Abstract
Objective:
Several studies have indicated a correlation between the number of platelet transfusions received by newborn intensive care unit (NICU) patients and the mortality rate. The number of platelet transfusions might be a marker for level of illness, and thus predictive of mortality. However, an alternative hypothesis is that multiple platelet transfusions themselves are harmful in this population.
Study Design:
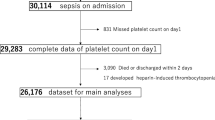
We evaluated data from all thrombocytopenic neonates cared for in the Intermountain Healthcare NICUs in the past 4 years, seeking associations between the lowest platelet count recorded, number of platelet transfusions received and mortality rate. We also conducted a sensitivity analysis to examine the hypothesis that platelet transfusions were responsible for some fraction of the mortality rate.
Result:
Transfusion and outcome data were examined from 1600 thrombocytopenic NICU patients. At any level of platelet count, some patients received platelet transfusions but others did not. However, at all levels of platelet count, those that received platelet transfusions had a higher mortality rate. Neonates not given any platelet transfusions had a mortality rate of 2%, those with 1 or 2 transfusions had a mortality rate of 11% (P<0.001); those with >10 had a mortality rate of 35% (P<0.001); and those with ⩾20 had a mortality rate of 50% (P<0.001). A sensitivity analysis suggested that the platelet transfusions themselves were very likely responsible for some fraction of the increasing mortality rate.
Conclusion:
The number of platelet transfusions administered in the NICU predicts the mortality rate. Some of this correlation is ascribable to unknown and unmeasured factors such as level of illness. However, the present data and the sensitivity analysis both suggest that some of this correlation is due to harmful effects of multiple platelet transfusions in this group of patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Del Vecchio A, Sola MC, Teriaque DW, Hutson AD, Wright D, Garcia MG et al. Platelet transfusions in the neonatal intensive care unit: factors predicting patients who will require multiple transfusions. Transfusion 2001; 41: 803–808.
Garcia MG, Duemas E, Sola MC, Hutson AD, Christensen RD . Epidemiologic and outcome studies of patients who received platelet transfusions in the neonatal intensive care unit. J Perinatol 2001; 21: 415–420.
Chakravorty S, Murray N, Roberts I . Neonatal thrombocytopenia. Early Hum Dev 2005; 81: 35–41.
Christensen RD, Henry E, Wiedmeier SE, Stoddard RA, Sola-Visner MC, Lambert DK et al. Thrombocytopenia among extremely-low birth-weight neonates: data from a multihospital healthcare system. J Perinatol 2006; 26: 348–353.
Fernandes CJ, O'Donovan DJ . Platelet transfusions in infants with necrotizing entercolitis. Curr Hematol Rep 2006; 5: 76–81.
Roberts IAG, Murray NA . Neonatal thrombocytopenia. Curr Hematol Rep 2006; 5: 55–63.
Banchette VS, Rand ML . Platelet disorders in newborn infants: diagnosis and management. Semin Perinatol 1997; 21: 53–62.
Murray NA . Evaluation and treatment of thrombocytopenia in the neonatal intensive care unit. Acta Paediatric Suppl 2002; 438: 74–81.
Kahn DJ, Richardson DK, Billett HH . Inter-NICU variation in rates and management of thrombocytopenia among very low birth-weight infants. J Perinatol 2003; 23: 312–316.
Khashu M, Osiovich H, Henry D, AlKhotani A, Solimano A, Speert DP . Persistent bacteremia and severe thrombocytopenia caused by coagulase-negative staphylococcus in a neonatal intensive care unit. Pediatrics 2006; 117: 341–348.
Kenton AB, Hegemier S, Smith EO, O'Donovan DJ, Brandt ML, Cass DL et al. Platelet transfusions in infants with necrotizing entercolitis do not lower mortality but may increase morbidity. J Perinatol 2005; 25: 173–177.
Roberts IAG, Murray NA . Thrombocytopenia in the newborn. Curr Opin Pediatr 2003; 15: 17–23.
Lin DY, Psaty BM, Kronmal RA . Assessing the sensitivity of regression results to unmeasured confounders in observational studies. Biometrics 1998; 54: 948–963.
Andrew M, Caco VC, Kirpalani H, Jefferies A, Ohlsson A, Watts J et al. A randomized, controlled trial of platelet transfusions in thrombocytopenic premature infants. J Pediatr 1993; 123: 285–291.
Gajic O, Dzik WH, Toy P . Fresh frozen plasma and platelet transfusion for nonbleeding patients in the intensive care unit: benefit or harm? Crit Care Med 2006; 34: 170–173.
Petaja J, Andersson S, Syrjala M . A simple automatized audit system for following and managing practices of platelet and plasma transfusions in a neonatal intensive care unit. Transfusion Med 2004; 4: 281–288.
Kopko PM, Holland PV . Mechanisms of severe transfusion reactions. Elsevier Science, Paris 2001; 8: 278–281.
Kleinman S, Chan P, Robillard P . Risks associated with transfusion of cellular blood components in Canada. Transfusion Med Rev 2003; 17: 120–162.
Murray NA, Hawarth LJ, McCloy MP, Letsky EA, Roberts IA . Platelet transfusion in the management of severe thrombocytopenia in neonatal intensive unit patients. Transfusion Med 2002; 12: 35–41.
Kuehnert MJ, Roth VR, Haley NR, Gregory KR, Elder KV, Schreiber GB et al. Transfusion-transmitted bacterial infection in the United States, 1998 through 2000. Transfusion 2001; 41: 1493–1499.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baer, V., Lambert, D., Henry, E. et al. Do platelet transfusions in the NICU adversely affect survival? Analysis of 1600 thrombocytopenic neonates in a multihospital healthcare system. J Perinatol 27, 790–796 (2007). https://doi.org/10.1038/sj.jp.7211833
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211833
Keywords
This article is cited by
-
Assessment of hemostatic profile in neonates with necrotizing enterocolitis using Rotational Thromboelastometry (ROTEM)
Pediatric Research (2023)
-
The Usability of Platelet Mass Index Thresholds to Assess the Repeated Platelet Transfusion Requirements in Neonates
Indian Journal of Hematology and Blood Transfusion (2023)
-
Platelet transfusions in preterm infants: current concepts and controversies—a systematic review and meta-analysis
European Journal of Pediatrics (2023)
-
Bleeding in neonates with severe thrombocytopenia: a retrospective cohort study
BMC Pediatrics (2022)
-
Role of platelets in neonatal necrotizing enterocolitis
Pediatric Research (2021)