Abstract
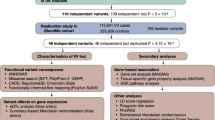
Varicose veins represent a common cause of cardiovascular morbidity, with limited available medical therapies. Although varicose veins are heritable and epidemiologic studies have identified several candidate varicose vein risk factors, the molecular and genetic basis remains uncertain. Here we analyzed the contribution of common genetic variants to varicose veins using data from the Veterans Affairs Million Veteran Program and four other large biobanks. Among 49,765 individuals with varicose veins and 1,334,301 disease-free controls, we identified 139 risk loci. We identified genetic overlap between varicose veins, other vascular diseases and dozens of anthropometric factors. Using Mendelian randomization, we prioritized therapeutic targets via integration of proteomic and transcriptomic data. Finally, topological enrichment analyses confirmed the biologic roles of endothelial shear flow disruption, inflammation, vascular remodeling and angiogenesis. These findings may facilitate future efforts to develop nonsurgical therapies for varicose veins.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
Full GWAS summary statistics from MVP can be found in dbGaP (https://www.ncbi.nlm.nih.gov/gap/) under the MVP accession (phs001672). GWAS summary statistics from FinnGen (release 4), BioBank Japan and UK Biobank are publicly available from https://www.finngen.fi/en/access_results, https://pheweb.jp/ and https://pan.ukbb.broadinstitute.org. The following datasets were used in the Topological Enrichment Analyses: GEO: GSE121520, GSE201376, GSE53998, GSE29611, GSE60156, GSE41166, GSE31838, GSE31477, GSE33213, GSE33213, GSE43786, GSE50144. GTEx v.8 RNA-seq datasets were downloaded from the GTEx Portal: https://gtexportal.org/.
Code availability
Publicly available software was used to perform analyses.
References
Criqui, M. H. et al. Chronic venous disease in an ethnically diverse population: the San Diego Population Study. Am. J. Epidemiol. 158, 448–456 (2003).
Evans, C. J., Fowkes, F. G., Ruckley, C. V. & Lee, A. J. Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population: Edinburgh Vein Study. J. Epidemiol. Community Health 53, 149–153 (1999).
Brand, F. N., Dannenberg, A. L., Abbott, R. D. & Kannel, W. B. The epidemiology of varicose veins: the Framingham Study. Am. J. Prev. Med. 4, 96–101 (1988).
Zahariev, T. et al. Prevalence of primary chronic venous disease: the Bulgarian experience. Int. Angiol. 28, 303–310 (2009).
Lurie, F. et al. The 2020 update of the CEAP classification system and reporting standards. J. Vasc. Surg. Venous Lymphat. Disord. 8, 342–352 (2020).
Müller-Bühl, U. et al. Varicose veins are a risk factor for deep venous thrombosis in general practice patients. Vasa 41, 360–365 (2012).
Chang, S.-L. et al. Association of varicose veins with incident venous thromboembolism and peripheral artery disease. JAMA 319, 807–817 (2018).
Bergan, J. J. et al. Chronic venous disease. N. Engl. J. Med. 355, 488–498 (2006).
Raffetto, J. D. Pathophysiology of chronic venous disease and venous ulcers. Surg. Clin. North Am. 98, 337–347 (2018).
Fukaya, E. et al. Clinical and genetic determinants of varicose veins. Circulation 138, 2869–2880 (2018).
Anwar, M. A. et al. A review of familial, genetic, and congenital aspects of primary varicose vein disease. Circ. Cardiovasc. Genet. 5, 460–466 (2012).
Shadrina, A. S., Sharapov, S. Z., Shashkova, T. I. & Tsepilov, Y. A. Varicose veins of lower extremities: insights from the first large-scale genetic study. PLoS Genet. 15, e1008110 (2019).
Ellinghaus, E. et al. Genome-wide association analysis for chronic venous disease identifies EFEMP1 and KCNH8 as susceptibility loci. Sci. Rep. 7, 45652 (2017).
Gaziano, J. M. et al. Million Veteran Program: a mega-biobank to study genetic influences on health and disease. J. Clin. Epidemiol. 70, 214–223 (2016).
Bulik-Sullivan, B. K. et al. LD score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat. Genet. 47, 291–295 (2015).
Piazza, G. Varicose veins. Circulation 130, 582–587 (2014).
Foley, C. N. et al. A fast and efficient colocalization algorithm for identifying shared genetic risk factors across multiple traits. Nat. Commun. 12, 764 (2021).
Paré, G. et al. Novel association of ABO histo-blood group antigen with soluble ICAM-1: results of a genome-wide association study of 6,578 women. PLoS Genet. 4, e1000118 (2008).
Kiechl, S. et al. Association of variation at the ABO locus with circulating levels of soluble intercellular adhesion molecule-1, soluble P-selectin, and soluble E-selectin: a meta-analysis. Circ. Cardiovasc. Genet. 4, 681–686 (2011).
Sánchez, F. S. L., Martínez, J. A. C., Méndez-García, L., García-Cenador, M. B. & Pericacho, M. Endoglin and other angiogenesis markers in recurrent varicose veins. J. Pers. Med. 12, 528 (2022).
Bryan, L. J., Callas, P. W., Criqui, M. H. & Cushman, M. Higher soluble P-selectin is associated with chronic venous insufficiency: the San Diego Population Study. Thromb. Res. 130, 716–719 (2012).
Grudzińska, E. & Czuba, Z. P. Immunological aspects of chronic venous disease pathogenesis. Cent. Eur. J. Immunol. 39, 525–531 (2014).
Aunapuu, M. & Arend, A. Histopathological changes and expression of adhesion molecules and laminin in varicose veins. Vasa 34, 170–175 (2005).
Nelson, C. P. et al. Genetically determined height and coronary artery disease. N. Engl. J. Med. 372, 1608–1618 (2015).
Demange, P. A. et al. Investigating the genetic architecture of noncognitive skills using GWAS-by-subtraction. Nat. Genet. 53, 35–44 (2021).
Davies, N. M., Holmes, M. V. & Davey Smith, G. Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. BMJ Online https://doi.org/10.1136/bmj.k601 (2018).
Zheng, J. et al. Phenome-wide Mendelian randomization mapping the influence of the plasma proteome on complex diseases. Nat. Genet. 52, 1122–1131 (2020).
Gaziano, L. et al. Actionable druggable genome-wide Mendelian randomization identifies repurposing opportunities for COVID-19. Nat. Med. 27, 668–676 (2021).
Jull, A. B., Arroll, B., Parag, V. & Waters, J. Pentoxifylline for treating venous leg ulcers. Cochrane Database Syst. Rev. 2012, CD001733 (2012).
Sey, N. Y. A. et al. A computational tool (H-MAGMA) for improved prediction of brain-disorder risk genes by incorporating brain chromatin interaction profiles. Nat. Neurosci. 23, 583–593 (2020).
Hyman, A. J., Tumova, S. & Beech, D. J. Piezo1 channels in vascular development and the sensing of shear stress. Curr. Top. Membr. 79, 37–57 (2017).
Purgatorio, G. et al. Germline GATA2 variant disrupting endothelial eNOS cell function and angiogenesis can be restored by c-Jun/AP-1 upregulation. Haematologica https://doi.org/10.3324/haematol.2021.278450 (2021).
Xie, Z. et al. Current knowledge of Krüppel-like factor 5 and vascular remodeling: providing insights for therapeutic strategies. J. Mol. Cell. Biol. 13, 79–90 (2021).
Pagliari, M. T. et al. ADAMTS13 activity, high VWF and FVIII levels in the pathogenesis of deep vein thrombosis. Thromb. Res. 197, 132–137 (2021).
Kenagy, R. D., Min, S.-K., Mulvihill, E. & Clowes, A. W. A link between smooth muscle cell death and extracellular matrix degradation during vascular atrophy. J. Vasc. Surg. 54, 182–191.e24 (2011).
Kunimura, K., Uruno, T. & Fukui, Y. DOCK family proteins: key players in immune surveillance mechanisms. Int. Immunol. 32, 5–15 (2020).
Sun, L. et al. Cabin 1, a negative regulator for calcineurin signaling in T lymphocytes. Immunity 8, 703–711 (1998).
Afrache, H., Gouret, P., Ainouche, S., Pontarotti, P. & Olive, D. The butyrophilin (BTN) gene family: from milk fat to the regulation of the immune response. Immunogenetics 64, 781–794 (2012).
Norlander, A. E. et al. A salt-sensing kinase in T lymphocytes, SGK1, drives hypertension and hypertensive end-organ damage. JCI Insight 2, 92801 (2017).
van der Heijden, T., Bot, I. & Kuiper, J. The IL-12 cytokine family in cardiovascular diseases. Cytokine 122, 154188 (2019).
Zhou, W. et al. Global Biobank Meta-analysis Initiative: powering genetic discovery across human diseases. Cell Genomics 2, 100192 (2022).
Klarin, D. et al. Genome-wide association study of peripheral artery disease in the Million Veteran Program. Nat. Med. 25, 1274–1279 (2019).
Xiao, Y., Huang, Z., Yin, H., Lin, Y. & Wang, S. In vitro differences between smooth muscle cells derived from varicose veins and normal veins. J. Vasc. Surg. 50, 1149–1154 (2009).
Finnis, M. L. & Gibson, M. A. Microfibril-associated glycoprotein-1 (MAGP-1) binds to the pepsin-resistant domain of the alpha3(VI) chain of type VI collagen. J. Biol. Chem. 272, 22817–22823 (1997).
Broekelmann, T. J., Bodmer, N. K. & Mecham, R. P. Identification of the growth factor-binding sequence in the extracellular matrix protein MAGP-1. J. Biol. Chem. 295, 2687–2697 (2020).
Buján, J. et al. Expression of elastic components in healthy and varicose veins. World J. Surg. 27, 901–905 (2003).
Barallobre-Barreiro, J. et al. Extracellular matrix remodelling in response to venous hypertension: proteomics of human varicose veins. Cardiovasc. Res. 110, 419–430 (2016).
Werneck, C. C. et al. Mice lacking the extracellular matrix protein MAGP1 display delayed thrombotic occlusion following vessel injury. Blood 111, 4137–4144 (2008).
King, E. A., Davis, J. W. & Degner, J. F. Are drug targets with genetic support twice as likely to be approved? Revised estimates of the impact of genetic support for drug mechanisms on the probability of drug approval. PLoS Genet. 15, e1008489 (2019).
Nelson, M. R. et al. The support of human genetic evidence for approved drug indications. Nat. Genet. 47, 856–860 (2015).
Huffman, J. E. Examining the current standards for genetic discovery and replication in the era of mega-biobanks. Nat. Commun. 9, 5054 (2018).
Sudlow, C. et al. UK Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 12, e1001779 (2015).
Purcell, S. et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am. J. Hum. Genet. 81, 559–575 (2007).
Chang, C. C. et al. Second-generation PLINK: rising to the challenge of larger and richer datasets. Gigascience 4, 7 (2015).
Mbatchou, J. et al. Computationally efficient whole-genome regression for quantitative and binary traits. Nat. Genet. https://doi.org/10.1038/s41588-021-00870-7 (2021).
Zhou, W. et al. Efficiently controlling for case-control imbalance and sample relatedness in large-scale genetic association studies. Nat. Genet. 50, 1335–1341 (2018).
Ani, A., van der Most, P. J., Snieder, H., Vaez, A. & Nolte, I. M. GWASinspector: comprehensive quality control of genome-wide association study results. Bioinformatics 37, 129–130 (2021).
Willer, C. J., Li, Y. & Abecasis, G. R. METAL: fast and efficient meta-analysis of genomewide association scans. Bioinformatics 26, 2190–2191 (2010).
Watanabe, K., Taskesen, E., van Bochoven, A. & Posthuma, D. Functional mapping and annotation of genetic associations with FUMA. Nat. Commun. 8, 1826 (2017).
Bulik-Sullivan, B. et al. An atlas of genetic correlations across human diseases and traits. Nat. Genet. 47, 1236–1241 (2015).
Klarin, D. et al. Genome-wide association analysis of venous thromboembolism identifies new risk loci and genetic overlap with arterial vascular disease. Nat. Genet. 51, 1574–1579 (2019).
de Leeuw, C. A., Mooij, J. M., Heskes, T. & Posthuma, D. MAGMA: generalized gene-set analysis of GWAS data. PLoS Comput. Biol. 11, e1004219 (2015).
GTEx Consortium. Human genomics. The Genotype-Tissue Expression (GTEx) pilot analysis: multitissue gene regulation in humans. Science 348, 648–660 (2015).
Subramanian, A. et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl Acad. Sci. 102, 15545–15550 (2005).
Elsworth, B. et al. The MRC IEU OpenGWAS data infrastructure. https://doi.org/10.1101/2020.08.10.244293 (2020).
Nikpay, M. et al. A comprehensive 1000 Genomes-based genome-wide association meta-analysis of coronary artery disease. Nat. Genet. 47, 1121–1130 (2015).
Klarin, D. et al. Genetic architecture of abdominal aortic aneurysm in the Million Veteran Program. Circulation 142, 1633–1646 (2020).
Malik, R. et al. Multiancestry genome-wide association study of 520,000 subjects identifies 32 loci associated with stroke and stroke subtypes. Nat. Genet. 50, 524–537 (2018).
Bowden, J., Davey Smith, G., Haycock, P. C. & Burgess, S. Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet. Epidemiol. 40, 304–314 (2016).
Lawlor, D. A., Harbord, R. M., Sterne, J. A. C., Timpson, N. & Davey Smith, G. Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat. Med. 27, 1133–1163 (2008).
Mendez, D. et al. ChEMBL: towards direct deposition of bioassay data. Nucleic Acids Res. 47, D930–D940 (2019).
Ay, F., Bailey, T. L. & Noble, W. S. Statistical confidence estimation for Hi-C data reveals regulatory chromatin contacts. Genome Res. 24, 999–1011 (2014).
Kaul, A., Bhattacharyya, S. & Ay, F. Identifying statistically significant chromatin contacts from Hi-C data with FitHiC2. Nat. Protoc. 15, 991–1012 (2020).
Valdeolivas, A. et al. Random walk with restart on multiplex and heterogeneous biological networks. Bioinformatics 35, 497–505 (2019).
Hwang, S. et al. HumanNet v2: human gene networks for disease research. Nucleic Acids Res. 47, D573–D580 (2019).
Szklarczyk, D. et al. STRING v11: protein-protein association networks with increased coverage, supporting functional discovery in genome-wide experimental datasets. Nucleic Acids Res. 47, D607–D613 (2019).
Zhang, Q. et al. hTFtarget: a comprehensive database for regulations of human transcription factors and their targets. Genomics Proteomics Bioinformatics 18, 120–128 (2020).
Cliff, A. et al. A high-performance computing implementation of iterative random forest for the creation of predictive expression networks. Genes 10, E996 (2019).
Basu, S., Kumbier, K., Brown, J. B. & Yu, B. Iterative random forests to discover predictive and stable high-order interactions. Proc. Natl Acad. Sci. USA 115, 1943–1948 (2018).
GTEx Consortium. The GTEx Consortium atlas of genetic regulatory effects across human tissues. Science 369, 1318–1330 (2020).
Acknowledgements
We thank the participants of the VA Million Veteran Program, UK Biobank, eMERGE, FinnGen and BioBank Japan studies. This research is based on data from the Million Veteran Program, Office of Research and Development, Veterans Health Administration, and was supported by an award from the Computational Health Analytics for Medical Precision to Improve Outcomes Now (CHAMPION) initiative to S.M.D., P.S.T. and R.K.M. This publication does not represent the views of the Department of Veteran Affairs or the US Government. M.G.L. is supported by the Institute for Translational Medicine and Therapeutics of the Perelman School of Medicine at the University of Pennsylvania and the NIH/NHLBI National Research Service Award postdoctoral fellowship (grant no. T32HL007843). S.M.D. is supported by the US Department of Veterans Affairs award no. IK2-CX001780. This publication does not represent the views of the Department of Veterans Affairs or the US Government. D.A.J., K.A.S., D.K., M.R.G., M.L., M.C. and J.I.M. are supported by funding from the Million Veteran Program Computational Health Analytics for Medical Precision to Improve Outcomes Now (CHAMPION) initiative and NIH grants no. DA051908 and no. DA051913. eMERGE is supported by grant no. U01HG8657 (University of Washington); grant no. U01HG8685 (Brigham and Women’s Hospital); grant no. U01HG8672 (Vanderbilt University Medical Center); grant no. U01HG8666 (Cincinnati Children’s Hospital Medical Center); grant no. U01HG6379 (Mayo Clinic); grant no. U01HG8679 (Geisinger Clinic); grant no. U01HG8680 (Columbia University Health Sciences); grant no. U01HG8684 (Children’s Hospital of Philadelphia); grant no. U01HG8673 (Northwestern University); grant no. U01HG8701 (Vanderbilt University Medical Center serving as the Coordinating Center); grant no. U01HG8676 (Partners Healthcare/Broad Institute); and grant no. U01HG8664 (Baylor College of Medicine). This research used resources of the Oak Ridge Leadership Computing Facility, which is a DOE Office of Science User Facility supported under Contract no. DE-AC05-00OR22725. This manuscript has been coauthored by UT-Battelle, LLC under contract no. DE-AC05-00OR22725 with the US Department of Energy. The US Government retains, and the publisher, by accepting the article for publication, acknowledges that the US Government retains, a nonexclusive, paid-up, irrevocable, world-wide license to publish or reproduce the published form of this manuscript, or allow others to do so, for US Government purposes. The Department of Energy will provide public access to these results of federally sponsored research in accordance with the DOE Public Access Plan (http://energy.gov/downloads/doe-public-access-plan, last accessed 16 September 2020). E.A.J. is supported by the Building Interdisciplinary Research Careers in Women’s Health (BIRCWH) career development program (grant no. K12HD043483). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
M.G.L., J.E.H., A.V., K.A.S., A.G.B., D.A.J., R.K.M. and S.M.D. designed the study. M.G.L., J.E.H., A.V., K.A.S., A.A.R., D.K., H.W., M.R.G., M.L., M.C. and J.I.M. performed analyses. M.G.L., J.E.H., A.V., A.A.R., A.G.B., R.K.M., P.S.T. and S.M.D. contributed data from MVP. A.V., B.L., Y.L., G.P.J., H.H., E.A.J. and M.D.R. contributed data from eMERGE. M.G.L. drafted the manuscript, and all authors provided critical revisions.
Corresponding author
Ethics declarations
Competing interests
S.M.D. receives research support from RenalytixAI and personal consulting fees from Calico Labs, both outside the scope of the current manuscript. S.M.D. is named as a coinventor on a Government-owned US Patent application (US20210113536A1) related to the use of genetic risk prediction for venous thromboembolic disease filed by the US Department of Veterans Affairs in accordance with Federal regulatory requirements, outside the scope of the current manuscript. S.M.D. is named as a coinventor on a Government-owned US Patent application (US20210285050A1) related to the use of PDE3B inhibition for preventing cardiovascular disease filed by the US Department of Veterans Affairs in accordance with Federal regulatory requirements, outside the scope of the current manuscript. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Cardiovascular Research thanks Dipender Gill and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Effect Size and Minor Allele Frequency for Novel and Previously Reported Risk Loci.
Absolute effect size after fixed-effects meta-analysis plotted as a function of minor allele frequency for all novel genome-wide significant loci (p < 5 × 10−8), and the 30/36 previously reported loci with p < 0.05 in the current meta-analysis.
Extended Data Fig. 2 Ancestry-Specific Heritability Estimates.
LD-score regression was used to estimate ancestry-specific liability-scale heritability, using ancestry-specific LD scores from Pan UK Biobank (https://pan.ukbb.broadinstitute.org/docs/ld). Bars represent 95% confidence intervals (95% CI).
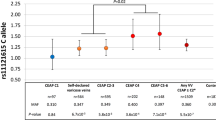
Extended Data Fig. 3 Mediated Effects of Candidate Varicose Vein Risk Loci.
Genomic Structural Equation Modeling was used to estimate the direct and indirect effects of rs62033413 (located near FTO) and rs6025 (Factor V Leiden) on Varicose Veins after accounting for the effects of each variant on BMI and venous thromboembolism (VTE), respectively. Error bars represent 95% Confidence Intervals (95% CI).
Extended Data Fig. 4 MAGMA Tissue and Gene Set Enrichment.
a) Tissue enrichment was assessed using MAGMA via the online FUMA platform, integrating GWAS summary statistics for varicose veins with gene expression (RNAseq) data from GTEx V8. b) Gene set enrichment results from MAGMA. Tissues (panel A) enriched at a false discovery rate threshold of 5% are noted by red bars. Pathways (panel B) enriched at a Bonferroni-adjusted p < 0.05 points are noted by red dots.
Extended Data Fig. 5 Genetic Correlation Between Varicose Veins and Vascular Traits.
Genetic correlations between varicose veins and other vascular traits were estimated using cross-trait LDSC. Varicose veins were significantly correlated with VTE (venous thromboembolism), PAD (peripheral artery disease), and AAA (abdominal aortic aneurysm), but not STROKE (any ischemic stroke) or CAD (coronary artery disease. Error bars represent 95% Confidence Intervals (95% CI).
Extended Data Fig. 6 Multi-Trait Colocalization.
Multi-trait colocalization was performed across all metabolites, proteins, or UK Biobank traits with shared associations with varicose veins at a given locus. Loci are labeled by chromosome, and each locus is denoted by the sentinel variant from the varicose veins GWAS meta-analysis. The size of points corresponds to the number of colocalizing traits.
Extended Data Fig. 7 Random Walk with Restart-based Topological Gene Enrichment of Genome-wide Significant Varicose Veins Variants.
a) Workflow of cell-type specific SNP-to-gene assignment and gene set enrichment analysis. Hi-C contact maps were generated from human umbilical vein endothelial cells (HUVECs) and human coronary artery smooth muscle cells (HCASMCs) and the intersecting H-MAGMA assigned genes from HUVEC and HCASMC Hi-C data sets. b) Varicose veins GWAS genes are more topologically enriched for GO terms related to known cardiovascular processes compared to other GO terms based on random walk with restart (RWR) ranking of genes associated with each GO term. Panel A created using BioRender.com.
Supplementary information
Supplementary Information
Supplementary Methods, Fig. 1, Note and References.
Supplementary Table
Supplementary Tables 1–23.
Rights and permissions
About this article
Cite this article
Levin, M.G., Huffman, J.E., Verma, A. et al. Genetics of varicose veins reveals polygenic architecture and genetic overlap with arterial and venous disease. Nat Cardiovasc Res 2, 44–57 (2023). https://doi.org/10.1038/s44161-022-00196-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44161-022-00196-5