Abstract
Study design:
A prospective cohort with acute tetraplegia.
Objectives:
Obstructive sleep apnoea (OSA) is common within weeks of tetraplegia. This study aimed at determining the feasibility of auto-titrating continuous positive airway pressure (CPAP) to treat OSA after acute tetraplegia.
Setting:
The Victorian Spinal Cord Service, Melbourne, Australia
Methods:
Participants underwent full, portable polysomnography. Those with an apnoea hypopnoea index of more than 10 events per hour were defined as having OSA and were offered treatment with CPAP. Treatment adherence was objectively monitored, and measures of quality of life, sleepiness and functional outcomes were determined at enrolment and 3 months later at study conclusion.
Results:
A total of 44 patients were admitted to our Spinal Cord Service over 9 months, and 19 participated. Fourteen of them had OSA and seven were adherent with therapy for 3 months. Compared with those who did not have OSA, and with those with OSA who were not adherent with CPAP, those who adhered to CPAP were older (mean (s.d.) age 54 years (13) versus non-adherent 28 years (15) and no OSA 29 years (10)) and heavier (body mass index (BMI) 32.5 (11.7), 24.1 (3.7) and 20.6 (3.1), respectively). CPAP-adherant patients and those without OSA showed a 50% or greater improvement in their state sleepiness over the 3 months. Patients with OSA who did not tolerate CPAP had no improvement in sleepiness.
Conclusion:
Auto-titrating CPAP is a feasible treatment for OSA in acute tetraplegia. Intensive clinical support was required initially, and a tolerance of therapy for at least 4 h for one of the first 3 days was predictive of good CPAP usage.
Sponsorship:
Transport Accident Commission.
Similar content being viewed by others
Introduction
Good sleep is an integral component of a healthy and productive life. People living with tetraplegia have a much higher prevalence of sleep disorders than does the general population.1 The most common respiratory sleep disorder in tetraplegia is obstructive sleep apnoea (OSA). The prevalence of OSA in chronic tetraplegia is 2 to 5 times higher2, 3, 4, 5, 6, 7, 8, 9 than that in the general population.10 In acute tetraplegia, OSA is apparent within weeks of initial injury and affects 60–83% of patients in the first year after injury.11
Spinal injuries are predominantly sustained by people in their 20s and 30s, the majority of whom then survive for a further 40 to 60 years.12 Untreated OSA is a significant issue in those with tetraplegia as it is associated with significant neurocognitive deficits,13 sleepiness2, 3, 4, 5, 6, 7, 8, 9, 14 and a reduced quality of life.14 The usual treatment for OSA in the able bodied is nasal continuous positive airway pressure (CPAP); however, CPAP has not been shown to be well tolerated in tetraplegia.
Continuous positive airway pressure corrects sleep hypoxaemia, improves neurocognitive performance15 and nocturnal blood pressure control16 in the able bodied with OSA; however, uncontrolled studies of CPAP treatment in chronic tetraplegia are disappointing. Stockhammer et al.9 found 31 cases of OSA after screening 50 patients with tetraplegia. Only 16 of the 31 had used CPAP in the past, with 11 (35%) continuing to use the device for at least a few weeks. Burns et al.6 undertook a cross-sectional postal survey of patients with tetraplegia whose record indicated diagnosis or treatment for OSA. Only 39% were currently using CPAP and an additional 27% had used CPAP but discontinued therapy because of intolerance. In our earlier acute cohort study,11 five patients with OSA were offered CPAP. Only one of the patients continued with CPAP for more than a few days. The reasons for poor adherence to CPAP have not been systematically examined before, but case series have suggested that nasal congestion, an inability to fall asleep with the mask on and no perceived benefit all contribute.
To determine whether CPAP can be used in acute tetraplegia, we carried out a study of the feasibility and effectiveness of early CPAP treatment for OSA. The secondary aims of the study were to determine the nature and the amount of assistance required to adequately implement CPAP, to determine if any baseline patient characteristics were likely to be predictive of adherence and to obtain preliminary estimates of the effect of treatment on quality of life, sleepiness and its functional outcomes.
Methods
Patient selection
All patients who were admitted to the Victorian Spinal Cord Service during the 9-month period from January 2007 to October 2007 with acute spinal cord lesions above T1 and aged 17–80 years were assessed for study inclusion. Patients were excluded if they had a significant history of cardiac or respiratory disease, an expected length of stay <6 weeks, an initial Glascow Coma Score <8 or a history of severe psychiatric illness.
A detailed medical history was obtained, the likelihood of pre-injury OSA was estimated17 and body mass index (BMI) was recorded at enrolment. All other measures were determined at both baseline and study completion (3 months). Neck circumference, abdominal circumference at end expiration and forced vital capacity (Easy One. NDD Medical Technologies Andover, MA, USA) were measured. These measures were determined with the participant in the supine position and without an abdominal binder.18 The participants completed five questionnaires examining quality of life and sleepiness. The questionnaires measured generic, health-related quality of life and health utility (Assessment of Quality of Life (AQoL),19 the functional outcomes of sleep (FOSQ)20 and current (state) sleepiness on a nine-point scale (Karolinska Sleepiness Scale (KSS)).21 General sleep symptoms were recorded with the Basic Nordic Sleep Questionnaire (BNSQ), a general sleep questionnaire that has been validated in the spinal population.5
Participants underwent an initial overnight diagnostic sleep study using a portable sleep-monitoring device. (Compumedics Somte, Abbottsford, Australia). The measures of the sleep study included central (C4/A1, C3/A2) electroencephalography, bilateral electro-oculography, electromyography (chin, diaphragmatic), electrocardiography, blood oxygen saturation, nasal pressure (airflow), leg movements, body position and respiratory movements of the chest and abdomen. The sleep studies were carried out with the participant sleeping in their hospital bed and commenced at their usual bedtime.
All studies were sleep staged and respiratory scored by an independent, experienced sleep scientist. Sleep was staged in 30-s epochs, arousals marked, respiratory events scored and summary indices calculated according to international standard criteria.22, 23 An apnoea hypopnoea index of >10 events per hour was defined as OSA.
Continuous positive airway pressure implementation
To determine whether it was feasible to use CPAP to treat OSA after acute tetraplegia, we provided a high level of individual support to all patients. CPAP was delivered by an auto-titrating device (Spirit Resmed Autoset, San Diego, CA, USA) fitted with an integrated, heated humidifier. Auto-titrating CPAP devices automatically adjust the level of delivered pressure that is required to ensure upper airway patency.24 Device usage was covertly monitored as ‘time at pressure’ and downloaded weekly.
Patients with OSA were fitted with a CPAP mask by the unit physiotherapist. An attended trial of the equipment was conducted in the afternoon and the same therapist attended that evening at the participant's nominated sleep time, applied the mask and stayed until the patient had either successfully settled or not for that night. Nightly support was maintained until each participant was able to independently direct and troubleshoot the mask application. Night nursing staff provided further, ongoing support.
The number of nights a therapist attended a patient and how long they stayed on each occasion was recorded. The time taken to troubleshoot equipment and debrief the patient in the morning was documented, as was the time spent educating ward staff to support each participant and to use the equipment. A semi-structured interview was conducted with each OSA-positive participant at study completion to examine the subjective experience of trial participation, particularly the experience of using (or attempting to use) CPAP. Participants were classified as adherent with therapy if they used the device for at least 4 h per night on 5 of 7 days25 in the last week of the study when adherence data were recorded.
Results were summarized as mean (s.d.) unless specified. Statistical comparisons between groups were not carried out because of the low number of participants and the absence of randomization in the study. All participants provided witnessed, informed consent, the project was approved by the institutional Human Ethics Research Committee and is registered at http://www.actr.org.au(001261). We certify that all applicable institutional and governmental regulations with regard to the ethical use of human volunteers were followed during the course of this research.
Results
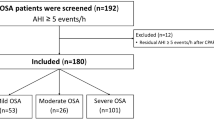
Forty-four patients with new cervical spinal injuries were admitted during the recruitment period and 23 were eligible for study inclusion. Nineteen patients underwent a baseline sleep study. Five recorded an apnoea hypopnoea index of <10 events per hour (OSA negative) and were not offered CPAP. The 14 OSA-positive patients were all offered CPAP and seven (50%) were adherent with therapy (Figure 1). One of the patients who was adherent with therapy was transferred (unexpectedly) overseas after 18 days and no follow-up data were obtained. Two adherent patients were transferred to other rehabilitation units after 56 and 60 days. Follow-up sleep studies and questionnaire data were obtained from these participants; however, objective CPAP adherence data could not be collected in the final month of the trial. These patients and their care givers reported that they remained adherent with CPAP over this period. Nightly CPAP usage for the seven adherent participants was 5.53 (2.1) h. Four of the non-adherent participants had <20 min use on any night. The average usage per night across the non-adherent group was 0.65 (1.0) hours.
Table 1 shows the baseline demographic characteristics of those included in the study. Those with OSA who tolerated CPAP were older, heavier, sleepier and had more severe OSA at baseline than those with OSA who did not tolerate CPAP and those without OSA (Table 2). No adverse events were observed with the auto-titrating CPAP devices, and adherent patients reported a high degree of satisfaction. Figure 2 shows the change in the delivered pressure over time.
Continuous positive airway pressure-adherent patients; time required to successfully implement continuous positive airway pressure therapy
Patient support was provided approximately 3 h per night for three to four nights in the first week of implementation. Approximately 1 h per day was also required during this time to troubleshoot equipment and to debrief the participant (Table 3). A similar amount of time was spent implementing CPAP in the group of patients who were adherent with therapy (16.2 (4.3) h) compared with those who were not (14.0 (6.8)). A variety of patient interfaces were used to achieve optimal patient comfort and adherence. These included Swift Nasal Pillows, Ultramirage masks in varying sizes, Liberty masks (all Resmed, San Diego, CA, USA) and Fisher and Paykel 407 nasal masks (Fisher and Paykel Healthcare, Auckland New Zealand). Chinstraps were used to control mouth leak in two patients who used CPAP.
Characteristics of those who were not adherent with CPAP
One patient refused any trial with CPAP and four patients were unable to tolerate the mask for longer than 20 min at any time. The remaining two participants wore the mask for periods of a few hours overnight. They had no subjective improvement in their sleep, had ongoing, intermittent nasal congestion and abandoned therapy after 4 and 12 weeks (Table 4). All of these patients reported sleeping well without CPAP.
Estimates of the effect of CPAP for OSA in acute quadriplegia
The final aim of this feasibility study was to determine the estimates of the effect of OSA and treatment with CPAP on our study outcome measures (Table 5). The data suggested that state sleepiness may be improved in those with OSA after CPAP treatment. Health-related quality of life and health utility scores are very low after injury and improve three- to fourfold. However, the response is highly variable and does not seem to be greatly affected by either OSA or CPAP treatment. FOSQ improved by a similar amount in all patients.
Discussion
This study replicates the earlier finding of a high prevalence of OSA in people who suffer from an acute cervical spinal cord injury.11 We have shown that it is feasible to screen people with acute tetraplegia for OSA using a comprehensive sleep-monitoring device and to treat those with OSA using auto-titrating, nasal CPAP. Participants who had a more severe disease, who were older, sleepier and larger seemed to be more likely to use CPAP. Intensive clinical support was required for the first 2–5 days of treatment, but if therapy was used for at least 4 h for one of the first 3 days, then treatment was likely to be adhered to for at least 3 months. This pattern of adherence to CPAP therapy is very similar to that observed in the able-bodied population,26 where early acceptance of therapy is a strong predictor of ongoing use.
Seven patients who had OSA were unable to tolerate CPAP. Although all nonadherent patients reported sleeping well without CPAP, this group showed no improvement in sleepiness over the 3-month trial, whereas those without OSA and those with OSA who were treated had a 50% or greater improvement in state sleepiness. The FOSQ did not seem to be substantially affected by the use of CPAP; it seemed to improve in a similar manner in all, regardless of both OSA and CPAP, and thus may not be a sensitive instrument in this population.
The quality of life data showed extremely low baseline health utility scores. A health utility score of 0.1, as shown by the group as a whole at baseline, implied that the participants were willing to trade 9 years of life in their current health state for 1 year of good (perfect) health. Such a perceived health state is perhaps understandable after catastrophic trauma; however, this is, to the best of our knowledge, the first description of health status in acute tetraplegia and is strikingly low. All groups improved health status during the trial over time; however, the response was highly variable. When the individual elements of AQoL were examined in detail, there is a suggestion that those patients who were better able to reconcile their ‘new’ physical state with an ongoing role in society and their family scored better. Similarly, there was a suggestion that those who had a reduction in sleepiness also had an improvement in health utility. These observations are noteworthy; however, with such a small study sample and a non-randomized trial design, these results warrant replication in a larger, controlled study.
A secondary aim of this study was to identify the nature and amount of assistance required to adequately implement CPAP in this patient population. To achieve a success rate of 50% adherence, we utilized the skills of an experienced physiotherapist trained in the care of patients with acute spinal injuries with a knowledge of noninvasive ventilation. Most of the time was spent on mask selection and donning. The next most time-consuming activity was dealing with nasal congestion, which required only half the time of mask donning and selection. Nasal congestion was an issue for most of those who abandoned therapy (Table 4), and more aggressive management with, for example, anti-cholinergic nasal therapy may have increased adherence further. Patients reported that the debrief time was valuable in order to understand the correct function of CPAP, and to interpret variable flow levels at different stages at night. Modifications to the humidifier temperature to correct for nasal dryness or condensate in the circuit were required by 9 of 14 patients. Adherent patients gained confidence quickly over the first week of treatment and became skilled in troubleshooting their own equipment and in instructing ward staff in the application of the mask.
The adherence rate of 50% in this study may be regarded as being close to the best possible achievable in routine clinical care and we believe that it was facilitated by a number of practices. We provided intensive support with highly skilled staff and a wide range of patient interfaces. We further suggest that the auto-titrating CPAP device may have enhanced adherence by adapting to changes in individual patient's pressure requirements over time (Figure 2). Had a fixed-pressure CPAP been used, the initial pressure would have been incorrect over time in all but one patient, and too much or too little pressure may have been expected to reduce usage. The observed degree of within-patient pressure change is substantially higher than that observed in the able-bodied population,27 and was unexpected. Further research examining the pressure and resistance characteristics of the upper airway and how they change over time in acute tetraplegia is required to understand these findings.
This research has shown that it is feasible to screen people with acute tetraplegia for OSA and to deliver treatment using auto-titrating, nasal CPAP. This finding, along with the suggestion of differences in patient characteristics between those without OSA and those who were adherent with therapy, provides a rationale for further prospective, randomized controlled trials of CPAP for OSA in acute tetraplegia.
References
Biering-Sorensen F, Biering-Sorensen M . Sleep disturbances in the spinal cord injured: an epidemiological questionnaire investigation, including a normal population. Spinal Cord 2001; 39: 505–513.
Leduc BE, Dagher JH, Mayer P, Bellemare F, Lepage Y . Estimated prevalence of obstructive sleep apnea-hypopnea syndrome after cervical cord injury. Arch Phys Med Rehabil 2007; 88: 333–337.
Short DJ, Stradling JR, Williams SJ . Prevalence of sleep apnoea in patients over 40 years of age with spinal cord lesions. J Neurol Neurosurg Psychiatry 1992; 55: 1032–1036.
McEvoy RD, Mykytyn I, Sajkov D, Flavell H, Marshall R, Antic R et al. Sleep apnoea in patients with quadriplegia. Thorax 1995; 50: 613–619.
Biering-Sorensen F, Biering-Sorensen M, Hilden J . Reproducibility of Nordic Sleep Questionnaire in spinal cord injured. Paraplegia 1994; 32: 780–786.
Burns SP, Little JW, Hussey JD, Lyman P, Lakshminarayanan S . Sleep apnea syndrome in chronic spinal cord injury: associated factors and treatment. Arch Phys Med Rehabil 2000; 81: 1334–1339.
Levi R, Hultling C, Nash MS, Seiger A . The Stockholm spinal cord injury study: 1. Medical problems in a regional SCI population. Paraplegia 1995; 33: 308–315.
Star AM, Osterman AL . Sleep apnea syndrome after spinal cord injury. Report of a case and literature review. Spine 1988; 13: 116–117.
Stockhammer E, Tobon A, Michel F, Eser P, Scheuler W, Bauer W et al. Characteristics of sleep apnea syndrome in tetraplegic patients. Spinal Cord 2002; 40: 286–294.
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S . The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 1993; 328: 1230–1235.
Berlowitz DJ, Brown DJ, Campbell DA, Pierce RJ . A longitudinal evaluation of sleep and breathing in the first year after cervical spinal cord injury. Arch Phys Med Rehabil 2005; 86: 1193–1199.
Cripps RA . Spinal Cord Injury, Australia 2005–06. Australian Institute of Health and Welfare: Canberra, 2007 November 2007, Contract No.: 10.
Sajkov D, Marshall R, Walker P, Mykytyn I, McEvoy RD, Wale J et al. Sleep apnoea related hypoxia is associated with cognitive disturbances in patients with tetraplegia. Spinal Cord 1998; 36: 231–239.
Spong J, Riley D, Ross J, Pierce RJ, Brown DJ, Berlowitz DJ . Sleep health in tetraplegia—A Victorian population survey. Respirology 2008; 13 (S2): A73.
Kingshott RN, Vennelle M, Hoy CJ, Engleman HM, Deary IJ, Douglas NJ . Predictors of improvements in daytime function outcomes with CPAP therapy. Am J Respir Crit Care Med 2000; 161 (3 Pt 1): 866–871.
Barnes M, Houston D, Worsnop CJ, Neill AM, Mykytyn IJ, Kay A et al. A randomized controlled trial of continuous positive airway pressure in mild obstructive sleep apnea. Am J Respir Crit Care Med 2002; 165: 773–780.
Maislin G, Pack AI, Kribbs NB, Smith PL, Schwartz AR, Kline LR et al. A survey screen for prediction of apnea. Sleep 1995; 18: 158–166.
Kelley A, Garshick E, Gross ER, Lieberman SL, Tun CG, Brown R . Spirometry testing standards in spinal cord injury. Chest 2003; 123: 725–730.
Hawthorne G, Richardson J, Osborne R . The Assessment of Quality of Life (AQoL) instrument: a psychometric measure of health-related quality of life. Qual Life Res 1999; 8: 209–224.
Weaver TE, Laizner AM, Evans LK, Maislin G, Chugh DK, Lyon K et al. An instrument to measure functional status outcomes for disorders of excessive sleepiness. Sleep 1997; 20: 835–843.
Gillberg M, Kecklund G, Akerstedt T . Relations between performance and subjective ratings of sleepiness during a night awake. Sleep 1994; 17: 236–241.
Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep 1999; 22: 667–689.
Rechtschaffen A, Kales A . A Manual of Standardized Terminology, Techniques and Scoring System for Sleep Stages in Human Subjects. National Institutes of Health: Washington DC, 1968.
Massie CA, McArdle N, Hart RW, Schmidt-Nowara WW, Lankford A, Hudgel DW et al. Comparison between automatic and fixed positive airway pressure therapy in the home. Am J Respir Crit Care Med 2003; 167: 20–23.
Kribbs NB, Pack AI, Kline LR, Smith PL, Schwartz AR, Schubert NM et al. Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. American Review of Respiratory Disease 1993; 147: 887–895.
Budhiraja R, Parthasarathy S, Drake CL, Roth T, Sharief L, Budhiraja P et al. Early CPAP use identifies subsequent adherence to CPAP therapy. Sleep 2007; 30: 320–324.
Bachour A, Virkkala JT, Maasilta PK . AutoCPAP initiation at home: Optimal trial duration and cost-effectiveness. Sleep Medicine 2007; 8: 704–710.
Acknowledgements
We acknowledge the generous support of the participants, their families and the Victorian Spinal Cord Service staff. This project was proudly supported by the Transport Accident Commission.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Berlowitz, D., Spong, J., Pierce, R. et al. The feasibility of using auto-titrating continuous positive airway pressure to treat obstructive sleep apnoea after acute tetraplegia. Spinal Cord 47, 868–873 (2009). https://doi.org/10.1038/sc.2009.56
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.56
Keywords
This article is cited by
-
Prevalence of sleep-disordered breathing in people with tetraplegia—a systematic review and meta-analysis
Spinal Cord (2021)
-
A randomised controlled trial of nasal decongestant to treat obstructive sleep apnoea in people with cervical spinal cord injury
Spinal Cord (2019)
-
Positive airway pressure therapy for sleep-disordered breathing confers short-term benefits to patients with spinal cord injury despite widely ranging patterns of use
Spinal Cord (2018)
-
Auto-titrating continuous positive airway pressure treatment for obstructive sleep apnoea after acute quadriplegia (COSAQ): study protocol for a randomized controlled trial
Trials (2013)
-
Continuous positive airway pressure requirements in patients with tetraplegia and obstructive sleep apnoea
Spinal Cord (2012)