Diagnosis and management [NG133] | Guidance and guidelines | NICE (2019).
Abalos, E., Cuesta, C., Grosso, A. L., Chou, D. & Say, L. Global and regional estimates of preeclampsia and eclampsia: A systematic review. Eur. J. Obstet. Gynecol. Reprod. Biol. 170(1), 1–7 (2013).
Poon, L. C. et al. ASPRE trial: Incidence of preterm pre-eclampsia in patients fulfilling ACOG and NICE criteria according to risk by FMF algorithm. Ultrasound Obstet. Gynecol. 51(6), 738–742 (2018).
Myers, J. E. et al. Angiogenic factors combined with clinical risk factors to predict preterm pre-eclampsia in nulliparous women: A predictive test accuracy study. BJOG Int. J. Obstet. Gynaecol. 120(10), 1215–1223 (2013).
Ormesher, L. et al. Postnatal enalapril to improve cardiovascular function following preterm preeclampsia (PICk-UP): A randomized double-blind placebo-controlled feasibility trial. Hypertension 76(6), 1828–1837 (2020).
McCarthy, F. P. et al. Planned delivery to improve postpartum cardiac function in women with preterm pre-eclampsia: The PHOEBE mechanisms of action study within the PHOENIX RCT. Effic. Mech. Eval. 8(12), 1–28 (2021).
Pieper, P. G. et al. Uteroplacental blood flow, cardiac function, and pregnancy outcome in women with congenital heart disease. Circulation 128(23), 2478–2487 (2013).
Tanaka, K. et al. Beta-blockers and fetal growth restriction in pregnant women with cardiovascular disease. Circ. J. 80(10), 2221–2226 (2016).
Räsänen, J. & Jouppila, P. Uterine and fetal hemodynamics and fetal cardiac function after atenolol and pindolol infusion. A randomized study. Eur. J. Obstet. Gynecol. 62(2), 195–201 (1995).
Nuttall, S. L., Routledge, H. C. & Kendall, M. J. A comparison of the β1-selectivity of three β1-selective β-blockers. J. Clin. Pharm Ther. 28(3), 179–186 (2003).
Resch, B. E., Ducza, E., GÁspÁr, R. & Falkay, G. Role of adrenergic receptor subtypes in the control of human placental blood vessels. Mol. Reprod. Dev. 66(2), 166–171 (2003).
Hynes, P. G., Friel, A. M., Smith, T. J. & Morrison, J. J. β-Adrenoceptor subtype expression in human placenta and umbilical arteries in normal and preeclamptic pregnancies. Hypertens. Pregnancy 27(2), 169–181 (2008).
Petersen, O. B., Skajaa, K., Svane, D., Gregersen, H. & Forman, A. The effects of dihydralazine, labetalol and magnesium sulphate on the isolated, perfused human placental cotyledon. BJOG Int. J. Obstet. Gynaecol. 101(10), 871–878 (1994).
Erkinaro, T. et al. Placental and fetal hemodynamics after labetalol or pindolol in a sheep model of increased placental vascular resistance and maternal hypertension. Reprod Sci. 16(8), 749–757 (2009).
Liu, Q., Ling, G.-J., Zhang, S.-Q., Zhai, W.-Q. & Chen, Y.-J. The effects on fetal outcome of the use of beta-blockers during pregnancy: A systematic review and meta-analysis. Int. J. Clin. Exp. Med. 12(12), 13943–13950 (2019).
Duan, L., Ng, A., Chen, W., Spencer, H. T. & Lee, M. S. Beta-blocker subtypes and risk of low birth weight in newborns. J. Clin. Hypertens. 20(11), 1603–1609 (2018).
Ersbøll, A., Hedegaard, M., Søndergaard, L., Ersbøll, M. & Johansen, M. Treatment with oral beta-blockers during pregnancy complicated by maternal heart disease increases the risk of fetal growth restriction. BJOG Int. J. Obstet. Gynaecol. 121(5), 618–626 (2014).
Hoeltzenbein, M. et al. Pregnancy outcome after first trimester exposure to bisoprolol: An observational cohort study. J. Hypertens. 36(10), 2109–2117 (2018).
Baum, T. & Sybertz, E. J. Pharmacology of labetalol in experimental animals. Am. J. Med. 75(4 PART 1), 15–23 (1983).
Tadepalli, A. S. & Novak, P. J. Intrinsic sympathomimetic activity of labetalol. J. Cardiovasc. Pharmacol. 8(1), 44–50 (1986).
Ferro, A. et al. Activation of nitric oxide synthase by β2-adrenoceptors in human umbilical vein endothelium in vitro. Br. J. Pharmacol. 126(8), 1872–1880 (1999).
Yao, K., Xu, B., Liu, Y.-P. & Ferro, A. Effects of beta-adrenoceptor stimulation on endothelial nitric-oxide synthase phosphorylation of human umbilical vein endothelial cells. Acta Pharmacol. Sin. 24(3), 219–224 (2016).
Lydakis, C., Lip, G. Y. H., Beevers, M. & Beevers, D. G. Atenolol and fetal growth in pregnancies complicated by hypertension. Am. J. Hypertens. 12(6), 541–547 (1999).
Easterling, T. R., Brateng, D., Schmucker, B., Brown, Z. A. N. E. & Millard, S. P. Prevention of preeclampsia: A randomized trial of atenolol in hyperdynamic patients before onset of hypertension. Obstet. Gynecol. 93(5), 725–733 (1999).
Gheorghiade, M., Colucci, W. S. & Swedberg, K. β-blockers in chronic heart failure. Circulation 107(12), 1570–1575 (2003).
Rodger, M. A. et al. Meta-analysis of low-molecular-weight heparin to prevent recurrent placenta-mediated pregnancy complications. Blood 123(6), 822–828 (2014).
Dodd, J. M., Mcleod, A., Windrim, R. C. & Kingdom, J. Antithrombotic therapy for improving maternal or infant health outcomes in women considered at risk of placental dysfunction. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD006780.pub3 (2013).
Roberge, S. et al. Prevention of pre-eclampsia by low-molecular-weight heparin in addition to aspirin: A meta-analysis. Ultrasound Obstet. Gynecol. 47(5), 548–553 (2016).
Rodger, M. A. et al. Low-molecular-weight heparin and recurrent placenta-mediated pregnancy complications: A meta-analysis of individual patient data from randomised controlled trials. Lancet 388(10060), 2629–2641 (2016).
Lees, C. et al. Perinatal morbidity and mortality in early-onset fetal growth restriction: Cohort outcomes of the trial of randomized umbilical and fetal flow in Europe (TRUFFLE). Ultrasound Obstet. Gynecol. 42(4), 400–408 (2013).
Sharp, A. et al. Maternal sildenafil for severe fetal growth restriction (STRIDER): A multicentre, randomised, placebo-controlled, double-blind trial. Lancet Child Adolesc. Health 2(2), 93 (2018).
Harkness, A. et al. Normal reference intervals for cardiac dimensions and function for use in echocardiographic practice: A guideline from the British Society of Echocardiography. Echo Res. Pract. 7(1), G1–G18 (2020).
Lang, R. M. et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 28(1), 1–39 (2015).
Maron, B. J. et al. Contemporary definitions and classification of the cardiomyopathies: An American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation 113(14), 1807–1816 (2006).
Mathew, T. et al. Diagnosis and assessment of dilated cardiomyopathy: A guideline protocol from the British Society of Echocardiography. Echo Res. Pract. 4(2), G1-13 (2017).
Orimadegun, A. & Omisanjo, A. Evaluation of five formulae for estimating body surface area of Nigerian children. Ann. Med. Health Sci. Res. 4(6), 889 (2014).
Lang, R. M. et al. Recommendations for chamber quantification. Eur. J. Echocardiogr. 7, 79–108 (2006).
Tranquilli, A. L. et al. The classification, diagnosis and management of the hypertensive disorders of pregnancy: A revised statement from the ISSHP. Pregnancy Hypertens. 4(2), 97–104 (2014).
Kiserud, T. et al. The World Health Organization fetal growth charts: A multinational longitudinal study of ultrasound biometric measurements and estimated fetal weight. PLOS Med. 14(1), e1002220 (2017).
Gordijn, S. J. et al. Consensus definition of fetal growth restriction: A Delphi procedure. Ultrasound Obstet. Gynecol. 48, 333–339 (2016).
Wilkinson, M., Johnstone, E. D., Simcox, L. E. & Myers, J. E. The impact of COVID-19 on pregnancy outcomes in a diverse cohort in England. Sci. Rep. 12(1), 1–10 (2022).
Printable, Blank UK, United Kingdom Outline Maps • Royalty Free. Available from: http://www.freeusandworldmaps.com/html/Countries/EuropeCountries/UnitedKingdomPrint.html
Acknowledgements
We thank Dr Cathy Head for facilitating collaborations through UK Maternal Cardiac Society, Lizzy Cottrell and Andy Trafford for supervision and Omar Asghar for assistance with cardiological classifications.
Funding
This study was carried out as part of a Medical Research Council-funded fellowship (MR/R001693/1).
Author information
Authors and Affiliations
Contributions
L.O. conceived the study, collated and analysed the data and drafted the article, supervised by J.M. and E.D.J. L.O., S.V., S.H., S.C., V.O., F.A., C.H., V.S., A.R., E.O., M.R., K.P., M.S., L.M., S.M., N.M., J.C., E.H. collected data. All authors agreed the manuscript’s final version.
Corresponding author
Ethics declarations
Competing interests
LM is supported by the NIHR Oxford Biomedical Research Centre and part-time employee of Sensyne Health plc. The remaining authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ormesher, L., Vause, S., Higson, S. et al. Prevalence of pre-eclampsia and adverse pregnancy outcomes in women with pre-existing cardiomyopathy: a multi-centre retrospective cohort study. Sci Rep 13, 153 (2023). https://doi.org/10.1038/s41598-022-26606-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-26606-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.