Abstract
Subjects at their first psychotic episode show an enlarged volume of the pituitary gland, but whether this is due to hypothalamic–pituitary–adrenal (HPA) axis hyperactivity, or to stimulation of the prolactin-secreting cells by antipsychotic treatment, is unclear. We measured pituitary volume, using 1.5-mm, coronal, 1.5 T, high-resolution MRI images, in 78 patients at the first psychotic episode and 78 age- and gender-matched healthy controls. In all, 18 patients were antipsychotic-free (12 of these were antipsychotic-naïve), 26 were receiving atypical antipsychotics, and 33 were receiving typical antipsychotics. As hypothesized, patients had a larger pituitary volume than controls (+22%, p<0.001). When divided by antipsychotic treatment, and compared to controls, the pituitary volume was 15% larger in antipsychotic-free patients (p=0.028), 17% larger in patients receiving atypicals (p=0.01), and 30% larger in patients receiving typicals (p<0.001). Patients receiving typicals not only had the largest pituitary volume compared to controls but also showed a trend for a larger pituitary volume compared to the other patients grouped together (+11%, p=0.08). When divided by diagnosis, and compared to controls, the pituitary volume was 24% larger in patients with schizophrenia/schizophreniform disorder (n=40, p<0.001), 19% larger in depressed patients (n=13, p=0.022), 16% larger in bipolar patients (n=16, p=0.037), and 12% larger in those with other psychoses (n=9, p=0.2). In conclusion, the first-episode of a psychotic disorder is associated with a larger pituitary independently of the presence of antipsychotic treatment, and this could be due to activation of the HPA axis. Typical antipsychotics exert an additional enlarging effect on pituitary volume, likely to be related to activation of prolactin-secreting cells. This activation of the hormonal stress response could participate to the important metabolic abnormalities observed in patients with psychosis.
Similar content being viewed by others
INTRODUCTION
We have previously shown that subjects at their first episode of psychoses show an enlarged volume of the pituitary gland, but it is still unclear whether this is due to activation of the hormonal stress response during the psychotic experience, or to stimulation of the prolactin-secreting cells by antipsychotic treatment (Cotter and Pariante, 2002; Pariante et al, 2004). Both old (Sachar et al, 1970) and recent studies (Ryan et al, 2003, 2004a, 2004b) have demonstrated hyperactivity of the main hormonal stress system, the hypothalamic–pituitary–adrenal (HPA) axis, in subjects experiencing their first psychotic episode. In turn, HPA axis hyperactivity—in major depression—has been linked to an increased volume of the pituitary gland (Axelson et al, 1992; Krishnan et al, 1991; MacMaster and Kusumakar, 2004). The pituitary gland regulates HPA axis activity by secreting the adrenocorticotropic hormone (ACTH), and its increased volume has been interpreted as reflecting an increase in the size and number of corticotrope cells producing ACTH (Axelson et al, 1992; Krishnan et al, 1991; Pariante et al, 2004). Indeed, in patients with major depression, the volume of the pituitary correlates with the circulating cortisol levels (Axelson et al, 1992; Krishnan et al, 1991).
Recently, we have described an increased volume of the pituitary gland, measured by magnetic resonance imaging (MRI), in 24 subjects with a first-episode of psychosis recruited in Melbourne, Australia (Pariante et al, 2004). This work supports the hypothesis that these patients have activation of the HPA axis. However, the interpretation of these findings is complicated by the fact that all patients were receiving antipsychotic medication at the time of scanning, and antipsychotics increase prolactin levels in humans and induce proliferation of prolactin-secreting cells in animals (Halbreich and Kahn, 2003; Perez et al, 1986; Saiardi et al, 1997). Furthermore, the small sample size did not allow us to evaluate any possible differences associated with specific diagnoses within psychoses. To clarify these issues, we have investigated the pituitary volume, using high-resolution MRI, in a different sample of 78 subjects at their first psychotic episode, recruited in London as part of the UK ÆSOP (Aetiology and Ethnicity in Schizophrenia and Other Psychoses) study (Dazzan et al, 2004; Dazzan et al, 2005). This is an epidemiologically based sample of patients at the first psychotic episode, which includes both antipsychotic-treated and antipsychotic-free subjects, and both affective and nonaffective psychoses. We hypothesized that the pituitary volume would be enlarged in both drug-free and antipsychotic-treated subjects, and across diagnoses.
SUBJECTS AND METHODS
Subjects
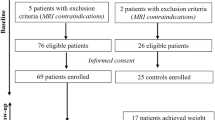
We studied 156 subjects: 78 subjects at their first episode of psychosis and 78 age- and gender-matched healthy controls. Subjects were recruited in Southeast London as part of the ÆSOP study, which investigates, in three cities, the higher rates of schizophrenia in the African-Caribbean population in the UK (Dazzan et al, 2004; Dazzan et al, 2005). Ethical approval for the study was granted by the Ethical Committee of the Institute of Psychiatry, and the participants gave written informed consent, in accordance with the Declaration of Helsinki.
We approached subjects aged 16-65 years, who consecutively presented for the first time to the local psychiatric services of Southeast London for a functional psychotic illness (ICD10 F10-19, excluding coding F1x.0 for Acute intoxication; F20-29 and F30-39, psychotic codings) (World Health Organisation, 1992), over a 3-year period. Exclusion criteria were (a) a history of head trauma resulting in loss of consciousness for over 1 h; (b) the presence of a disease of the central nervous system; (c) moderate or severe learning disabilities as defined by ICD-10 (World Health Organisation, 1992); (d) poor fluency in English language; and (e) transient psychotic symptoms resulting from acute intoxication as defined by ICD-10 (World Health Organisation, 1992), following the administration of alcohol or other psychoactive substance. In total, 115 right-handed patients consented to have an MRI scan. A total of 10 patients terminated the scanning session before full image acquisition had been achieved and a further 15 scans were excluded from the analysis (13 due to subject motion, one because of congenital hydrocephalus, and one because of the presence of a subarachnoid cyst). Of the 90 subjects on which a valid MRI was available, 78 could be matched (for age and gender) to a sample of 78 healthy controls recruited from the same sociodemographic areas and who had consented to have an MRI scan.
Clinical Measures
We interviewed patients using the WHO Schedules for Clinical Assessment in Neuropsychiatry (SCAN) (World Health Organisation, 1994). We made a diagnosis according to ICD-10 criteria (World Health Organisation, 1992) by consensus in meetings with senior clinicians (RM or JL) in which all clinical information was presented. We used both the patients' medical notes and the information obtained from the SCAN interviews to establish the date of onset, and duration of illness was operationalized as the time in weeks between the onset of psychotic symptoms and the MRI scan date. A total symptomatology score was obtained by summing the SCAN's individual symptom item scores, as previously done for the Present State Examination (PSE) (Wing et al, 1974; Wing and Sturt, 1978). This was an appropriate model to adopt as the SCAN incorporates the 10th edition of the PSE.
Pharmacological Treatment
From clinical notes, we completed a medication record for each patient. We calculated the total duration of antipsychotic exposure in days and the daily antipsychotic dose at the time of MRI scan, converted into chlorpromazine equivalents for typical antipsychotics. We also recorded information on treatment with antidepressants. Therapeutic interventions (type of medication and length of treatment) were decided by the responsible clinical team, based on clinical presentation, and were not influenced by participation to the study. For the purposes of the main study, we obtained one MRI scan as soon as possible after first presentation to the services, independently of length of antipsychotic treatment. Depending on their current treatment, subjects were divided into three groups: typical antipsychotics, atypical antipsychotics, and antipsychotic-free. The criteria for this division have been already published (Dazzan et al, 2005) and are based on existing literature on antipsychotic wash-out. We considered ‘antipsychotic-free’ those subjects who had not taken any antipsychotic in the 3 weeks prior to the MRI scan (Farde et al, 1986; Miller et al, 1997a; Miller et al, 1997b; Miller et al, 2001). We considered subjects as being on treatment with atypical antipsychotics if they had been taking one atypical antipsychotic only for at least 2 weeks prior to MRI, and had not taken more than one dose of a typical antipsychotic during this time. Similar criteria were used for the subjects on typicals; however, because typicals affect prolactin levels even when administered together with atypicals, patients who had received both typicals and atypicals during the 2 weeks preceding the scan (n=4) were categorized as ‘typicals’. Clearly, the allocation of subjects to each of these three groups was nonrandomized, but based on the medication prescribed by the clinician in charge at the time of MRI scan. Nevertheless, previous comparisons of brain structures morphology between these three subgroups have highlighted qualitative differences in the effects of the different antipsychotic classes on the brain (Dazzan et al, 2005). One subject on which we had no medication history was excluded from this analysis.
Structural MRI Image Acquisition
Scans were acquired with a GE Signa 1.5-T system (GE Medical Systems, Milwaukee), at the Maudsley Hospital, London. The whole brain was scanned with a 3-D inversion recovery prepared fast spoiled GRASS (SPGR) T1-weighted data set. These T1-weighted images were obtained in the coronal plane with 1.5 mm contiguous sections. TR was 13.8 ms, TI was 450 ms, TE was 2.8 ms, and the flip angle was 20 degrees, with one data average and a 256 × 256 × 128 pixel matrix. Acquisition time was 6 min and 27 sec.
Pituitary Measurement
Each pituitary was traced in all coronal slices where it could be visualized, using ANALYZE 7.5 (Mayo) with a method that has been used previously by us and others (MacMaster and Kusumakar, 2004; Pariante et al, 2004; Sassi et al, 2001). The pituitary stalk was excluded from the tracings, whereas we included a posterior bright spot, corresponding to the posterior pituitary (the intensity of which is thought to reflect vasopressin concentrations). We traced around the usually well-defined borders of anterior and posterior pituitary: the diaphragma sellae, superiorly; the sphenoid sinus, inferiorly; and the cavernous sinuses, bilaterally. Figure 1 shows these borders in a good-quality image from the original Australian sample in which we developed the measurement method (Pariante et al, 2004). Volume of the pituitary (in mm3) was calculated by summing volumes for all relevant slices. All pituitaries were traced by two investigators (AD, FB), after training with another senior member of the team (PD). These investigators were blind to the clinical or sociodemographic characteristics of the subjects during the tracing process. The inter-raters reliabilities (between AD, FB, and PD) ranged 0.92–0.95; the intra-rater reliabilities ranged 0.95–0.97.
Statistical Analysis
Data are presented as individual values, mean±standard deviation (SD), or adjusted means and standard error of mean (SEM), as detailed. All differences in pituitary volume between groups were examined conducting two-way analysis of variance tests, using group as between-subject factors and adjusting for gender, followed by pairwise comparisons of estimated means. Categorical variables were analyzed using the chi-square test. As there were no differences in whole-brain volume (WBV) between first-episode subjects and controls (ANOVA, F=0.05; df=1, 155; p=0.8), the main analyses of pituitary volume did not include this variable as a covariate. However, we run a second set of confirmatory analyses using WBV as a covariate and found no difference in the results (data not shown). The relationships between pituitary volumes and clinical and sociodemographic continuous variables were examined using Pearson's r.
RESULTS
Characteristics of the Sample
The main demographics and clinical features of the first-episode subjects and controls are presented in Table 1. The first-episode subjects are presented as a whole group (n=78) and after division according to antipsychotic treatment (n=77; drug-free=18, atypical= 26, typical=33) or to diagnosis (n=78; schizophrenia/schizophreniform disorder=40, affective=29, other psychoses=9). As expected, there were no significant differences in age and gender between the controls and the first-episode subjects. When the first-episode group was further divided, there were no differences in age and gender based on antipsychotic treatment, while there was a nonsignificant tendency for more female subjects to be in the affective psychosis group (p=0.12). Moreover, there was a trend for the extent of psychopathology according to the SCAN to be lower in drug-free subjects (p=0.09 vs atypicals and p=0.06 vs typicals).
Pituitary Volumes
There was a significant difference in pituitary volume between the first-episode and control subjects (ANOVA, F=20.7; df=1, 155; p<0.001) (Figure 2). Specifically, pituitary volume in first-episode subjects was significantly larger (+22%) than in controls (estimated mean difference±SEM: +125±27 mm3). Although the examination of the individual data showed an overlap between the groups, 63 of the 78 first-episode subjects (81%) had pituitary volumes that were larger than the median of the control subjects.
In the whole sample, female subjects had larger pituitaries than male subjects (uncorrected values: 671±191 vs 607±170 mm3; ANOVA, F=5.4; df=1, 155; p=0.021), and pituitary volume was negatively correlated with age (r=−0.25, p=0.002). There was no gender by group interaction in the differences in pituitary volume between first-episode and controls (ANOVA, F=0.05; df=1, 155; p=0.8).
Effects of Antipsychotic Treatment
Of the 18 patients who were antipsychotic-free (for at least 3 weeks), 12 were antipsychotic-naïve, three had previously received an atypical, and three had previously received a typical (two for 2–3 days only, and one for 20 days). Of the 26 patients receiving atypicals, 19 were taking olanzapine, five, risperidone, one, sertindole, and one, amisulpride. Of the 33 patients receiving typicals, three were on depot, and the others were on oral medication.
There was a significant difference in pituitary volume between the three groups of patients and controls (ANOVA, F=8.7; df=3, 152; p<0.001; see Figure 3). Specifically, compared to controls, the pituitary volume was 15% larger in antipsychotic-free patients (+85±38 mm3, p=0.028), 17% larger in patients receiving atypicals (+100±38 mm3, p=0.01), and 30% larger in patients receiving typicals (+171±34 mm3, p<0.001). When the 12 neuroleptic-naïve patients were considered separately, their pituitary volume was also 17% larger than controls, but this difference only reached trend statistical significance (+97±51 mm3, p=0.08). The patients receiving typicals not only had the largest pituitary volume compared to controls but also had a larger volume (+11%) compared with all other patients taken together, although this difference also only reached trend statistical significance (+74±42 mm3, p=0.08). There was no effect of current antidepressant treatment on pituitary volume (ANOVA, F=1.4; df=1, 74; p=0.7). After adjusting for the class of antipsychotic treatment, there was no correlation between pituitary volume and either dose of antipsychotic at the time of the scan (r=0.13, p=0.3) or total days of antipsychotic treatment before the scan (r=−0.11, p=0.3).
Individual measures of pituitary volumes in first-episode patients (n=77; one subject on which we had no medication history was excluded from this analysis) divided by antipsychotic treatment (free, n=18; atypicals, n=26; typicals, n=33). Bars denote the estimated mean for each group after adjustment for gender. Compared to controls, the pituitary volume was 15% larger in antipsychotic-free patients (p=0.028), 17% larger in patients receiving atypicals (p=0.01), and 30% larger in patients receiving typicals (p<0.001).
Effects of Diagnosis
A total of 40 patients had a diagnosis of schizophrenia/schizophreniform disorder, 29 had an affective psychosis (bipolar=16, depression=13), and nine had other psychoses. Again, there was a significant difference in pituitary volume between the three groups of patients and controls (ANOVA, F=6.2; df=3, 152; p=0.001; see Figure 4). Specifically, compared to controls, the pituitary volume was 24% larger in patients with schizophrenia/schizophreniform disorder (+139±34 mm3, p<0.001), 17% larger in those with affective psychosis (+100±36 mm3, p=0.006), and 12% larger in those with other psychoses (not statistically significant: +72±56 mm3, p=0.2). There was no difference between bipolar and depressive psychoses: compared to controls, the pituitary volume was 16% larger in bipolar patients (+92±44 mm3, p=0.037) and 19% larger in depressed patients (+112±48 mm3, p=0.022).
Individual measures of pituitary volumes in first-episode patients divided by diagnostic group (schizophrenia/schizophreniform (Schiz.), n=40; affective, n=29, other, n=9). Bars denote the estimated mean for each group after adjustment for gender. Compared to controls, the pituitary volume was 24% larger in patients with schizophrenia/schizophreniform disorder (p<0.001), 17% larger in those with affective psychosis (p=0.006), and 12% larger in those with other psychoses (not statistically significant, p=0.2).
Interestingly, most patients with schizophrenia/schizophreniform disorder were on atypicals, while most patients with affective psychosis were on typicals. Specifically, 21 patients with schizophrenia/schizophreniform disorder (out of 39, 54%) were on atypicals, 13 (33%) were on typicals, and five (13%) were antipsychotic-free; in contrast, two patients with affective psychosis (7%) were on atypicals, 18 (62%) were on typicals, and nine (31%) were antipsychotic-free (chi square=19.3, df=4, p=0.001). There was no interaction between antipsychotic treatment and diagnoses on pituitary volume (ANOVA, F=0.5, df=4, 73; p=0.7), that is, patients on typicals had the largest pituitary volume across diagnoses (data not shown).
After adjusting for antipsychotic treatment and diagnosis, there was no correlation between pituitary volume and either duration of illness (r=0.07, p=0.5) or total symptom score (r=−0.09, p=0.4).
DISCUSSION
Our results indicate that the first-episode of a psychosis is associated with larger size of the pituitary gland, across diagnostic subgroups. This work confirms and extends our previous findings in a smaller Australian sample (Pariante et al, 2004). Furthermore, we now demonstrate that patients who are antipsychotic-free and patients on atypical antipsychotics have similar increases of pituitary volume (compared to matched controls), while patients on typical antipsychotics have an even larger pituitary volume. These results show that the enlarged pituitary is present independently of the effects of the antipsychotics, but also indicate that activation of prolactin-secreting cells by typicals may cause an additional enlargement of the pituitary.
We suggest that the increased pituitary volume is due to activation of the HPA axis. Animal and clinical studies have demonstrated that HPA axis activation by corticotropin-releasing hormone (CRH) or by stress leads to an increase in the number and size of corticotropes in the pituitary gland (Asa et al, 1992; Carey et al, 1984; Gertz et al, 1987; Westlund et al, 1985). This increase in the size and numbers of corticotropes can increase pituitary volume in humans as shown on brain imaging (Kubota et al, 1992; Mineura et al, 1987). Moreover, patients with major depression, where HPA axis hyperactivity has been consistently demonstrated, also have increased pituitary volumes (Axelson et al, 1992; Krishnan et al, 1991; MacMaster and Kusumakar, 2004). Indeed, in depressed patients, the pituitary volume is positively correlated with post-dexamethasone cortisol levels, suggesting that the pituitary gland is larger in those patients who show less suppression of cortisol secretion by dexamethasone, and thus have a more hyperactive HPA axis (Axelson et al, 1992).
Of course, our data in patients receiving typical antipsychotics indicate that the pituitary volume is also sensitive to activation of lactotrope cells. It is well known that blockade of the D2 dopamine receptors on lactotropes by typical antipsychotics induces proliferation of these cells in animals and increased prolactin levels in humans (Halbreich and Kahn, 2003; Perez et al, 1986; Saiardi et al, 1997). We now find that this phenomenon has a macroscopic brain correlate. Although prolactin secretion is also activated by stress, previous studies have found no evidence that this hormone is elevated in antipsychotic-free patients (Muck-Seler et al, 2004; Rao et al, 1994; Segal et al, 2004; Warner et al, 2001). In fact, one recent study found elevated cortisol levels but normal prolactin levels in the same antipsychotic-free patients with schizophrenia (Muck-Seler et al, 2004). This further supports the notion that the increased pituitary volume in our antipsychotic-free subjects (and in those receiving atypicals) is due to activation of the HPA axis. Indeed, a strength of this paper is that the antipsychotic-free subjects were either antipsychotic-naïve (67%) or had received antipsychotics only for a short period of time. Moreover, those who had received antipsychotics had stopped for at least 3 weeks before the MRI scan, and this interval is sufficient for prolactin levels to decrease in patients switched from a prolactin-increasing to a prolactin-spearing antipsychotic (Kinon et al, 2003). Therefore, we believe that there was no longer any effect of previous (typical) antipsychotics on pituitary volume in these antipsychotic-free subjects.
Clearly, the allocation of the subjects to the treatment groups was nonrandomized, and this could have influenced the results. For example, and perhaps unsurprisingly, antipsychotic-free subjects had lower symptoms severity compared to the treated groups, while symptoms score were similar in those on atypicals and those on typicals. However, pituitary volume was similar in antipsychotic-free patients and in those on atypicals, even if their symptoms scores were different; and pituitary volume was different in those on atypicals and those on typicals, even if their symptoms scores were similar. Taken together, these findings support the conclusion that subjects receiving typical antipsychotics have a larger pituitary volume because of the activation of lactotrope cells and not because of baseline clinical differences.
To our knowledge, this is the first study to compare a (putative) marker of HPA axis function in patients with a first-episode of schizophrenia, psychotic depression or psychotic mania. Previous studies have found raised cortisol and ACTH levels in patients with first-episode schizophrenia (Ryan et al, 2003, 2004a, 2004b; Sachar et al, 1970), together with increased intra-abdominal fat (Ryan et al, 2004a) and impaired glucose tolerance (Ryan et al, 2003), thus suggesting that these endocrine abnormalities could have important metabolic consequences (Dinan, 2004). Studies of patients in the acute relapse phase of a psychotic disorder (with florid symptoms, newly hospitalized or unmedicated) have also found elevated cortisol levels that correlate with the severity of psychotic and arousal symptoms (Lammers et al, 1995; Tandon et al, 1991; Walder et al, 2000), nonsuppression of cortisol secretion by dexamethasone in the dexamethasone suppression test and in the dexamethasone/CRH test (Coryell and Tsuang, 1992; Herz et al, 1985; Lammers et al, 1995), and elevated levels of CRH in the cerebrospinal fluid (Banki et al, 1987). Finally, patients with bipolar disorder also show HPA axis hyperactivity (Kunzel et al, 2003; Linkowski et al, 1994; Watson et al, 2004). It is of note that a smaller pituitary volume has been described in psychiatric patients with long duration of illness and whose mental state is stable or less severely affected at the time of the MRI scan: for example, in euthymic and depressed bipolar patients, or in patients with chronic, treated schizophrenia (Pariante et al, 2004). As we and others have previously speculated, the explanations for the smaller pituitary volume have ranged from being the consequence of a chronic activation of the HPA axis to being a neurodevelopmental problem (Lum et al, 2002; Pariante et al, 2004; Sassi et al, 2001). A recent paper by Chen et al (2004), showing normal pituitary volume in children with bipolar disorder, supports the notion that is an acquired, rather than a neurodevelopmental, abnormality, and suggests that a long duration of illness (longer than the 3.9 years mean in this children's sample) is needed for the pituitary to decrease in size. In our previous study, which found a smaller pituitary volume in patients with chronic schizophrenia, the mean duration of illness was of 19 years (Pariante et al, 2004).
Interestingly, the HPA axis hyperactivity (and the increased pituitary volume) in depression has been interpreted as indicating a lack of negative inhibitory feedback by circulating glucocorticoid hormones on the HPA axis, especially at the level of the pituitary (glucocorticoid resistance) (Pariante et al, 2002; Pariante, 2003; Pariante and Miller, 2001; Raison and Miller, 2003). Indeed, increased size and number of corticotropes and increased volume of the pituitary are present also in subjects with a lack of negative inhibitory feedback by circulating glucocorticoid hormones because of Addison's disease (Mineura et al, 1987). In turn, glucocorticoid resistance is a common correlate of stress-induced HPA axis activation in animals and humans (Raison and Miller, 2003). Taken together with the aforementioned studies, our work suggests that glucocorticoid resistance may be present in the acute and severe phases of a psychosis. Stress-induced HPA axis activation in this sample could represent a consequence of the distress and arousal associated with the psychotic experience; or, alternatively, it could represent an increased activation of the stress response preceding the development of psychosis, for an increased susceptibility to daily life stress, an increased level of independent stressors, or both (Bebbington et al, 1993; Myin-Germeys et al, 2001). This cross-sectional study does not allow a clarification of this point; however, our recent data showing enlarged pituitary volume preceding the onset of psychosis, in a group of subjects at ultra-high risk of developing psychosis, seem to support the latter model (Garner et al, 2005).
This work has been conducted in Southeast London, an urban region with a large proportion of migrants, deprived areas, and a high incidence of psychosis (Boydell et al, 2001; Boydell et al, 2003). Previous studies have identified environmental risk factors for schizophrenia, like urban place of birth (Pedersen and Mortensen, 2001) and neighborhood environment (van Os et al, 2000), which support the link between a stressful environment and the development of psychosis. Furthermore, cannabis abuse has been identified as a risk factor for schizophrenia (Arseneault et al, 2004), and activation of the hormonal stress response by cannabis could also participate to this phenomenon (D'Souza et al, 2004; D'Souza et al, 2005). Indeed, this sample may be at a higher risk of presenting all these environmental risk factors: for example, approximately 50% of these patients were currently using or abusing cannabis at the time of the study (unpublished data). Since the controls are from the same sociodemographic areas, the increased pituitary volume seems to be an effect of the psychosis and not simply of the ‘stressful environment’. In fact, data from the 2000 British Crime Survey show that approximately 50% people aged 16–29 years in London have used cannabis at least once in their lifetime, and 31% of men and 22% of women in this age range have used cannabis in the previous year (London Health Observatory; www.lho.org.uk). Moreover, we have already described the increased pituitary volume in another sample of first-episode psychosis from a completely different sociodemographic context in Melbourne (Australia), thus indicating that this finding is independent of environmental risk factors (Pariante et al, 2004). Nevertheless, quantitative differences in pituitary volume—the 22% increase compared to controls in this sample vs the 10% increase in Melbourne—could be interpreted as showing a larger contribution of environmental risk factors to the development of psychosis in this sample.
Two lines of evidence further support our conclusions. First, the effects of age and gender on pituitary volumes in our sample are consistent with our and other previously published studies in young adults (Elster, 1993; Lurie et al, 1990; Pariante et al, 2004), thus confirming the reliability of our methods. Second, the most common causes of increased pituitary volume—administration of exogenous estrogens, hypothalamic tumour, pregnancy, and primary hypothyroidism (Elster, 1993)—are excluded in our subjects. A possible limitation of our study, common to all studies examining pituitary volume by imaging methods, is the difficulty in distinguishing between anterior and posterior pituitary volumes. However, the posterior pituitary, which releases vasopressin and oxytocin, comprises less than 20% of the total pituitary volume; moreover, there are no known conditions associated with posterior pituitary enlargement, except tumours. Therefore, we believe that the changes in volume we have described are due to changes in the volume of the anterior pituitary. We did not measure hormonal levels in this sample, nor did we control for menstrual cycle in female patients. Although an increased production of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) during puberty and the menstrual cycle has been implicated in the enlarged pituitary volume in female subjects, these hormones seem to be reduced in female psychotic patients, independently from the effects of antipsychotics (Bergemann et al, 2005; Huber et al, 2001). Moreover, all statistical comparisons are adjusted for gender. Therefore, we would exclude that the differences in pituitary volume between groups are influenced by differences in the phase of menstrual cycle. However, our next studies on this topic will have to include hormone measurements and recording of the menstrual phase.
In conclusion, we have found that the first-episode of a psychotic disorder is associated with a larger pituitary, independently of antipsychotic treatment. These findings support the presence of an activation of the hormonal stress response during a first-episode of psychosis. Future studies should examine whether measurement of the pituitary volume (or of other indicators of the hormonal stress response) can increase our ability to predict the occurrence and the course of a first-episode of psychosis.
References
Arseneault L, Cannon M, Witton J, Murray RM (2004). Causal association between cannabis and psychosis: examination of the evidence. Br J Psychiatry 184: 110–117.
Asa SL, Kovacs K, Hammer GD, Liu B, Roos BA, Low MJ (1992). Pituitary corticotroph hyperplasia in rats implanted with a medullary thyroid carcinoma cell line transfected with a corticotropin-releasing hormone complementary deoxyribonucleic acid expression vector. Endocrinology 131: 715–720.
Axelson DA, Doraiswamy PM, Boyko OB, Rodrigo EP, McDonald WM, Ritchie JC et al (1992). In vivo assessment of pituitary volume with magnetic resonance imaging and systematic stereology: relationship to dexamethasone suppression test results in patients. Psychiatry Res 44: 63–70.
Banki CM, Bissette G, Arato M, O'Connor L, Nemeroff CB (1987). CSF corticotropin-releasing factor-like immunoreactivity in depression and schizophrenia. Am J Psychiatry 144: 873–877.
Bebbington P, Wilkins S, Jones P, Foerster A, Murray R, Toone B et al (1993). Life events and psychosis. Initial results from the Camberwell Collaborative Psychosis Study. Br J Psychiatry 162: 72–79.
Bergemann N, Mundt C, Parzer P, Jannakos I, Nagl I, Salbach B et al (2005). Plasma concentrations of estradiol in women suffering from schizophrenia treated with conventional versus atypical antipsychotics. Schizophr Res 73: 357–366.
Boydell J, van Os J, Lambri M, Castle D, Allardyce J, McCreadie RG et al (2003). Incidence of schizophrenia in south-east London between 1965 and 1997. Br J Psychiatry 182: 45–49.
Boydell J, van Os J, McKenzie K, Allardyce J, Goel R, McCreadie RG et al (2001). Incidence of schizophrenia in ethnic minorities in London: ecological study into interactions with environment. BMJ 323: 1336–1338.
Carey RM, Varma SK, Drake Jr CR, Thorner MO, Kovacs K, Rivier J et al (1984). Ectopic secretion of corticotropin-releasing factor as a cause of Cushing's syndrome. A clinical, morphologic, and biochemical study. N Engl J Med 311: 13–20.
Chen HH, Nicoletti M, Sanches M, Hatch JP, Sassi RB, Axelson D et al (2004). Normal pituitary volumes in children and adolescents with bipolar disorder: a magnetic resonance imaging study. Depress Anxiety 20: 182–186.
Coryell W, Tsuang D (1992). Hypothalamic–pituitary–adrenal axis hyperactivity and psychosis: recovery during an 8-year follow-up. Am J Psychiatry 149: 1033–1039.
Cotter D, Pariante CM (2002). Stress and the progression of the developmental hypothesis of schizophrenia. Br J Psychiatry 181: 363–365.
Dazzan P, Morgan KD, Orr KG, Hutchinson G, Chitnis X, Suckling J et al (2005). Different effects of typical and atypical antipsychotics on grey matter in first episode psychosis: the ÆSOP study. Neuropsychopharmacology 30: 765–774.
Dazzan P, Morgan KD, Orr KG, Hutchinson G, Chitnis X, Suckling J et al (2004). The structural brain correlates of neurological soft signs in AESOP first-episode psychoses study. Brain 127: 143–153.
D'Souza DC, Abi-Saab WM, Madonick S, Forselius-Bielen K, Doersch A, Braley G et al (2005). Delta-9-tetrahydrocannabinol effects in schizophrenia: implications for cognition, psychosis, and addiction. Biol Psychiatry 57: 594–608.
D'Souza DC, Perry E, MacDougall L, Ammerman Y, Cooper T, Wu YT et al (2004). The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: implications for psychosis. Neuropsychopharmacology 29: 1558–1572.
Dinan TG (2004). Stress and the genesis of diabetes mellitus in schizophrenia. Br J Psychiatry Suppl 47: S72–S75.
Elster AD (1993). Modern imaging of the pituitary. Radiology 187: 1–14.
Farde L, Hall H, Ehrin E, Sedvall G (1986). Quantitative analysis of D2 dopamine receptor binding in the living human brain by PET. Science 231: 258–261.
Garner B, Pariante CM, Wood SJ, Velakoulis D, Phillips L, Soulsby B et al (2005). Pituitary volume predicts future transition to psychosis in individuals at ultra-high risk of developing psychosis. Biol Psychiatry (in press).
Gertz BJ, Contreras LN, McComb DJ, Kovacs K, Tyrrell JB, Dallman MF (1987). Chronic administration of corticotropin-releasing factor increases pituitary corticotroph number. Endocrinology 120: 381–388.
Halbreich U, Kahn LS (2003). Hormonal aspects of schizophrenias: an overview. Psychoneuroendocrinology 28(Suppl 2): 1–16.
Herz MI, Fava GA, Molnar G, Edwards L (1985). The dexamethasone suppression test in newly hospitalized schizophrenic patients. Am J Psychiatry 142: 127–129.
Huber TJ, Rollnik J, Wilhelms J, von zur MA, Emrich HM, Schneider U (2001). Estradiol levels in psychotic disorders. Psychoneuroendocrinology 26: 27–35.
Kinon BJ, Gilmore JA, Liu H, Halbreich UM (2003). Prevalence of hyperprolactinemia in schizophrenic patients treated with conventional antipsychotic medications or risperidone. Psychoneuroendocrinology 28(Suppl 2): 55–68.
Krishnan KR, Doraiswamy PM, Lurie SN, Figiel GS, Husain MM, Boyko OB et al (1991). Pituitary size in depression. J Clin Endocrinol Metab 72: 256–259.
Kubota T, Hayashi M, Kabuto M, Shirasaki N, Aradachi H, Miyanaga K et al (1992). Corticotroph cell hyperplasia in a patient with Addison disease: case report. Surg Neurol 37: 441–447.
Kunzel HE, Binder EB, Nickel T, Ising M, Fuchs B, Majer M et al (2003). Pharmacological and nonpharmacological factors influencing hypothalamic–pituitary–adrenocortical axis reactivity in acutely depressed psychiatric in-patients, measured by the Dex-CRH test. Neuropsychopharmacology 28: 2169–2178.
Lammers CH, Garcia-Borreguero D, Schmider J, Gotthardt U, Dettling M, Holsboer F et al (1995). Combined dexamethasone/corticotropin-releasing hormone test in patients with schizophrenia and in normal controls: II. Biol Psychiatry 38: 803–807.
Linkowski P, Kerkhofs M, Van Onderbergen A, Hubain P, Copinschi G, L'Hermite-Baleriaux M et al (1994). The 24-hour profiles of cortisol, prolactin, and growth hormone secretion in mania. Arch Gen Psychiatry 51: 616–624.
Lum C, Kucharczyk W, Montanera W, Becker LE (2002). The sella turcica and parasellar region. In: Atlas SW (ed). Magnetic Resonance Imaging of the Brain and Spine. Lippincott, Williams and Wilkins: Philadelphia. pp 1283–1362.
Lurie SN, Doraiswamy PM, Husain MM, Boyko OB, Ellinwood Jr EH, Figiel GS et al (1990). In vivo assessment of pituitary gland volume with magnetic resonance imaging: the effect of age. J Clin Endocrinol Metab 71: 505–508.
MacMaster FP, Kusumakar V (2004). MRI study of the pituitary gland in adolescent depression. J Psychiatr Res 38: 231–236.
Miller DD, Andreasen NC, O'Leary DS, Rezai K, Watkins GL, Ponto LL et al (1997a). Effect of antipsychotics on regional cerebral blood flow measured with positron emission tomography. Neuropsychopharmacology 17: 230–240.
Miller DD, Andreasen NC, O'Leary DS, Watkins GL, Boles Ponto LL, Hichwa RD (2001). Comparison of the effects of risperidone and haloperidol on regional cerebral blood flow in schizophrenia. Biol Psychiatry 49: 704–715.
Miller DD, Rezai K, Alliger R, Andreasen NC (1997b). The effect of antipsychotic medication on relative cerebral blood perfusion in schizophrenia: assessment with technetium-99 m hexamethyl-propyleneamine oxime single photon emission computed tomography. Biol Psychiatry 41: 550–559.
Mineura K, Goto T, Yoneya M, Kowada M, Tamakawa Y, Kagaya H (1987). Pituitary enlargement associated with Addison's disease. Clin Radiol 38: 435–437.
Muck-Seler D, Pivac N, Mustapic M, Crncevic Z, Jakovljevic M, Sagud M (2004). Platelet serotonin and plasma prolactin and cortisol in healthy, depressed and schizophrenic women. Psychiatry Res 127: 217–226.
Myin-Germeys I, van Os J, Schwartz JE, Stone AA, Delespaul PA (2001). Emotional reactivity to daily life stress in psychosis. Arch Gen Psychiatry 58: 1137–1144.
Pariante CM (2003). Depression, stress and the adrenal axis. J Neuroendocrinol 15: 811–812.
Pariante CM, Miller AH (2001). Glucocorticoid receptors in major depression: relevance to pathophysiology and treatment. Biol Psychiatry 49: 391–404.
Pariante CM, Papadopoulos AS, Poon L, Checkley SA, English J, Kerwin RW et al (2002). A novel prednisolone suppression test for the hypothalamic–pituitary–adrenal axis. Biol Psychiatry 51: 922–930.
Pariante CM, Vassilopoulou K, Velakoulis D, Phillips L, Soulsby B, Wood SJ et al (2004). Pituitary volume in psychosis. Br J Psychiatry 185: 5–10.
Pedersen CB, Mortensen PB (2001). Evidence of a dose–response relationship between urbanicity during upbringing and schizophrenia risk. Arch Gen Psychiatry 58: 1039–1046.
Perez RL, Machiavelli GA, Romano MI, Burdman JA (1986). Prolactin release, oestrogens and proliferation of prolactin-secreting cells in the anterior pituitary gland of adult male rats. J Endocrinol 108: 399–403.
Raison CL, Miller AH (2003). When not enough is too much: the role of insufficient glucocorticoid signaling in the pathophysiology of stress-related disorders. Am J Psychiatry 160: 1554–1565.
Rao ML, Gross G, Strebel B, Halaris A, Huber G, Braunig P et al (1994). Circadian rhythm of tryptophan, serotonin, melatonin, and pituitary hormones in schizophrenia. Biol Psychiatry 35: 151–163.
Ryan MC, Collins P, Thakore JH (2003). Impaired fasting glucose tolerance in first-episode, drug-naive patients with schizophrenia. Am J Psychiatry 160: 284–289.
Ryan MC, Flanagan S, Kinsella U, Keeling F, Thakore JH (2004a). The effects of atypical antipsychotics on visceral fat distribution in first episode, drug-naive patients with schizophrenia. Life Sci 74: 1999–2008.
Ryan MC, Sharifi N, Condren R, Thakore JH (2004b). Evidence of basal pituitary–adrenal overactivity in first episode, drug naive patients with schizophrenia. Psychoneuroendocrinology 29: 1065–1070.
Sachar EJ, Kanter SS, Buie D, Engle R, Mehlman R (1970). Psychoendocrinology of ego disintegration. Am J Psychiatry 126: 1067–1078.
Saiardi A, Bozzi Y, Baik JH, Borrelli E (1997). Antiproliferative role of dopamine: loss of D2 receptors causes hormonal dysfunction and pituitary hyperplasia. Neuron 19: 115–126.
Sassi RB, Nicoletti M, Brambilla P, Harenski K, Mallinger AG, Frank E et al (2001). Decreased pituitary volume in patients with bipolar disorder. Biol Psychiatry 50: 271–280.
Segal M, Avital A, Rojas M, Hausvater N, Sandbank S, Liba D et al (2004). Serum prolactin levels in unmedicated first-episode and recurrent schizophrenia patients: a possible marker for the disease's subtypes. Psychiatry Res 127: 227–235.
Tandon R, Mazzara C, DeQuardo J, Craig KA, Meador-Woodruff JH, Goldman R et al (1991). Dexamethasone suppression test in schizophrenia: relationship to symptomatology, ventricular enlargement, and outcome. Biol Psychiatry 29: 953–964.
van Os J, Driessen G, Gunther N, Delespaul P (2000). Neighbourhood variation in incidence of schizophrenia. Evidence for person–environment interaction. Br J Psychiatry 176: 243–248.
Walder DJ, Walker EF, Lewine RJ (2000). Cognitive functioning, cortisol release, and symptom severity in patients with schizophrenia. Biol Psychiatry 48: 1121–1132.
Warner MD, Walker AM, D'Souza DC, Lee D, Nasseri D, Peabody CA (2001). Lower prolactin bioactivity in unmedicated schizophrenic patients. Psychiatry Res 102: 249–254.
Watson S, Gallagher P, Ritchie JC, Ferrier IN, Young AH (2004). Hypothalamic–pituitary–adrenal axis function in patients with bipolar disorder. Br J Psychiatry 184: 496–502.
Westlund KN, Aguilera G, Childs GV (1985). Quantification of morphological changes in pituitary corticotropes produced by in vivo corticotropin-releasing factor stimulation and adrenalectomy. Endocrinology 116: 439–445.
Wing J, Cooper J, Sartorius N (1974). The Measurement and Classification of Psychiatric Symptoms. Cambridge University Press: Cambridge.
Wing J, Sturt E (1978). The PSE-ID-CATEGO System: Supplementary Manual. Medical Research Council: London.
World Health Organisation (1992). The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. WHO: Geneva.
World Health Organisation (1994). Schedules for Clinical Assessment in Neuropsychiatry (SCAN)—Version 2.0. WHO: Geneva.
Acknowledgements
The ÆSOP study was funded by the Medical Research Council (UK). CM Pariante is funded by a Medical Research Council (UK) Clinician Scientist Fellowship, by a NARSAD Young Investigator Award, and by the Guy's & St Thomas' Charitable Foundation. P Dazzan is funded by an NARSAD Young Investigator Award. We also thank the Stanley Medical Research Foundation for their support. Finally, we thank the ÆSOP researchers who helped with the data collection and the patients who took part in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pariante, C., Dazzan, P., Danese, A. et al. Increased Pituitary Volume in Antipsychotic-Free and Antipsychotic-Treated Patients of the Æsop First-Onset Psychosis Study. Neuropsychopharmacol 30, 1923–1931 (2005). https://doi.org/10.1038/sj.npp.1300766
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300766
Keywords
This article is cited by
-
MRI atlas of the pituitary gland in young female adults
Brain Structure and Function (2024)
-
Perturbed iron biology in the prefrontal cortex of people with schizophrenia
Molecular Psychiatry (2023)
-
Imaging the pituitary in psychopathologies: a review of in vivo magnetic resonance imaging studies
Brain Structure and Function (2019)
-
Toward earlier identification and preventative intervention in schizophrenia: evidence from the London Child Health and Development Study
Social Psychiatry and Psychiatric Epidemiology (2016)
-
Biomarkers of a five-domain translational substrate for schizophrenia and schizoaffective psychosis
Biomarker Research (2015)