Abstract
The known angiotensin II (AngII) physiological effect of aldosterone synthesis and secretion is mediated by either Gq/11 proteins or βarrestin1 (βarr1), both of which can couple to its type 1 receptors (AT1Rs), present in adrenocortical zona glomerulosa (AZG) cell membranes. In the present study, we examined the relative potencies of all the currently used in the clinic AT1R antagonist drugs (angiotensin receptor blockers, ARBs, or sartans) at preventing activation of these two signaling mediators (G proteins and βarrs) at the AngII-bound AT1R and, consequently, at suppression of aldosterone in vitro. All ARBs were found to be potent inhibitors of G protein activation at the AT1R. However, candesartan and valsartan were the most potent at blocking AngII-induced βarr activation at this receptor, among the tetrazolo-biphenyl-methyl derivatives, translating into excellent efficacies at aldosterone suppression in H295R cells. Conversely, irbesartan and losartan were largely G protein-selective inhibitors at the AT1R, with very low potency towards βarr inhibition. As a result, they were very weak suppressors of βarr1-dependent aldosterone production in H295R cells. These findings provide important pharmacological insights into the drug class of ARBs and medicinal chemistry insights for future drug development in the field of AngII antagonism.
Similar content being viewed by others
Introduction
Aldosterone is an adrenocortical mineralocorticoid hormone with significant cardiovascular toxicity, as it contributes to hypertension, heart failure and other heart conditions1. It is produced and secreted by the adrenal cortex in response to AngII acting through its AT1Rs, which are endogenously expressed in AZG cells2. AT1R is a G protein-coupled receptor (GPCR) that also signals through G protein-independent pathways, a plethora of which are mediated by the scaffolding actions of βarrs, originally discovered as terminators of GPCR signaling3. We have uncovered such a G protein-independent but βarr1-dependent pathway in AZG cells that underlies the important AngII-elicited physiological effect of aldosterone synthesis and secretion, thereby exacerbating post-myocardial infarction (MI) heart failure progression4,5,6. Importantly, the oldest AT1R-selective antagonist on the market losartan, the prototypic drug in the class of ARBs or sartans, was found completely ineffective at blocking the adrenal βarr1-dependent aldosterone production and hence, at suppressing circulating aldosterone post-MI5. This phenomenon (i.e. failure at suppressing aldosterone) has been observed with several ARBs clinically and is sometimes referred to as “aldosterone breakthrough”7,8,9,10. Given that both G protein-dependent and βarr1-dependent signaling pathways are elicited by the AngII-activated AT1R and contribute to aldosterone synthesis and secretion in AZG cells, we sought to examine, in the present study, the relative potencies of the various ARBs at inhibiting these two signal transducers at the AT1R and, consequently, gauge their efficacies at lowering aldosterone.
Results
ARBs and G protein vs. βarr inhibition at the AT1R
The failure of losartan at suppression of adrenal βarr1-dependent circulating aldosterone observed previously5 prompted us to investigate herein the relative potencies of various ARBs (essentially all the ARBs currently marketed in the US: losartan and its active metabolite EXP3174, candesartan, valsartan, telmisartan, irbesartan, eprosartan, azilsartan and olmesartan) at inhibiting βarr and G protein activation at the AngII-activated AT1R in vitro. Using two different but complementary cell-based assay systems, the proprietary DiscoveRx assay system (Supplemental Figure 1) and the CellKey assay system (Supplemental Figure 2), first we verified that all the ARBs tested are true (neutral) antagonists with no inverse agonist activity whatsoever for either G proteins or βarrs at the human AT1R (Figure 1, A and B). In other words, none of them causes activation of either G proteins or βarrs intrinsically, like AngII or its analog peptide SII (a known βarr-“biased” agonist) do11,12. Figure 1A shows the data from the DiscoveRx assay and Figure 1B the data from the CellKey assay. Of note, the human AT1R showed no constitutive activity in either of these two in vitro assays. Next, we tested the relative potencies of the ARBs at inhibiting βarrs vs. G proteins (early response, ER) at the AngII-bound AT1R with the CellKey system (Figure 2A). G proteins interact with the receptor instantly upon its agonist activation, while βarr activation follows (and terminates G protein activation)4,13. We also corroborated these data with the DiscoveRx assay (Figure 2B). Inhibition efficacy of the AngII-induced G protein activation was also gauged with the Fluorescent Imaging Plate Reader (FLIPR) calcium assay, which measures calcium ion flux into cells, an AT1R signaling effect thought to be mediated exclusively by G proteins14 (Figure 2C). By combining the data from these assays (Figure 2), we were able to calculate relative potencies for βarr and G protein inhibition at the AngII-activated AT1R in vitro (Table 1) and thus, derive a measure of relative “pathway selectivity” (βarr vs. G protein) for the AT1R inhibition each ARB confers in vitro. With regards to the agents that are not biphenyl-tetrazol derivatives, i.e. azilsartan, telmisartan and eprosartan (Figure 3), all are extremely and more or less equally potent at blocking both G proteins and βarrs, thus displaying “zero” selectivity in their AT1R inhibition with respect to one signal transducer over the other (although eprosartan and telmisartan display some degree of “selectivity” for G protein inhibition, unlike azilsartan, which is perfectly “balanced” between the two pathways, Table 1). Focusing on the tetrazolo-biphenyl-methyl derivative chemical subclass of ARBs, which includes all the rest of this drug class's members (Figure 3), first we confirmed the very low potency of losartan at inhibiting βarrs5 (Table 1), placing it at position 2.1 on the “scale of inhibition selectivity” of Figure 4, i.e. selective for G protein inhibition, although its active metabolite EXP317415 is much more potent at inhibiting both signal transducers and less selective for either one (Table 1). Importantly, valsartan and (even more so) candesartan are much more potent at blocking βarrs than at blocking G proteins (Table 1), placing them at positions 0.5 and 0.35 on the “scale of inhibition selectivity”, respectively (Figure 4). This practically means that valsartan is 50% and candesartan 65% selective toward βarr inhibition (over G protein inhibition). In contrast, olmesartan is on the other end of the “selectivity scale”, i.e. to the right of the 1.0 “zero selectivity” mark (Table 1 & Figure 4). Similarly, irbesartan (like losartan) is significantly less potent at blocking βarrs than G proteins, i.e. very selective for G protein inhibition (Table 1), placing it at position 2.54 of the “selectivity scale” (Figure 4). Of note, irbesartan appeared completely ineffective in the FLIPR assay at the standard concentrations used (Figure 2C), which, coupled with its reportedly very low potency at inhibiting phosphoinositide accumulation16,17, suggests this compound might confer unique (G protein-dependent) signaling properties to the AT1R, e.g. it might block G proteins other than Gq [the opposite of what SII has been reported to do18].
Lack of agonist activity of ARBs for AT1R-induced G protein or βarr activation.
(A) Dose-response curves of each drug for βarr activation at the AT1R, based on the DiscoveRx PathHunterTM β-Arrestin assay system. (B) Dose-response curves of each drug for acute G protein or βarr activation derived from the CellKey assay. LOS: Losartan; EXP: EXP3174; TEL: Telmisartan; EPR: Eprosartan; AZI: Azilsartan; OLM: Olmesartan; CAN: Candesartan; VAL: Valsartan; IRB: Irbesartan.
In vitro potency of sartans at blocking AT1R-induced G protein or βarr activation.
(A) Dose-response curves for inhibition of AngII-induced AT1R-βarr binding or for inhibition of AngII-induced AT1R-G protein coupling (early response, ER) for each compound, as derived from the CellKey assay. (B) Dose-response curves of each drug for βarr activation at the AngII-bound AT1R, based on the DiscoveRx PathHunterTM β-Arrestin assay system. (C) AngII-induced G protein inhibition potencies based on the FLIPR calcium assay (Molecular Devices). Los: Losartan; Exp: EXP3174; Tel: Telmisartan; Epr: Eprosartan; Azi: Azilsartan; Olm: Olmesartan; Can: Candesartan; Val: Valsartan; Irb: Irbesartan.
Ranking of “selectivity” for G protein (G prt) or βarr inhibition at the AT1R and association with AT1R-dependent aldosterone suppression.
Ratios <1.0 denote relative selectivity for βarr inhibition (the lower the ratio, the higher the selectivity), ratios >1.0 denote relative selectivity for G protein inhibition (and the higher the ratio, the higher the selectivity), whereas a ratio of 1.0 denotes no selectivity. LOS: losartan; CAN: candesartan; VAL: valsartan; IRB: irbesartan; OLM: olmesartan.
ARBs and AZG βarr1-dependent aldosterone production
Next, we examined what these findings mean for the physiological effect of AT1R-induced, βarr1-dependent aldosterone production. To that end, we utilized the human AZG cell line H295R, which endogenously expresses AT1Rs (but not AT2Rs) and produces and secretes aldosterone in response to AngII2. H295R cells express βarr1 endogenously (but not βarr2)4. By transfecting the cells with adenovirus encoding for full length wild type βarr1 to overexpress it ~4-fold of basal, endogenous levels (data not shown) and using in vitro aldosterone secretion as the readout, we found that candesartan and valsartan are by far the most potent aldosterone secretion inhibitors in vitro (Figure 5A). Olmesartan also displays some limited capability of suppressing secretion but losartan and irbesartan are completely incapable of suppressing SII-induced aldosterone secretion from these cells (Figure 5A). Of note, we used SII instead of AngII as the secretagogue in these experiments in order to examine the effects of the drugs exclusively on the βarr1-dependent component of aldosterone secretion (since AngII stimulates secretion through both G proteins and βarr1, Figure 4)4. Nevertheless, when AngII was used as the stimulus for aldosterone secretion (instead of SII), similar results were observed (data not shown). On the other hand, in H295R cells transfected with a dominant negative βarr1 mutant (V53D βarr1) to inhibit endogenous βarr14, no effect on aldosterone secretion was seen with any agent, as expected, confirming the essential role of βarr1 in AT1R-induced aldosterone production5,6 and that all ARBs are effective, neutral antagonists of G protein-dependent aldosterone secretion (Figure 5B). Consistent with these findings on in vitro secretion, a similar picture was observed when aldosterone synthesis was examined in these cells, as assessed by steroidogenic acute regulatory (StAR) protein induction2,4. StAR is the enzyme that catalyzes the rate-limiting step in adrenocortical steroidogenesis, i.e. uptake of cholesterol, the precursor of all adrenal steroids, from the cytoplasm into the mitochondria to initiate steroid biosynthesis2. When StAR protein levels in βarr1-overxepressing H295R cells were examined, candesartan and valsartan were found again to be the most potent inhibitors of SII-induced StAR upregulation, whereas losartan and irbesartan were completely incapable of reducing SII-induced StAR levels (Figure 6, A and B). Finally, in H295R cells overexpressing the dominant negative βarr1 mutant, again no agent produced any effect on StAR induction, as expected (Figure 6, C and D). Similar results were found when AngII was used as the stimulus for StAR upregulation, instead of SII (data not shown).
Efficacy of ARBs at suppressing in vitro aldosterone secretion from H295R cells.
Aldosterone secretion in vitro by H295R cells stimulated for 6 hrs with 10 μM SII alone (SII) or in the presence of 10 μM of each of the sartans tested (losartan-LOS, valsartan-VAL, candesartan-CAN, olmesartan-OLM, or irbesartan-IRB). (A) Data from cells transfected to overexpress βarr1. Data are shown as % of the response to SII alone. *, p < 0.05, vs. SII, n = 4 independent experiments/treatment. (B) Data from cells transfected to overexpress the dominant negative V53D βarr1 mutant (23). Data are shown as % of the response to SII alone. No significant differences were observed among treatments, nor did SII induce any response, as expected, since endogenous βarr1 is blocked. n = 3 independent experiments/treatment.
Efficacy of ARBs at preventing StAR upregulation in SII-stimulated H295R cells.
(A,B) Western blotting for StAR protein levels in H295R cells transfected to overexpress βarr1 and treated for 6 hrs with 10 μM SII alone (SII) or in the presence of 10 μM of each of the sartans tested. Representative blots of 3 independent experiments are shown in (A), including blots for βarr1 to confirm its overexpression and for GAPDH (glyceraldehyde 3-phosphate dehydrogenase) as loading control and the StAR protein induction (as % of the SII response), as derived by densitometric quantification, is shown in (B). *, p < 0.05, n = 3 independent experiments/treatment. Blots shown have been cropped to fit space requirements and run under the same experimental conditions (same gel) (the full length blots are shown in Supplementary Information). (C,D) Western blotting for StAR protein levels in dominant negative βarr1 mutant-transfected H295R cells and treated as in (A–B). Representative blots are shown in (C), including blots for the dominant negative βarr1 mutant to confirm its overexpression and for GAPDH as loading control and the StAR protein induction (as % of vehicle-no stimulation), as derived by densitometric quantification, is shown in (D). No significant differences were observed among treatments, nor did any treatment cause any induction in StAR levels. Blots shown have been cropped to fit space requirements and run under the same experimental conditions (same gel) (the full length blots are shown in Supplementary Information). n = 3 independent experiments/treatment. LOS: Losartan-; VAL: Valsartan; CAN: Candesartan; OLM: Olmesartan; IRB: Irbesartan.
Consistent with these in vitro findings, in post-MI rats overexpressing βarr1 specifically in their adrenals in vivo, candesartan significantly reduces cardiac fibrosis (Figure 7A) and the adverse remodeling/heart failure-associated markers collagen-1a1 (Figure 7B) and B-type natriuretic peptide (BNP) (Figure 7C), whereas irbesartan fails to do so (Figure 7, A–C). These effects on cardiac morphology/function in vivo are secondary to the effects of these drugs on circulating aldosterone levels19.
In vivo effects of candesartan and valsartan in post-MI rats overexpressing adrenal βarr1.
(A) Trichrome-Masson's staining in myocardial cross-sections from post-MI rats overexpressing βarr1 specifically in their adrenals and treated for 7 days with either vehicle or 10 mg/kg body weight/day candesartan or 40 mg/kg body weight/day irbesartan (all via drinking water). Blue denotes collagen fibers, red denotes muscle fibers and black represents cell nuclei. Representative images are shown from 5–6 rat hearts stained per group, along with staining in sham-operated rat hearts, in which no blue staining was detectable. (B,C) Heart mRNA levels of (B) collagen I (Col1a1) and brain natriuretic peptide (BNP) (C) in these rats at the end of the 7-day drug treatments. Values for post-MI rats receiving AdGFP in their adrenals instead of Adβarr1 (i.e. not overexpressing βarr1 in their adrenals) were used as reference. *, p < 0.05, vs. Candesartan (Adβarr1), n = 5 rat hearts/group.
Discussion
Over the past several years, it has become increasingly apparent that the ARBs are not pharmacologically, therapeutically or clinically interchangeable. Significant differences in their pharmacodynamic and pharmacokinetic properties, as well as in their therapeutic effects have been noted among several members of this drug class15,20. Our present study adds another dimension to their differential pharmacology and physiology: the different potencies at preventing βarr activation by the AT1R, which, in the adrenal cortex, translates into aldosterone production that, in turn, can exacerbate heart disease. Our data suggest that candesartan and valsartan might be the most preferable members of this drug class therapeutically, especially if the condition is complicated by elevated aldosterone levels. In contrast, irbesartan and losartan appear to be very weak inhibitors of βarr1-dependent aldosterone turnover. Of note, EXP1374, the active metabolite of losartan, was found equipotent at blocking G protein and βarr activation by the AngII-bound AT1R, indicating that the pharmacokinetic properties of the ARB compound can play a significant role in its pharmacodynamic and therapeutic attributes.
From a pharmacotherapeutic standpoint, the potential importance of these findings is dual: on one hand, we recently reported, in a separate study, that candesartan and valsartan, contrary to irbesartan and losartan, are very potent suppressors of post-MI, adrenal βarr-dependent hyperaldosteronism in vivo19. The in vitro findings of the present study completely corroborate those in vivo findings and suggest that the potency of each ARB at blocking adrenal βarr1-dependent aldosterone turnover might underlie (at least in part) the therapeutic differences observed with these various ARB drugs clinically (e.g. in the treatment of heart failure)20. On the other hand, the degree to which each ARB prevents βarr1 activation by the AngII-bound adrenocortical AT1R might underlie the “aldosterone breakthrough” phenomenon that often hampers the clinical use of these agents8,9,10. Given that all ARBs appear more or less equally potent at blocking the G protein-dependent component of the AT1R signaling towards aldosterone production in the AZG cells, but display significant differences in their potencies at blocking the βarr1-dependent component, it is quite plausible that the adrenal βarr1-dependent aldosterone production pathway is responsible for the manifestation of the “aldosterone breakthrough” phenomenon upon ARB use, and, the stronger inhibitor of this pathway an ARB drug is, the lower the risk of this side-effect. Based on our present study and if this hypothesis holds true, candesartan and valsartan appear to be the ARBs with the lowest risk for “aldosterone breakthrough” but, obviously, further studies are needed to address this question and confirm this hypothesis.
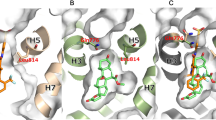
Finally, in terms of structure-activity relationships (SAR) of the biphenyl-tetrazole ARBs (Figure 3), an R1 substitution both bulky and negatively charged on this biphenyl-tetrazolo-backbone (as in candesartan and valsartan) appears to confer strong βarr inhibition at the AT1R, given that losartan and irbesartan with bulky but unionized R1 substitutions are weak βarr inhibitors, as is also olmesartan, whose R1 substitution has a carboxyl-group (i.e. negative charge) but is not bulky. The compound: 2-pentyl-1-({4-[2-(2H-1,2,3,4-tetrazol-5-yl)phenyl]phenyl}methyl)-1H-1,3-benzodiazole-7-carboxylic acid satisfies both of the aforementioned criteria (bulky and anionic R1) and we are currently studying its potency at blocking βarrs at the human AT1R, as well as its aldosterone suppression properties and post-MI cardiac effects in vivo. Of course, these inferences await confirmation upon resolution of the crystal structure of the human AT1R; however, given that all the current SAR data on ARBs are based solely on molecular modeling and pertain exclusively to G protein inhibition at the AT1R, our present findings add another layer of medicinal chemistry information towards a more complete understanding of ARB pharmacology.
Methods
Materials
All drugs were purchased from Selleck Chemicals (Houston, TX, USA), except EXP3174 which was from SantaCruz Biotechnology (Santa Cruz, CA, USA). The peptides AngII and SII were purchased from Pierce Biotechnology, (Rockford, IL, USA).
DiscoveRx assay
The PathHunterTM β-Arrestin® assay monitors the activation of a GPCR in a homogenous, non-imaging assay format using a proprietary complementation technology (Supplemental Fig. 1), developed by DiscoveRx (Fremont, CA, USA)21. Briefly, the assay utilizes an enzyme fragment complementation reaction with β-galactosidase (β-Gal) as the functional reporter. The enzyme is split into two complementary portions expressed as fusion proteins in the cell. The Enzyme Acceptor (EA) is fused to βarr and the ProLink donor peptide is fused to the GPCR of interest, in this case, human AT1R overexpressed in Chinese Hamster Ovary (CHO) cells. Upon GPCR stimulation, βarr is recruited to the receptor for desensitization, bringing the two fragments of β-Gal together and allowing complementation to occur. This generates an active enzyme that can convert a chemiluminescent substrate to generate an output signal detectable on a standard microplate reader.
CellKey assay
This assay utilizes cellular dielectric spectroscopy (CDS) to detect a range of whole-cell responses in a label-free manner. CellKey is a CDS-based instrument that detects GPCR activation in an automated microplate format22. Agonist and antagonist activity can be accurately quantified under conditions of low receptor expression. In the present study, human AT1R-overexpressing human embryonic kidney (HEK)293 cells were used in the CellKey assay system (see also Supplemental Figure 2, A–C). Briefly, cells were incubated with the agent of interest for 40 min at room temperature and the change in impedance was recorded to measure degree of AT1R activation. To measure degree of inhibition of AngII-induced signaling, the change in impedance upon a second challenge with 5 nM AngII for 10 min, immediately following agent washout from the previous treatment, was recorded.
FLIPR assay
The FLIPR (Fluorescent Imaging Plate Reader) calcium assay utilizes a calcium-sensitive dye that is absorbed into the cell's cytoplasm during incubation14. Upon ligand-receptor binding, intracellular calcium is released, binding with the dye, thereby increasing fluorescence intensity. The FLIPR assay kit employed in the present study was from Molecular Devices (Sunnyvale, CA, USA) and the assay was performed according to the manufacturer's instructions.
H295R cell culture and transfections
H295R cells were purchased from American Type Culture Collection (Manassas, VA, USA) and cultured as previously described4. Transfection was performed either with Adβarr1, for which adenovirus encoding for GFP (Green Fluorescent Protein, AdGFP) was used as control, or with pcDNA3.1 plasmid encoding for the V53D dominant negative βarr1 mutant, for which empty pcDNA3.1 plasmid served as control for the transfection23. Plasmid transfections were performed using the Lipofectamine 2000 reagent (Invitrogen, Carlsbad, CA, USA).
In vitro aldosterone secretion measurements
In vitro aldosterone secretion in the culture medium of H295R cells was measured by EIA (Aldosterone EIA kit, ALPCO Diagnostics, Salem, NH, USA), as described4,5,6. Data are presented as % of the measurements obtained with SII-treated cells.
Western blotting
Western blots to assess protein levels of StAR (sc-25806, SantaCruz Biotechnology, Santa Cruz, CA, USA), βarr1 (A1CT antibody, a generous gift from Dr. R.J. Lefkowitz, Duke University Medical Center, Durham, NC, USA) and GAPDH (MAB374; Chemicon, Temecula, CA, USA) were done using protein extracts from treated H295R cells, as described previously4. Visualization of western blot signals was performed with Alexa Fluor 680– (Molecular Probes) or IRDye 800CW–coupled (Rockland Inc.) secondary antibodies on a LI-COR infrared imager (Odyssey). Blots for GAPDH (glyceraldehyde 3-phosphate dehydrogenase) were used as loading control and for normalization of the densitometric values of the StAR and βarr1 levels.
Masson-Trichrome staining & real-time PCR
Masson-trichrome staining for cardiac fibrosis and real-time PCR for collagen-1a1 (Col-1a1) and BNP were performed as described previously5. Briefly, real time RT-PCR was performed using SYBR® Green Supermix (Bio-Rad) and normalization was done with 18S rRNA levels.
Statistical analyses
Data are generally expressed as mean ± SEM. Unpaired 2-tailed Student's t test and one- or two-way ANOVA with Bonferroni test were generally performed for statistical comparisons, unless otherwise indicated. For most 3-group statistical comparisons Dunnett's test using SAS version 8.2 software was used, as well. For all tests, a p value of <0.05 was generally considered to be significant.
References
Weber, K. T. Aldosterone in congestive heart failure. N. Engl. J. Med. 345, 1689–1697 (2001).
Rainey, W. E., Saner, K. & Schimmer, B. P. Adrenocortical cell lines. Mol. Cell. Endocrinol. 228, 23–38 (2004).
Luttrell, L. M. & Gesty-Palmer, D. Beyond desensitization: physiological relevance of arrestin-dependent signaling. Pharmacol. Rev. 62, 305–330 (2010).
Lymperopoulos, A. et al. An adrenal beta-arrestin 1-mediated signaling pathway underlies angiotensin II-induced aldosterone production in vitro and in vivo. Proc. Natl. Acad. Sci. USA. 106, 5825–5830 (2009).
Lymperopoulos, A. et al. Adrenal beta-arrestin 1 inhibition in vivo attenuates post-myocardial infarction progression to heart failure and adverse remodeling via reduction of circulating aldosterone levels. J. Am. Coll. Cardiol. 57, 356–365 (2011).
Bathgate-Siryk, A. et al. Negative impact of β-arrestin-1 on post-myocardial infarction heart failure via cardiac and adrenal-dependent neurohormonal mechanisms. Hypertension. 63, 404–412 (2014).
Sarzani, R. et al. Plasma aldosterone is increased in class 2 and 3 obese essential hypertensive patients despite drug treatment. Am. J. Hypertens. 25, 818–826 (2012).
Horita, Y., Taura, K., Taguchi, T., Furusu, A. & Kohno, S. Aldosterone breakthrough during therapy with angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers in proteinuric patients with immunoglobulin A nephropathy. Nephrology (Carlton). 11, 462–466 (2006).
Bomback, A. S. & Klemmer, P. J. The incidence and implications of aldosterone breakthrough. Nat. Clin. Pract. Nephrol. 3, 486–492 (2007).
Naruse, M. et al. Aldosterone breakthrough during angiotensin II receptor antagonist therapy in stroke-prone spontaneously hypertensive rats. Hypertension. 40, 28–33 (2002).
Violin, J. D. & Lefkowitz, R. J. Beta-arrestin-biased ligands at seven-transmembrane receptors. Trends Pharmacol. Sci. 28, 416–422 (2007).
Shukla, A. K. et al. Distinct conformational changes in beta-arrestin report biased agonism at seven-transmembrane receptors. Proc. Natl. Acad. Sci. USA. 105, 9988–9993 (2008).
Wei, H. et al. Independent beta-arrestin 2 and G protein-mediated pathways for angiotensin II activation of extracellular signal-regulated kinases 1 and 2. Proc. Natl. Acad. Sci. USA. 100, 10782–10787 (2003).
Sheth, H. et al. A Multiplexed Fluorescent Calcium and NFAT Reporter Gene Assay to Identify GPCR Agonists. Curr. Chem. Genomics Transl. Med. 7, 1–8 (2013).
Michel, M. C., Foster, C., Brunner, H. R. & Liu, L. A systematic comparison of the properties of clinically used angiotensin II type 1 receptor antagonists. Pharmacol. Rev. 65, 809–848 (2013).
Vanderheyden, P. M., Fierens, F. L., De Backer, J. P., Fraeyman, N. & Vauquelin, G. Distinction between surmountable and insurmountable selective AT1 receptor antagonists by use of CHO-K1 cells expressing human angiotensin II AT1 receptors. Br. J. Pharmacol. 126, 1057–1065 (1999).
Vanderheyden, P. M., Fierens, F. L., De Backer, J. P. & Vauquelin, G. Reversible and syntopic interaction between angiotensin receptor antagonists on Chinese hamster ovary cells expressing human angiotensin II type 1 receptors. Biochem. Pharmacol. 59, 927–935 (2000).
Saulière, A. et al. Deciphering biased-agonism complexity reveals a new active AT1 receptor entity. Nat. Chem. Biol. 8, 622–630 (2012).
Lymperopoulos, A. et al. Different potencies of angiotensin receptor blockers at suppressing adrenal βarrestin1-dependent post-myocardial infarction hyperaldosteronism. J. Am. Coll. Cardiol. 64, 2805–2806 (2014).
Eklind-Cervenka, M. et al. Association of candesartan vs losartan with all-cause mortality in patients with heart failure. J. Am. Med. Assoc. 305, 175–182 (2011).
McGuinness, D. et al. Characterizing cannabinoid CB2 receptor ligands using DiscoveRx PathHunter beta-arrestin assay. J. Biomol. Screen. 14, 49–58 (2009).
Peters, M. F. et al. Evaluation of cellular dielectric spectroscopy, a whole-cell, label-free technology for drug discovery on Gi-coupled GPCRs. J. Biomol. Screen. 12, 312–319 (2007).
Ferguson, S. S. et al. Role of beta-arrestin in mediating agonist-promoted G protein-coupled receptor internalization. Science. 271, 363–366 (1996).
Acknowledgements
We thank Prof. R.J. Lefkowitz (Duke Univ. Medical Center, Durham, NC) for the generous gift of the A1CT antibody. This work was supported in part by a Scientist Development Grant from the American Heart Association (AHA #09SDG2010138, National Center) and a Nova Southeastern University's President's Faculty Research and Development Grant (PFRDG) (to A.L.) and NIH grants R37 HL061690, R01 HL085503, P01 HL075443 (Project 2) and P01 HL091799 (to W.J.K.).
Author information
Authors and Affiliations
Contributions
S.D., A.B.S., T.R.V., M.J. and E.S. performed research. P.M. and W.J.K. designed research. A.L. conceived the project, designed and performed research, supervised the project and wrote the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Supplementary Information
Supplementary Information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Dabul, S., Bathgate-Siryk, A., Valero, T. et al. Suppression of adrenal βarrestin1-dependent aldosterone production by ARBs: head-to-head comparison. Sci Rep 5, 8116 (2015). https://doi.org/10.1038/srep08116
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep08116
This article is cited by
-
Allisartan isoproxil reduces mortality of stroke-prone rats and protects against cerebrovascular, cardiac, and aortic damage
Acta Pharmacologica Sinica (2021)
-
Low-dose angiotensin AT1 receptor β-arrestin-biased ligand, TRV027, protects against cisplatin-induced nephrotoxicity
Pharmacological Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.