Key Points
-
The dental profession is moving away from a cavity-orientated surgical approach for managing dental caries.
-
This paper presents a summary of the application of child-friendly Minimum Intervention Dentistry (MID) for managing dental caries and carious lesions in primary teeth.
-
The five key principles covered are Recognition, Re-orientation, Remineralisation, Repair and Review.
-
Alongside early detection and less invasive methods for managing carious lesions for children, patient self-care is a core goal of dental care.
Abstract
Child-friendly minimum intervention dentistry (MID) dominates modern thinking and practice around delivery of oral care for children. It is an enormous challenge for our profession to move away from the narrow focus of a mechanistic, cavity-orientated surgical approach for managing dental caries to one which embraces new strategies for caries prevention and management, delivered in the context of a partnership with children, families and other adults involved in the child's life environment. It is also time for a shift in the orientation of dentistry towards 'patient self-care' becoming a core goal of dental care, where dentists help their patients assume responsibility for achieving and maintaining their own oral health, and that of their children. Holistic care, which improves oral health and maximises ability to maintain oral health, should be regarded with the same importance and rewarded with a similar level of remuneration as 'traditional operative dentistry'. This paper gives an overview of a model of care involving the principles of this new approach, and the application of MID in clinical practice for primary teeth.
Similar content being viewed by others
Main
Recognition is not limited to the detection and diagnosis of disease, but incorporates an in-depth oral health assessment, including an appraisal of how lifestyle factors (especially diet) contribute to health and disease, while Re-orientation involves working with the child and family to reinforce or alter these factors, supporting future oral health. Remineralisation aims to arrest or reverse mineral loss in lesions at all disease stages, reducing damage and allowing for Repair of lost tooth substance where the damage is non-cleansable and the lesion is likely to progress. Finally, Review ensures the optimal management choices have been selected for long-term maintenance of oral health.
It is an enormous challenge for our profession to move away from the narrow focus of a mechanistic, cavity-orientated surgical approach for managing dental caries to one which embraces new strategies for caries prevention and management, delivered in the context of a partnership with children, families and other adults involved in the child's life environment.
It is also time for a shift in the orientation of dentistry towards 'patient self-care' becoming a core goal of dental care, where dentists help their patients assume responsibility for achieving and maintaining their own oral health, and that of their children. Inter-personal, psychosocial and coaching skills are no less technical and certainly no easier to establish and refine than the surgical skills learnt in the operative techniques laboratory and, like surgical skills, will be honed over many years of clinical practice. Holistic care, which improves oral health and maximises ability to maintain oral health, should be regarded with the same importance and rewarded with a similar level of remuneration as 'traditional operative dentistry'.
This paper gives an overview of a model of care involving the principles of this new approach, and the application of MID in clinical practice for primary teeth.
Background
Children have the same rights to general and oral health as adults.1 Although the general philosophy behind minimal intervention dentistry (MID) is similar for adults and children, the specific approaches and techniques for children are not always the same, as children are fundamentally different from adults.2,3 Children cannot look after their own oral health for a significant part of their childhood, being entirely dependent on adults for their diet and tooth brushing. They need to be brought for dental appointments, and they like operative care even less than adults. Children tend to live in the present, and tolerating operative dental interventions for an unperceived future gain has little attraction for them. Children also require specific behaviour management techniques. As well as children being cognitively different from adults and holding a distinct place in society, their primary and permanent dentitions are structurally and morphologically different; crucially, primary teeth have a limited lifespan, and exfoliate. A final key difference is that adult dental disease begins in childhood, so long term maintenance of oral health through education and support have to be a core management feature. As the majority of oral disease experienced by children is dental caries, this overview will focus on MID for caries prevention and management.
Oral diseases are the fourth most expensive human disease to treat.4 Current annual EU27 spending of €79 billion is predicted to reach €93 billion by 2020; with 5-10% of public health expenditure relating to oral health.5 Globally, there is an increase in the burden of oral disease, especially in countries with emerging economies.6,7
Despite reductions in the levels of oral disease reported in national surveys, in the UK there remains a significant proportion of children with dental caries. In the latest surveys, 40% of 5-year-olds in England, Wales and Northern Ireland6 and 32% in Scotland, had obvious caries experience.8 For 12-year-olds in Scotland this was 25%.9 Improvements in caries experience over time, however, hide the fact that those with the disease have multiple carious lesions and there continues to be a significant minority of children who carry the majority of the burden of disease.6,9 Additionally, the rate of improvement in the past decade has slowed, and there continues to be a need for community and practice-based preventive strategies targeted at individual disease risk, as well as an ongoing need for high quality dental caries management for children.7
Dental caries causes pain and infection. The disease has a negative impact on children's psychological, social and functional wellbeing, impacting considerably on family life.10,11 It is theoretically an entirely preventable lifestyle disease and is increasingly concentrated in certain high-risk groups, who share common risk factors for general health and disease development.10,12 However, despite technological advances in dental and oral health, there is little evidence that this has translated to improvements in the overall dental health of all children, with continuing disparities in disease levels. The socio-economic and geographical gradient of the disease, within and between societies, presents a complex background on which to try to make improvements. However, there is evidence that simpler interventions to those traditionally used for managing caries are more effective, cheaper and preferred by children.12,13
Minimum intervention dentistry
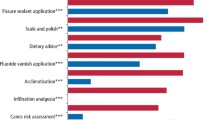
Minimum intervention dentistry (MID) has been discussed as a particular concept since the early 1990s and has evolved to a comprehensive and person-centred philosophy of managing the disease.13 It is a response to the ineffectiveness of the traditional surgically-focused approach to managing dental caries. However, the principles of MID for managing dental caries are built on foundations established in the 1970s.14,15,16,17 Its core principles, adapted and expanded from Walsh et al. 201316 (Fig. 1) can be summarised as: Recognition (of disease contributory factors); Re-orientation (of contributory lifestyle factors); Remineralisation (of all lesions – visible and not visible, cavitated and non-cavitated); Repair (where no other solution is possible) and Review (of the child, their oral health and their life environment).
Applying the core principles of minimum intervention dentistry to children with dental caries16
In this paper an MID approach to the prevention and management of dental caries in children will be discussed, including practical, evidence-based advice on how a modern dental professional should approach the problem of managing dental caries at the level of the child and family. It is outside the scope of this paper to give detailed and comprehensive guidance on every aspect of the implementation of an MID approach; instead, those aspects of the approach which might not currently be part of clinical practice will be outlined, and references given for where further information might be found. The paper follows the main UK-based clinical guidelines around prevention and management of dental caries.18,19,20
Recognition (of contributory factors); including oral health assessment
Child and family
The success of the clinical oral care provided for children stands or falls on a thorough and valid assessment of the child's individual situation (their living/life environment) and the other people involved, including acknowledgement of the link between parental and child oral health and caries risk.21 A full Oral Health Assessment is demanding, and requires skill, persistence, expertise and excellent inter-personal skills of the highest standards. The effort involved will be well-rewarded by providing the information needed for high quality care, both short and long-term. The traditional phrase 'check-up' does not do justice to the key role this stage plays in laying the foundations for truly effective oral health care. It is acknowledged that the remuneration system and availability of different treatment options will also have an influence on the delivery of care.
Social history
A social history is gathered to assess child and family lifestyle factors that contribute to dental caries risk. Several adults may have regular, significant involvement in a child's care, particularly if the parents work, and for some children, their 'care network' can be extensive, and include immediate and extended family and friends, as well as child minders, school clubs and nurseries. All the relevant individuals need to be identified, and their level of involvement recorded in the child's clinical records. The Oral Health Care team (OHC team) should then work with those attending with the child, to ensure effective transfer of knowledge and understanding about the preventive programme – essential to making sure the necessary changes take place to prevent further disease. In addition (and a significantly more difficult task), the OHC team must ensure that the individual adults in the child's care-network also accept their own personal responsibility for the child's oral health. It is particularly important to identify and target any adults who provide regular overnight care for a child, due to the major contribution to the caries burden of nocturnal on-demand bottle feeding and to caries prevention provided by effective 'before-bed' tooth-brushing with a fluoridated paste. Factors such as whether the child was breast-fed, the educational level of the mother, whether the parents are employed, the oral health status of the primary care-giver and whether they smoke or not can have a considerable association with the risk of developing early childhood caries in the child.21 This information can be obtained at the oral health assessment appointment and starts to give insight into some of the barriers to addressing issues later, for example, difficulties with attending appointments.
Dental history
To obtain a reliable history, use open questions, exploring the range of issues and concerns to be addressed, and consider the possible barriers to doing so. The key areas to be investigated must include frequency of dietary sugar intake and toothbrushing habits, both evidence-based critical factors in determining the child's oral health status. Assessing each of 'knowledge', 'skills' and 'attitude' (Fig. 2) for all oral health-related behaviours will inform the approach needed.
Some areas to be explored
-
Brushing practice: how often? When? By whom? Fluoride concentration of toothpaste? Amount applied? Spits out, or rinses?
-
Knowledge – ask the parent/carer or in the case of an older child, the child, to tell you what they know already about tooth-brushing and why they do it. Can they identify that brushing should take place twice-a-day with fluoridated toothpaste of at least 1,000 ppm F; that the child should spit out and not rinse and that there should be nothing to eat or drink after that for 30 minutes
-
Skills – watching the parent/carer brush the child's teeth, or if the child is older, asking them to show you how they brush their teeth, can be very informative in identifying problems with technique (Fig. 3)
Figure 3: (A) Maxillary anterior teeth before cleaning with plaque distributed across teeth; (B) After disclosure the full extent of the plaque (more recent in pink and more mature in blue/purple) can be seen. (C) The child (or for the younger child, the parent/carer) is observed for ability to remove plaque (Skills assessment – see Fig. 2) and to give hints and tips on how to be more effective. (D) After brushing, the lateral incisors are not cleaned effectively so again, it is possible to direct the patient or ask the parent/carer to assist. Note also, that it is only after removal of plaque that a full assessment for dental caries, before cavitation, can be made. (Images courtesy of Dr Patrick Rouas, Bordeaux, France)
-
Attitude towards, and previous experience of, dental care
-
Anxiety levels towards dentistry (and in general), and causes of anxiety.
Medical history
Medical history can influence the treatment planning for the child's oral health care. For example, medical complications due to cardiac disease or a compromised immune system need to be taken into account when considering appropriate options for carious lesions. Underpinning this is the imperative that for these children, caries experience is minimised, and pulpal involvement avoided. This often means intensive prevention of carious lesions and carefully considered management of teeth with lesions that are adjacent to the pulp – often extraction is the safest and most appropriate treatment. If you feel uncertain of the appropriate care options for medically-compromised children, then refer for specialist care.
Behavioural history
Children often require behavioural support and this can be a challenge for both the child and the clinician. Fortunately, there are many straightforward techniques that allow most dental care to be successfully provided.2,22
The two steps that will ensure success on almost all occasions with most patients (children and adults) are:
-
Gaining rapport with the patient. If you gain eye contact with the patient, and communicate in such a way as to receive a positive response, such as a smile, then you are well on the way to establishing effective rapport. Be aware that rapport can go both up and down during an appointment!
-
Giving control to the patient. This process is often misunderstood by clinicians. Saying 'let me know if there are any problems!' just before you use the handpiece is not giving the patient control. Agreeing a signal 'raise your hand if you want me to stop', and then rehearsing it, is much more powerful. If a patient signals for you to stop (and for a child this will include vocalising, or crying), then you must stop immediately. To do otherwise is outside of patient consent, and you and other clinicians in the future will have to pick up the pieces of a patient with serious mistrust issues.
Techniques that work well alongside gaining rapport and giving control include: relaxation (breathing exercises with imagery/tense and relax), tell-show-do, reinforcement with reward, modelling, desensitisation and hypnosis. Relative analgesic techniques such as inhalation of nitrous oxide/oxygen are also very successful and safe in the hands of appropriately trained clinicians.2
Diagnosis of carious lesions
As dental professionals, we diagnose the presence or absence of dental caries as part of our daily clinical practice. However, there is now extensive research that carious lesions can arrest and remineralise. Caries detection and diagnosis is, therefore, no longer simply a binary decision of: 'is caries present? Or absent?' It is essential that, as well as diagnosing the presence of lesions; both cavitated and non-cavitated, it is also necessary to assess whether the lesion is active, arrested, and, if active, how it might be arrested. For active lesions in the primary dentition, a further assessment has to be made of the risk of that lesion causing pain or infection before exfoliation. As part of this process, the extent and activity of lesions needs to be recorded at each assessment. Without this information being available over time, it is difficult for the practitioner to assess the effectiveness of any caries management programme. The usual manner of marking treatment needs on a chart does not allow for this, and it is up to the individual practitioner to find a system that lets extent and activity of lesions be recorded.
To examine for the presence of carious lesions, ensure the teeth are clean and dry. Radiographs help with decision-making (Figs 4, 5) and should be taken in line with recommended guidelines. Treatment possibilities for each lesion depend on lesion stage and activity. So, diagnosis consists of deciding, for each surface of a tooth:
-
Lesion present – yes/no
-
Lesion stage – initial/moderate (risk of irreversible pulpal disease low)/advanced (risk of irreversible pulpal disease high)
-
Lesion activity – active/arrested (soft/hard for dentine and rough/smooth for enamel)
-
For primary teeth, what is the risk of the lesion causing pain/sepsis before the tooth exfoliates.
(B) Radiograph of the same child, taken at the same time revealing the extent of the carious lesions. Tooth 74 has a moderate distal carious lesion extending into the middle 1/3 of dentine and tooth 75 has a moderate mesial carious lesion extending into the outer 1/3 of dentine. A 'clear band of dentine' is visible between the advancing edge of the lesion and the dental pulp for both teeth, and fitting Hall crowns at this stage has a high chance of success.
This tooth should be extracted. The mandibular second primary molar (tooth 75) has an advanced carious lesion on the mesial surface, and no clear band of dentine visiblew between the lesion and the dental pulp. This tooth should have appropriate pulp therapy before being crowned with a preformed metal crown
This information then leads to a judgement about whether a preventive and restorative approach is needed or a xapreventive alone strategy is sufficient.
Recognition
Summary of actions
Use open questions to find out detailed information on:
-
Who spends time looking after the child
-
Toothbrushing habits – assess knowledge, skills and attitude
-
Dietary sugar intake – frequency and timing.To build confidence always:
-
Gain rapport with the child/family
-
Give control when providing treatment.
Caries detection/diagnosis:
-
Not just lesion present – yes/ no, but also:
-
Lesion stage – initial/moderate/advanced
-
Lesion activity – active/arrested
-
For primary teeth, what risk of pain/sepsis before exfoliation?
Re-orientation (of lifestyle factors)
A thorough oral health assessment will have highlighted any caries risk factors to be addressed. The effectiveness of the most important caries preventive interventions we have at our disposal, toothbrushing and controlling the frequency of dietary sugars, will almost totally depend on the parent/carers for their implementation and, therefore, the ability of the OHC team to encourage long term behaviour change in the parent/carers as well as the child. For many children the first dental visit is because they've kept the parents up all night with toothache, so the importance of regular dental care also needs to be encouraged.
Behaviour change
While knowledge is necessary, it is not sufficient to support behaviour change. Simply giving patients information, however intensely and earnestly, is unlikely to change behaviour, possibly because as adults we are generally happy with our behaviour (or at least have rationalised it to our own satisfaction!), and to respond to a request to change implies criticism of ourselves, and loss of our autonomy.2 There are few things more difficult than trying to change someone's behaviour – our role isn't to change it but to support someone to change their own behaviour, and this will only happen if the need to change is accepted and seen as possible by the patient.
Re-orientation
Summary of actions
The oral health assessment may have identified a number of areas where behaviour change techniques might be useful – commonly:
-
Improving tooth-brushing habits
-
Improving dietary sugar intake
-
Improving attendance.
Achieving behaviour change
Simply giving people information and then telling them to follow it DOES NOT WORK! You waste your time and theirs.
You must use specific health behaviour change models to have a chance of changing behaviours. The models that seem to have the greatest supporting evidence supporting their effectiveness are motivational interviewing (Fig. 6) and coaching.
Changing a parent/carer's beliefs and behaviour regarding their child's oral health care is a key step, arguably the single most important step, in managing the oral health of children with active dental caries, particularly in encouraging compliance with tooth-brushing advice and dietary advice.23 It could also be used to encourage completion of a course of treatment, reduce failed appointments, and improve compliance with recall appointments. The use of specific health behaviour change models gives more chance of changing behaviours.24 There are many models; however, the ones that seem to have the greatest supporting evidence supporting their effectiveness are motivational interviewing (Fig. 6) and coaching.25,26
Remineralisation (of all lesions – not just early stage ones)
With a normal diet, superficial enamel is constantly demineralising and remineralising. Dental caries occurs when the rate of demineralisation exceeds that of remineralisation. The OHC team needs to tip the balance back in favour of remineralisation. Our two main tools for achieving this are encouraging best toothbrushing practice with an appropriately fluoridated paste, and reducing the frequency of dietary sugar intake each day. Topical application of fluorides by the OHC team also helps. If a carious lesion has occurred, then the balance can be tipped in favour of remineralisation by the above actions, and also by managing the cariogenic plaque biofilm, either topically, or by sealing-in. Methods for doing this are covered in the next section.
As a profession, standard management of carious lesions has been excision of the lesion and restorative replacement of the lost tooth substance.27 However, progression of lesions, both pre-cavitation and post-cavitation, can be arrested. Carious lesions progress at a slow rate (in most cases), albeit slightly faster in primary than permanent teeth. Regardless of rate of progression, lesions that are confined to enamel which have not cavitated should not be managed restoratively – either in primary or permanent teeth. While the enamel surface layer remains intact, remineralisation is possible even if the lesion extends into dentine.28
Remineralisation
Summary of actions
Toothbrushing
Parent/carers should ensure that:
-
Children have their teeth brushed twice daily: once in the morning, and last thing before going to bed at night
-
0-3 years old: using a smear of 1000 ppm fluoride paste
-
3 years and older: a pea sized amount of 1,450ppm fluoride paste
-
Spitting out, not rinsing, after brushing
-
'Nuthin' after brushin' at night.
Diet advice
-
Sugar in food and drinks should be restricted to four occasions a day18,19,20
-
Only drink water or milk between meals.
Additional caries preventive measures
The oral health care team also needs to ensure that fissure sealants and topical fluorides are used in line with local guidance.
Repair (where no other solution is possible) to manage carious lesions in primary teeth
Effective treatment planning for the child with dental caries is complex and complicated, as many factors feed into the decision-making process. As such, it is not possible to give clear guidance on the best management option for every clinical situation. Instead, an overview of current thinking will be presented, along with the evidence base for it, to provide a framework for the clinician to formulate their own decision-making. Central to everything, though, is that effective management of carious lesions relies on effective prevention to be in place for success, or it is as futile as trying to place 'new windows in a burning building'.27
Recent advances in cariology
Traditionally, carious tooth tissue has been managed almost as if it were gangrene, with complete excision. Now there is overwhelming evidence that the carious process is driven by the plaque biofilm, and if the biofilm can be effectively managed, then the carious lesion will arrest.29,30 The potential advantages of reducing operative management to the patient, and dentists, in terms of reduced risk of iatrogenic pulpal damage and needless loss of irreplaceable tooth tissue, are significant. Broadly, there are two separate approaches to managing the plaque biofilm in carious primary teeth: topically, where the plaque biofilm is left open to the oral environment, but managed, and the sealing-in approach, where the tooth surface at risk is isolated from the oral environment. These approaches, and how they are applied clinically, are discussed in the next section.
The choice of the optimal biofilm management strategy for a carious lesion in a primary tooth will depend on four main factors:
-
Lesion related factors – is it active or arrested? What stage has it reached (initial/moderate/advanced)? Is it likely to cause pain/sepsis before the tooth naturally exfoliates, and if yes, is the risk imminent or in the future?
-
Clinician related factors – how up-to-date is the clinician regarding the evidence base for new techniques? How confident is the clinician in providing some aspects of care, such as pulpotomies, Hall crowns, or resin infiltration? Are preformed metal crowns, or silver diammine fluoride available within the practice? Does the remuneration system allow the clinician to provide the full range of treatment options?
-
Child-related factors – what are the child's wishes regarding management of the lesion? How likely are they to cope with different management options? Are there medical complications? If multiple active lesions are present, along with pain/sepsis, might the child benefit from referral to a specialist centre for consideration of extractions with GA?
-
Family related factors – what is the anticipated compliance with prevention-based strategies for lesion management? If multiple appointments are required, what is the likely compliance with attendance?
The information on which to base these decisions, and so arrive at a treatment plan that is likely to be effective, will only be obtained from a thorough oral health assessment (Recognition stage, as above).
The treatment leading to least damage should always be provided.27 It is now accepted that if iatrogenic exposure of a dental pulp which is either healthy or only has symptoms of a reversible pulpitis occurs, then the clinician has caused unnecessary damage to the tooth and failed to use minimum intervention strategies or apply enough care.
The guiding principles for lesion management (for both the primary and permanent dentition) can be summarised as being to:30
-
'Preserve non-demineralised ...[tooth] tissue;
-
Achieve an adequate restorative seal by placing the peripheral restoration onto sound dentine and/or enamel, thus controlling the lesion and inactivating remaining bacteria;
-
Avoid discomfort/pain and dental anxiety (...)
-
Maintain pulpal health by preserving residual dentine (avoiding unnecessary pulpal irritation/insult) and preventing pulp exposure (...)
-
Maximise longevity of the restoration by removing enough soft dentine to place a durable restoration of sufficient bulk and resilience.'
Diagnosing the stage and activity of carious lesions in primary teeth
There is no single agreed classification for lesion staging although a number are available, for example the International Caries Detection, Assessment and Classification System and the Nyvad System.31,32,33 However, any system that is used for clinical purposes has to allow for the diagnosis to be clinically relevant and relate to treatment decision making. In this paper we will classify the lesion stage as follows:
-
Initial – may be non cavitated, with no dentine involvement, or limited to the outer 1/3rd dentine. Risk of irreversible pulpal disease extremely low
-
Moderate – lesion extends to the middle 1/3rd of dentine, and radiographically a clear band of dentine of normal radiodensity separates the lesion from the dental pulp. Risk of irreversible pulpal disease low
-
Advanced – the lesion involves the inner 1/3rd of dentine, and radiographically encroaches on the pulp. Risk of irreversible pulpal disease high.
Assessing lesion activity is currently an inexact science, but there are accepted signs to aid decision making. An active enamel lesion will feel slightly rough to a steel instrument drawn gently over the surface, while an arrested enamel lesion will feel smooth. Active dentinal caries will feel soft; arresting dental caries feels harder and is drier, while arrested dentinal caries will be hard. Colour is not a reliable indicator for caries activity. The gold standard diagnostic test for an arrested lesion is that it does not progress over time. An accurate charting system can help with this assessment, and radiography (in line with guidelines) and standardised photography is very useful.
Diagnosing and managing pulpal disease in carious primary teeth
The reliable diagnosis of the presence of disease in a primary pulp is problematic, as all the diagnostic methods are indirect, relying on proxy indicators. The following points should be noted:
-
The absence of symptoms does not mean the absence of disease
-
Primary teeth dental pulps have an excellent blood supply and therefore a good reparative potential; teeth with reversible pulpitis (vital pulp; pain only on thermal stimuli; pain resolves on removal of stimuli), should initially be managed with a cavity dressing/restoration, and reviewed
-
Primary molar teeth with irreversible pulpitis (vital pulp, but spontaneous pain or pain with thermal stimuli which doesn't resolve on removal of stimuli) can be managed with either extraction or a pulpotomy
-
Current thinking is that it is unacceptable to leave dental infection/sepsis associated with carious primary teeth unmanaged, even if it is not causing the child pain. This is detected through careful examination to ensure no sinuses are present and radiographs to look for peri-radicular and peri-apical pathology. Affected teeth should be extracted, or (very exceptionally, and only if restorable), referred to a specialist for pulpectomy.
Management options for vital carious primary teeth with initial and moderate lesions
Arrested lesions
If a lesion is not active (that is, can be considered arrested) consider whether the carious lesion actually needs restorative management. Similarly, if the lesion is active, but the tooth likely to shed within 6-12 months, consider whether a restoration is indicated. Unlike permanent teeth, restorative management of carious lesions in primary teeth may not always provide a health benefit for the child.
Active lesions
The focus of management is changing the plaque biofilm from a cariogenic state into a non-cariogenic state. There are two main strategies for achieving this: topically, and by sealing-in.
Topical management strategies for the cariogenic biofilm
The plaque biofilm is left open to the oral environment, but is managed in such a way that it changes to a healthy state, using the following strategies:
-
Encouraging daily disruption and removal of the plaque biofilm through effective tooth brushing. This may be achieved through education alone, or it may also require cavity shaping and opening up and application of fluoride (sometimes called Non-Restorative Cavity Control).34 Until recently, anecdotal evidence has indicated this approach may be successful for managing carious anterior primary teeth. However, two recent studies call the effectiveness of the option into question because of the important role of the parent in changing their behaviour to prevent progression of the lesion35,36,37,38
-
Application of topical fluorides. These can include fluoride from an appropriately fluoridated tooth paste,39 or topical agents applied by the oral health team, such as fluoride varnish.40,41 Silver Diammine Fluoride (SDF) is a topical agent that has recently become available in the UK for application by clinicians, and it has a growing evidence base supporting its effectiveness. Further information on its use is available42,43
-
Reducing the frequency of dietary sugars to less than four times a day is also effective in changing the plaque biofilm to a healthy state.44
It should be noted that, with the possible exception of Silver Diammine Fluoride application, all the topical strategies rely very heavily on child and parent compliance with preventive advice regarding brushing and diet and reapplication of the fluoride product. While their lack of invasiveness is attractive for the child and clinician, their effectiveness (or lack of it) needs very careful monitoring over time.
Sealing-in management strategies for the cariogenic biofilm
Here the cariogenic biofilm is managed by being sealed from the oral environment, and hence the dietary sugars that fuel it. Carious lesions that are isolated from the oral environment will not progress, but the seal must be effective and durable over time. There is a stronger evidence base supporting the use of sealing-in techniques, than for topical management of the plaque biofilm. Sealing-in strategies that might be used in increasing order of invasiveness, include:
-
Use of unfilled resins – fissure sealants can be used to arrest carious lesions in pits and fissures which have not progressed past micro-cavitation. If cavitation has occurred, use of an adhesive restorative material might be indicated, to achieve a seal of the necessary durability. Initial (non-cavitated) proximal lesions can be sealed either using a variation of the usual fissure sealant technique, or through using the ICON® technique.45 Where infiltration is not available or practitioners do not use it, fluoride varnish can be applied regular while risk exists and parents shown specifically how to clean that area
-
No carious tissue removal, and seal with a preformed metal crown (Hall Technique) – this approach has a strong evidence base and is suitable for pre-cavitated and proximal lesions in primary molars. It can also be used for occlusal lesions where use of fissure sealants or an adhesive restorative material is not judged to be suitable.46,47 (https://en.wikipedia.org/wiki/Hall_Technique)
-
Selective (partial) carious tissue removal, and seal with an adhesive restorative material – this can be useful for cavitated occlusal lesions, where superficial caries can be gently hand excavated to allow a sufficient bulk of adhesive restorative material to be used for a durable restoration. Recent consensus has agreed that carious tissue should only be removed in these lesions until firm dentine is felt and NOT to the extent of reaching hard dentine which is considered over-preparation.30,34 The margins of these restorations must be on sound enamel and dentine. The evidence base does not support this technique for cavitated proximal lesions, where a Hall crown should be used, if possible. There is still limited evidence that glass ionomer is a suitable restorative material for multi-surface cavitated lesions
-
Step-wise (two stage) carious tissue removal, and indirect pulp caps – these technically more demanding strategies are generally only applied in the permanent dentition, and are not usually indicated when managing the primary dentition.
As with the topical strategies, sealing-in strategies need careful monitoring over time, generally including the use of radiography (in line with guidance). Arrested lesions with a non-cariogenic biofilm do not progress. If progression is identified, then the chosen strategy isn't working, and an alternative should be tried.
Management options for asymptomatic carious primary teeth with advanced lesions, or which are not restorable
As with managing the initial and moderate lesions, the advanced lesion requires the clinician to carefully weigh up all the risks and benefits of the various options, and to discuss these fully with the child and their parents. If there is evidence of associated pain or infection (sinus present, or peri-radicular/apical radiolucency), then extraction is indicated. Absence of signs and symptoms of infection does not mean the pulp is healthy, and if a child is medically compromised, then again extraction should be considered. In the absence of these factors, then a judgement has to be made around whether the lesion is likely to be arrestable and whether the tooth is likely to exfoliate before causing pain or infection. The treatment options here are not passive treatments but require very active intervention from the clinician to carry out their part in the process of halting the progress of the disease:
-
Motivating the parent/carer (or the child if they are older)
-
Applying site-specific prevention including non-restorative cavity control
-
Applying fluoride varnish or consider applying SDF.
This is NOT a 'watch and wait' option and efforts to make this course of action work must be clearly documented. If this programme of non-restorative cavity control fails and the lesions are not arrested (with signs of progression) then the tooth may need to be extracted if there is infection present or it is likely to develop.
Working with the child and family to deliver care
As the child moves through adolescence towards becoming a young adult there should be a gradual process of moving the responsibility for their oral health from the parent/carers to the patient themselves; the age at which this happens will depend on the child, the family and their relationship with the oral health care team. At no time does the primary responsibility for a child's oral health lie with the oral health care team. However, an obligation that does lie with the team is ensuring that the parent/carers of a child perceive and accept that the responsibility for their child's oral health lies with them, until the child is old enough to take this on for themselves, and that the oral health care team are there to support them in discharging that responsibility. This will need a shift in behaviour and beliefs, where self-care becomes a core principle of how dental care is provided, and that the time and skills required to achieve this behaviour change are rewarded at the same level of remuneration as repairing teeth where that self-care has gone wrong.
Repair
Actions for carious primary teeth
Prevention must be in place for success
-
For cavitated lesions, change from thinking about how to manage the cavity to how to manage the cariogenic biofilm: can it be managed topically? or by sealing-in?
-
The least invasive option appropriate for the tooth should be chosen
-
Carious lesions should be repaired when cavitation has resulted in a non-cleanable lesion, weakens the tooth structure or compromises aesthetics
-
Exposure of the dental pulp (previously known as a carious exposure) in an asymptomatic tooth constitutes iatrogenic damage
-
Dividing carious lesions into initial or advanced stage can help in making decisions about treatment options
-
Arrested lesions may be able to be maintained without pain and infection in the older child but this relies on active intervention from the clinician and motivation of the parent/carer.
Review (of the child, their oral health and their situation)
Once a treatment plan has been formulated and completed, the ongoing caries risk of the patient (and family) needs to be established and a recall period determined. The recall period reflects the risk of the child, and changes in duration dependant on the risk – longer for lower risk and vice versa. It allows timely intervention with behaviour and dental care related to the child's oral health.
Those children at high caries risk and/or who will suffer greater consequences from the development of carious lesions (that is, the medically compromised) should have recall between three and six months after the initial care period. This allows for reassessment of the caries risk, review of existing white spot lesions for signs of remineralisation or demineralisation and early detection of new lesions. Preventive messages such as diet and oral hygiene can be reinforced.
Those children estimated to be at 'medium' risk should be seen at six monthly intervals, and this interval possibly extended up to 12 months where a regularly attending child can be confidently placed in the low risk category.
Summary of the MID approach
Using the core principles of MID of Recognition, Re-orientation, Remineralisation, Repair and Review allows a comprehensive patient/family assessment, with early diagnosis of carious lesions, a reliable caries risk assessment, implementation of effective preventive measures and minimally destructive restorative care. Essentially, it shifts the focus away from the tooth-centred surgical model, to a child and family-centred model.
Inter-personal, psychosocial and coaching skills need to be regarded with a similar importance and level of remuneration as the 'traditional restorative/surgical approach' if we are to adapt the physician approach to the management of dental caries in children. MID provides us the opportunity, working with the child and their parent/carers, to maintain the oral health of children into adulthood, and to provide them with the ability and will to care for their own oral health from then on.
References
Wikipedia. Convention on the Rights of the Child. Available at: https://en.wikipedia.org/wiki/Convention_on_the_Rights_of_the_Child (accessed 28 May 2017).
Oliver K, Manton D J . Contemporary behaviour management techniques in clinical paediatric dentistry: out with the old and in with the new? J Dent Children 2015; 82: 22–28.
Innes N, Evans D . Managing dental caries in children: improving acceptability and outcomes through changing priorities and understanding the disease. Br Dent J 2009; 206: 549–550.
Peterson P E, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C . Bulletin of the World Health Organization. World Health Organization 2005; 83.
Patel R . The State of Oral Health in Europe: Better Oral Health European Platform. 2012. Available at: http://www.oralhealthplatform.eu/our-work/the-state-of-oral-health-in-europe/ (accessed 2 June 2017).
Vernazza C R, Rolland S L, Chadwick B, Pitts N . Caries experience, the caries burden and associated factors in children in England, Wales and Northern Ireland 2013. Br Dent J 2016; 221: 315–320.
Kassebaum N J, Bernabé E, Dahiya M, Bhandari B, Murray C J L, Marcenes W . Global burden of untreated caries: a systematic review and metaregression. J Dent Res 2015; 94: 650–658.
Macpherson L M D, Ball G, Carson S et al. National Dental Inspection Programme (NDIP): The Scottish Dental Epidemiology Coordinating Committee. 28 October 2014. Available at: http://ndip.scottishdental.org/2014-ndip-report-published/ (accessed 2 June 2017).
Macpherson L M D, Ball G, Carson S et al. National Dental Inspection Programme (NDIP) 2015: The Scottish Dental Epidemiology Coordinating Committee, 27 October 2015. Available at: http://ndip.scottishdental.org/wp-content/uploads/2015/10/ndip_scotland2015-P7.pdf (accessed 2 June 2017).
Selwitz R H, Ismail A I, Pitts N B . Dental caries. Lancet 2007; 369: 51–59.
Jackson S L, Vann W F, Kotch J B, Pahel B T, Lee J Y . Impact of poor oral health on children's school attendance and performance. Am J Public Health 2011; 101: 1900–1906.
Bernabé E, MacRitchie H, Longbottom C, Pitts N B, Sabbah W . Birth weight, breastfeeding, maternal smoking and caries trajectories. J Dent Res 2016; 96: 171–178.
Dawson A S, Makinson O F . Dental treatment and dental health. Part 1. A review of studies in support of a philosophy of minimum intervention dentistry. Aust Dent J 1992; 37: 126–132.
Massler M . Pulpal reactions to dental caries. Int Dent J 1967; 17: 441–460.
Handelman S L, Washburn F, Wopperer P . Two-year report of sealant effect on bacteria in dental caries. J Am Dent Assoc 1976; 93: 967–970.
Walsh L J, Brostek A M . Minimum intervention dentistry principles and objectives. Aust Dent J 2013; 58: 3–16.
Elderton R J . Management of early dental caries in fissures with fissure sealant. Br Dent J 1985; 158: 254–258.
Scottish Intercollegiate Guidelines Network. Dental interventions to prevent caries in children; a national clinical guideline. Edinburgh: Healthcare Improvement Scotland, 2014. Available at: http://www.sign.ac.uk/sign-138-dental-interventions-to-prevent-caries-in-children.html (accessed 2 June 2017).
Public Health England. Department of Health. Delivering better oral health: an evidence-based toolkit for prevention. 3rd ed. London, 2014. https://www.gov.uk/government/publications/delivering-better-oral-health-an-evidence-based-toolkit-for-prevention (accessed 2 June 2017).
Scottish Dental Clinical Effectiveness Programme. Prevention and management of dental caries in children. NES, 2010. Available at: http://www.sdcep.org.uk/published-guidance/caries-in-children/ (accessed 2 June 2017).
Plonka K A, Pukallus M L, Barnett A G, Holcombe T F, Walsh L J, Seow W K . A longitudinal case-control study of caries development from birth to 36 months. Caries Res 2013; 47: 117–127.
Campbell C, Soldani F, Busutil-Naudi A, Chadwick B . Non-pharmacological behaviour management. London, UK: British Society for Paediatric Dentistry, 2011. http://bspd.co.uk/Resources/BSPD-Guidelines (accessed 2 June 2017).
Harris R, Gamboa A, Dailey Y, Ashcroft A . One-to-one dietary interventions undertaken in a dental setting to change dietary behaviour. Cochrane Database Syst Rev 2012; CD006540.
Kay E, Vascott D, Hocking A, Nield H, Dorr C, Barrett H . A review of approaches for dental practice teams for promoting oral health. Community Dent Oral Epidemiol 2016; 44: 313–330.
Harrison R, Benton T, Everson-Stewart S, Weinstein P . Effect of motivational interviewing on rates of early childhood caries: a randomized trial. Paediatr Dent 2007; 29: 16–22.
Weinstein P, Harrison R, Benton T . Motivating mothers to prevent caries: confirming the beneficial effect of counseling. J Am Dent Assoc 2006; 137: 789–793.
Frencken J E, Peters M C, Manton D J, Leal S C, Gordan V V, Eden E . Minimal intervention dentistry for managing dental caries – a review. Int Dent J 2012; 62: 223–243.
ten Cate J M . Remineralization of caries lesions extending into dentin. J Dent Res 2001; 80: 1407–1411.
Ricketts D, Lamont T, Innes N P, Kidd E, Clarkson J E . Operative caries management in adults and children. Cochrane Database Syst Rev 2013; CD003808.
Schwendicke F, Frencken J E, Bjørndal L et al. Managing carious lesions: consensus recommendations on carious tissue removal. Adv Dent Res 2016; 28: 58–67.
Jablonski-Momeni A, Stachniss V, Ricketts D N, Heinzel-Gutenbrunner M, Pieper K . Reproducibility and accuracy of the ICDAS-II for detection of occlusal caries in vitro. Caries Res 2008; 42: 79–87.
Braga M M, Mendes F M, Martignon S, Ricketts D N, Ekstrand KR . In vitro comparison of Nyvad's system and ICDAS-II with Lesion Activity Assessment for evaluation of severity and activity of occlusal caries lesions in primary teeth. Caries Res 2009; 43: 405–412.
Shoaib L, Deery C, Ricketts D N, Nugent Z J . Validity and reproducibility of ICDAS II in primary teeth. Caries Res 2009; 43: 442–448.
Innes N P, Frencken J E, Bjorndal L et al. Managing carious lesions: consensus recommendations on terminology. Adv Dent Res 2016; 28: 49–57.
Hansen N V, Nyvad B . Non-operative control of cavitated approximal caries lesions in primary molars: a prospective evaluation of cases. J Oral Rehabil 2017; 44: 537–544.
Santamaria R M, Innes N P, Machiulskiene V, Evans D J, Alkilzy M, Splieth C H . Acceptability of different caries management methods for primary molars in a RCT. Int J Paediatr Dent 2015; 25: 9–17.
Santamaria R M, Innes N P, Machiulskiene V, Evans D J, Splieth C H . Caries management strategies for primary molars: 1-yr randomized control trial results. J Dent Res 2014; 93: 1062–1069.
Santamaria R, Innes N P T, Machiulskiene V, J S, Alkilzy M, Splieth C . Alternative caries management options for primary molars: 2.5-yr outcomes of a randomised clinical trial Caries Res 2017; in press.
Wong M C, Clarkson J, Glenny A M et al. Cochrane reviews on the benefits/risks of fluoride toothpastes. J Dent Res 2011; 90: 573–579.
Marinho V C . Applying prescription-strength home-use and professionally applied topical fluoride products may benefit people at high risk for caries – the American Dental Association (ADA) 2013 clinical practice guideline recommendations. J Evid Based Dent Pract 2014; 14: 120–123.
Marinho V C, Worthington H V, Walsh T, Clarkson J E . Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev 2013; CD002279.
Duangthip D, Jiang M, Chu C H, Lo E C . Non-surgical treatment of dentin caries in preschool children - systematic review. BMC Oral Health 2015; 15: 44.
Gao S S, Zhang S, Mei M L, Lo E C, Chu C H . Caries remineralisation and arresting effect in children by professionally applied fluoride treatment – a systematic review. BMC Oral Health 2016; 16: 12.
Moynihan P J, Kelly S A M . Effect on caries of restricting sugars intake: systematic review to inform who guidelines. J Dent Res 2014; 93: 8–18.
Dorri M, Dunne S M, Walsh T, Schwendicke F . Micro-invasive interventions for managing proximal dental decay in primary and permanent teeth. Cochrane Database Syst Rev 2015; CD010431.
Innes N P, Evans D J, Stirrups D R . Sealing caries in primary molars: randomized control trial, 5-year results. J Dent Res 2011; 90: 1405–1410.
Innes N P, Ricketts D, Chong L Y, Keightley A J, Lamont T, Santamaria R M . Preformed crowns for decayed primary molar teeth. Cochrane Database Syst Rev 2015; CD005512.
Acknowledgements
The authors would like to thank Victoria Pickering for her administrative help in preparing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Innes, N., Manton, D. Minimum intervention children's dentistry – the starting point for a lifetime of oral health. Br Dent J 223, 205–213 (2017). https://doi.org/10.1038/sj.bdj.2017.671
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.671
This article is cited by
-
Evaluation of proximal slicing in primary maxillary incisors with proximal caries- a retrospective cohort study
BMC Oral Health (2023)
-
Factors predicting different times for brushing teeth during the day: multilevel analyses
BMC Oral Health (2023)
-
A scoping literature review on minimum intervention dentistry for children with dental caries
British Dental Journal (2022)
-
Recommended procedures for the management of early childhood caries lesions – a scoping review by the Children Experiencing Dental Anxiety: Collaboration on Research and Education (CEDACORE)
BMC Oral Health (2020)
-
When to intervene in the caries process? A Delphi consensus statement
British Dental Journal (2020)