Abstract
The ATP-binding cassette family of transporter proteins, subfamily B (MDR/TAP), member 1 (ABCB1) (P-glycoprotein) transporter is a key component of the blood–brain barrier. Many antidepressants are subject to ABCB1 efflux. Functional polymorphisms of ABCB1 may influence central nervous system bioavailability of antidepressants subject to efflux. Single-nucleotide polymorphisms (SNPs) at rs1045642 (C3435T) of ABCB1 have been associated with efflux pump efficiency. This may explain part of the interindividual variation in antidepressant dose needed to remit. Individuals (N=113) with DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition) major depressive disorder (MDD) were treated with escitalopram (ESC) or venlafaxine (VEN) over 8 weeks. The17-item Hamilton Depression Rating Scale was assessed serially, blind to genotype. SNP rs1045642 of ABCB1 along with two SNPs previously reported to be in linkage disequilibrium with it (rs2032582 and rs1128503) were genotyped. Demographic features, clinical features, P450 metabolizer status and 5-HTTLPR (serotonin-transporter-linked promoter region) genotype were controlled for. Carriers of rs1045642 TT needed on average 11 mg of ESC to remit, whereas TC and CC carriers required 24 and 19 mg, respectively (P=0.0001). This equates to a 2.0- (95% confidence interval=1.5–3.4; P<0.001) fold greater ESC dose needed to remit for C carriers compared with TT carriers at rs1045642. Of VEN-treated subjects carrying TT genotype at rs1045642, 73.3% remitted compared with 12.5% for CC genotype (odds ratio=6.69; 95% confidence interval=1.72–25.9, P=0.006). These data suggest that antidepressant dose needed to remit can be predicted by an ABCB1 SNP. This has the potential clinical translation implications for dose selection and remission from MDD.
Similar content being viewed by others
Introduction
ATP-binding cassette family of transporter proteins, subfamily B (MDR/TAP), member 1 (ABCB1) was discovered during the study of chemotherapeutic resistance in hamster cancer cells. The involved permeability glycoprotein was then named the P-glycoprotein.1 Nearly a decade later, the human coding gene was identified on chromosome 7q21.12 and called the multidrug resistance 1 (MDR1) gene.2, 3 It is now known to be a member of a larger ABCB1, which is involved in multidrug resistance.4 ABCB1 has been recently shown to be evenly expressed and functionally protective across the entire human brain.5
As with many other genes, the functions of ABCB1 have been elucidated from the study of abcb1 knockout mice. Such studies demonstrate much greater entry of tracer agent into the cerebrospinal fluid (CSF).6, 7 ABCB1 is also expressed in various other tissues, such as the liver, kidney and intestine, but has greatest expression at the blood–brain barrier (BBB).4 In abcb1 knockout mice, there is an 87-fold greater tracer entry through the BBB and <4-fold greater entry at other tissue sites.8 It appears that ABCB1 has a key role in CNS bioavailability of several psychotropics.9 For example, blockage of ABCB1 by verapamil or cyclosporin A enhances the transport of impiramine across the BBB.10
The importance of ABCB1 in drug bioavailability was emphasized by using human duodenal cells that showed the TT polymorphism of the rs1045642 single-nucleotide polymorphism (SNP) reduced ABCB1 efflux.11 This is a synonymous SNP producing a codon that does not change the expressed amino acid (isoleucine). These data do not easily explain the potential mechanism by which rs1045642 polymorphism may affect ABCB1 bioactivity. It has been suggested that rs1045642 is in linkage disequilibrium (LD) with the nonsynonymous SNP rs2032582 (Ala893Thr/Ser) on ABCB1, raising the possibility that the Thr/Ser variation could be affecting protein function, with rs1045642 merely acting as a ‘tag-SNP’ for it.12, 13, 14 However, many other studies suggest that rs1045642 is not in LD with rs2032582.15, 16, 17, 18, 19, 20, 21, 22, 23 Furthermore, a study of CSF/serum ratios of the anticonvulsant phenobarbitol in 60 patients found that rs1045642 and not rs2032582 influenced the CSF/serum ratio, with TT carriers at rs1045642 having a significantly higher ratio consistent with reduced ABCB1 efflux.24 Lastly, a study of 332 epileptic patients demonstrated that carriers of the TT allele at rs1045642 were more responsive to anticonvulsants, with no association found with rs2032582 polymorphism.15 This association has been replicated in a subgroup of 160 epileptic patients.16 Taken together, these data suggest that the synonymous rs1045642 SNP has functional effects on ABCB1. In a study utilizing cultured human HeLa cell lines, TT genotype at rs1045642 resulted in use of the rarer isoleucine codon (ATT rarer than ATC), altering ABCB1 conformational folding and efflux functioning.25 These data suggest that rs1045642 can affect ABCB1 functionality without changes in amino-acid sequence, and provides a mechanism explanation for the association of rs1045642 polymorphisms to ABCB1 functioning.
Studies with abcb1 knockout mice have demonstrated that citalopram, escitalopram (ESC), paroxetine, sertraline, venlafaxine (VEN), desvenlafaxine, reboxetine, doxepin, amitriptyline and trimipramine are substrates for ABCB1; however, fluoxetine, mirtazapine, bupropion and melperone are not.26, 27, 28, 29, 30, 31 Polymorphisms of the ABCB1 gene are reported to predict selective serotonin re-uptake inhibitor tolerability.32 However, no association with nortriptyline-induced postural hypotension and ABCB1 polymorphisms were shown.33 Three studies have found an association between ABCB1 polymorphisms and improvement on antidepressants subject to ABCB1 efflux.22, 30, 34 Relapse after response (≥50% reduction in 17-item Hamilton Depression Rating Scale (HDRS)) but not remission (HDRS ≤7) is common, making remission the aim in clinical care.35 The aims of this study were to investigate for associations between ABCB1 polymorphisms and antidepressant dose needed to remit in MDD. The primary hypothesis of this study was that polymorphism of rs1045642 would predict dose needed to remit from major depression, with C carriers needing significantly higher doses for remission. The secondary hypothesis was that polymorphism of rs1045642 would predict probability of remission, with TT genotype significantly more likely to remit. Finally, the influence of two ABCB1 SNPs previously described to be in LD with rs1045642 (rs2032582 and rs1128503) were also examined to determine if they were in LD with rs1045642 in this study population.
Methods
Subjects and ratings
Subjects where either of Caucasian (European, recruited from two sites in Australia) or Asian (Han Chinese, recruited from a third site in Singapore) background. Patients 18 years and over with a principal diagnosis of MDD (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria, assessed by semistructured clinical interview) were studied. An HDRS score of ≥18 was required to exclude milder cases of MDD, which may be less medication responsive.36 Patients who had treatment refractory depression (≥3 failed medication trials) were excluded as more aggressive treatments were clinically appropriate. Patients were studied prospectively for 8 weeks with HDRS ratings as the primary outcome. Clinical global impression scales for improvement and severity were used as a secondary outcome measures to guide clinical dose adjustment. Ratings were blinded to genotype. Before commencement, there was a drug washout period (five half-lives of the previous agent) for subjects already receiving an antidepressant. During the first week, all patients received a standard dose of either ESC 10 mg or VEN 75 mg per day. Drug selection was based on patient’s preference of side-effect profile. At weeks 1, 4 and 8 of treatment, doses were adjusted on a clinical basis, with the dose escalated if there was no improvement on the clinical global impression scale, or the dose reduced if problematic side effects emerged (elevation of the UKU side effects scale37 with patient intolerance of the reported side effect). No other psychotropic medications were given and psychotherapy was not commenced during the study period. Genotyping of CYP2D6 and CYP2C19 polymorphisms was conducted to control for metabolized status as a potential confounder for dose needed to remit. In addition, 5-HTTLPR (serotonin-transporter-linked promoter region) genotype was assessed as a potential antidepressant efficacy confounder.38 Three ABCB1 SNPs (rs1045642, rs2032582 and rs1128503) were assayed. The study was approved by an independent research ethics committee (Study 138; The Melbourne Clinic, Richmond, VIC, Australia).
SNP analysis
DNA was extracted from each sample using QIAamp DNA Mini Kit (Qiagen, Melbourne, VIC, Australia) from venous blood or buccal brush samples. Genotype of candidate SNPs was determined by the polymerase chain reaction followed by single primer extension and analysis on a Sequenom Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (Sequenom, San Diego, CA, USA) 384-well genetic analysis system. For the large duplications and deletions of the CYP2D6 gene, as well as determining the 5-HTTLPR genotype, standard long-range polymerase chain reaction was used.
Statistical analysis
Data were analyzed using SPSS (version 19, IBM, Armonk, NY, USA). Intention-to-treat analysis was applied. Repeated-measures analysis of variance was used to determine changes in HDRS scores and antidepressant dose over time by each of three genotypes of the ABCB1 SNPs studied. Genotype-wise differences were examined using a post hoc pairwise analysis with a Bonferroni correction (P=0.017). Logistic regression was used to estimate the odds ratio and 95% confidence intervals for each ABCB1 polymorphism on symptom remission. To examine differences in dose among responders and remitters by ABCB1 genotype, χ2 analysis was performed. The CubeX program39 was applied to detect departures from Hardy–Weinberg equilibrium and estimate pairwise LD measures r2 and D′. SNPs with Hardy–Weinberg equilibrium >0.01 were considered to be in equilibrium. LD was assumed if a pair of SNPs had r2 and D′ values >0.80.
Results
Of 113 subjects screened, 107 were enrolled in the study. Two patients withdrew consent early for undetermined reasons. Seven patients disengaged before either week 4 or 8, preventing remission assessment. Thus, 98 subjects of the 107 enrolled had sufficient data to analyze response, remission, dose and genotype. In all, 57 subjects were prescribed ESC and 41 VEN.
Demographic and clinical variables (including baseline HDRS and duration of episode), CYP2D6 and CYP2C19 metabolizer status and 5-HTTLPR genotype among the three ABCB1 loci studied is displayed in Table 1. Among subjects treated with ESC, there was a significant difference in the mean duration of depressive episode between the three possible rs2032582 genotypes (Table 1). There was also a significant difference between the three possible rs1128503 genotypes and the proportion of female patients in each group (Table 1). However, there were no significant differences among these characteristics between the three rs1045642 genotype groups (Table 1). Importantly, significant ethnic differences by ABCB1 polymorphisms were not observed. Thus, we did not perform analysis stratified by ethnicity. In addition, all three ABCB1 SNPs were in Hardy–Weinberg equilibrium and pairwise LD analysis showed that all three SNPs were at independent loci (r2 and/or D′ <0.80; Table 2). Thus, haplotype analysis was not performed.
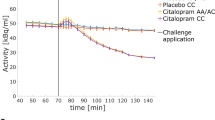
There was a Bonferroni-corrected significant finding for the TT genotype of rs1045642 to better odds of remitting (odds ratio=6.69; 95% confidence interval=1.72–25.9, P=0.006) among subjects treated with VEN but not ESC (Table 3 and Figure 1a). No association between polymorphisms of rs2032582 or rs1128503 to antidepressant remission rate was observed.
Symptom remission and dose needed for remission by ABCB1 genotype. (a) A larger proportion of TT genotype carriers achieve symptom remission with venlafaxine over 8 weeks (*P=0.006). (b) TT genotype carriers required a significantly lower average dose of escitalopram compared with C allele carriers to remit (**P=0.0001). Bars represent standard error of the mean.
There was a Bonferroni-corrected significant association of the TT genotype to a lower average dose of ESC needed to remit for all three ABCB1 SNPs examined (Table 4). Carriers of rs1045642 TT needed on average 11 mg of ESC to remit, whereas TC and CC carriers required 24 and 19mg, respectively (P=0.0001). This equates to a 2.0- (95% confidence interval=1.5–3.4; P<0.001) fold greater ESC dose needed to remit for C carriers compared with TT carriers at rs1045642 (Figure 1b). At rs2032582, TT carriers needed on average 10 mg to remit and TC carriers 22 mg (P=0.008). At rs1128503, TT carriers needed on average 11 mg to remit and TC carriers 23 mg (P=0.0002).
Discussion
These data demonstrate that the ABCB1 rs1045642 polymorphism predicts ESC dose needed for remission controlled for various demographic, clinical and genetic confounders. C carriers at rs1045642 needed a 2.0-fold higher dose of ESC to remit. As 69% of all subjects were C carries at rs1045642, this polymorphism represents a substantial proportion of subjects with translational implications if replicated. As rs1045642 was not in LD with rs2032582 or rs1128503, it does not appear that rs1045642 is acting as a ‘tag-SNP’ to these ABCB1 SNPs, but has a direct association to VEN remission rate and ESC dose needed to remit. Similar findings for ESC dose needed to remit were made for the other two ABCB1 SNPs studied, but with the potential confounder of a significantly different mean duration of depressive episode among the rs2032582 genotypes, and a significant difference in the gender distribution among the rs1128503 genotypes. There were no such potential confounders of baseline features among the three rs1045642 genotypes analyzed for associations to antidepressant dose needed to remit.
The association of rs1045642 polymorphism to dose needed to remit on ESC was not seen for subjects treated with VEN. This may be explained by the longer process of dose titration needed for VEN compared with ESC. During the 8 weeks of the study, it was easier to escalate the dose of ESC to its maximum of 30 mg than to escalate the dose of VEN to its maximum of 450 mg due to the much smaller clinical dose range of ESC. In fact, during the 8 weeks of this study, the highest dose of VEN reached was 300 mg. Some subjects treated with VEN may have been inadvertently under-dosed, with subsequent inadequate CNS bioavailability and reduced remission rates. This may explain why the only significant finding for genotype to remission rate was for subjects treated with VEN, with those carrying the TT allele at rs1045642 showing a significantly greater remission rate. This lower ABCB1 efflux group may have greater CNS bioavailability of VEN at the lower doses reached during this 8-week study, and hence a significantly greater remission rate. Conversely, as ESC could be escalated to an adequate dose faster, C carriers could have their dose escalated to enable adequate CNS bioavailability with no significant remission rate differences between groups discernible. These findings appear to support the hypothesis that C carriers at the rs1045642 may have higher ABCB1 efflux and reduced CNS bioavailability of the antidepressants studied. Furthermore, this suggests that C carriers at rs1045642 treated with VEN could become remitters if their medication dose was escalated further. Longer follow-up could have helped answer this question by enabling greater doses of VEN to be attained.
A strength of this study was controlling for P450 metabolizer status and 5-HTTLPR genotype, both of which may impact the efficacy of antidepressants.38, 40 As serum levels of ESC and VEN will influence CNS bioavailability, not controlling for antidepressant serum levels was a limitation. Trough serum antidepressant level covariance analysis to the ABCB1 SNPs examined could be explored in future studies to help control for this factor. This study analyzed P450 metabolizer status in an attempt to address this issue. Having subject CSF samples would enable a serum to CSF ratio to be determined and correlated to ABCB1 genotype. Such studies are difficult to establish, but they would provide robust evidence of the role of ABCB1 polymorphisms to antidepressant CNS bioavailability. This study would have also benefited from a greater sample size to improve power, but by the same token clinically translatable effect sizes should emerge in moderate samples. A further limitation of this study was not controlling for early life and recent stressors as such seem to influence antidepressant responsiveness putatively by epigenetic mechanisms.41, 42
Previous positive studies demonstrating a significant association between ABCB1 polymorphisms and HDRS score reduction, response and remission22, 30, 32 reflect results akin to the VEN group finding in this study. Namely, that certain ABCB1 genotypes needed a higher dose to remit but were inadequately dosed during the study period, and thus had a significantly lower remission rate than the TT carriers at rs1045642. This study has potential clinical translation and compliments the recent understanding of how synonymous SNPs can have functional outcomes through conformational folding of ABCB1 due to rs1045642 polymorphism.
References
Juliano RL, Ling V . A surface glycoprotein modulating drug permeability in Chinese hamster ovary cell mutants. Biochim Biophys Acta 1976; 455: 152–162.
Chen CJ, Chin JE, Ueda K, Clark DP, Pastan I, Gottesman MM et al. Internal duplication and homology with bacterial transport proteins in the mdr1 (P-glycoprotein) gene from multidrug-resistant human cells. Cell 1986; 47: 381–389.
Callen DF, Baker E, Simmers RN . Localization of the human multiple drug resistance gene, MDR1, to 7q21.1. Hum Genet 1987; 77: 142–144.
Hartz A, Bauer BABC . Transporters in the CNS—an inventory. Curr Pharm Biotechnol 2011; 12: 656–673.
Eyal S, Ke B, Muzi M, Link JM, Mankoff DA, Collier AC et al. Regional P-glycoprotein activity and inhibition at the human blood–brain barrier as imaged by positron emission tomography. Clin Pharmacol Ther 2010; 87: 579–585.
Schinkel AH, Wagenaar E, Mol C, van Deemter L . P-glycoprotein in the blood–brain barrier of mice influences the brain penetration and pharmacological activity of many drugs. J Clin Invest 1996; 97: 2517–2524.
Karlsson L, Schmitt U, Josefsson M, Carlsson B, Ahlner J, Bengtsson F et al. Blood–brain barrier penetration of the enantiomers of venlafaxine and its metabolites in mice lacking P-glycoprotein. Eur Neuropsychopharmacol 2010; 20: 632–640.
Rao VV, Dahlheimer JL, Bardgett ME, Snyder AZ, Finch RA, Sartorelli AC et al. Choroid plexus epithelial expression of MDR1 P glycoprotein and multidrug resistance-associated protein contribute to the blood–cerebrospinal–fluid drugpermeability barrier. Proc Natl Acad Sci USA 1999; 96: 3900–3905.
Linnet K, Ejsing TB . A review on the impact of P-glycoprotein on the penetration of drugs into the brain. Focus on psychotropic drugs. Eur Neuropsychopharmacol 2008; 18: 157–169.
O’Brien FE, Clarke G, Fitzgerald P, Dinan TG, Griffin BT, Cryan JF . Inhibition of P-glycoprotein enhances transport of imipramine across the blood–brain barrier: microdialysis studies in conscious freely moving rats. Br J Pharmacol 2012; 166: 1333–1343.
Hoffmeyer S, Burk O, von Richter O, Arnold HP, Brockmoller, Johne A et al. Functional polymorphisms of the human multidrug-resistance gene: multiple sequence variations and correlation of one allele with P-glycoprotein expression and activity in vivo. Proc Natl Acad Sci USA 2000; 97: 3473–3478.
Xu P, Jiang ZP, Zhang BK, Tu JT, Li HD . Impact of MDR1 haplotypes derived from C1236T,G2677T/A and C3435T on the pharmacokinetics of single-dose oral digoxin in healthy chinese volunteers. Pharmacology 2008; 82: 221–227.
Tang K, Ngoi SM, Gwee PC, Chua JM, Lee EJ, Chong SS et al. Distinct haplotype profiles and strong linkage disequilibrium at the MDR1 multidrug transporter gene locus in three ethnic Asian populations. Pharmacogenetics 2002; 12: 437–450.
Kim RB, Leake BF, Choo EF, Dresser GK, Kubba SV, Schwarz UI et al. Identification of functionally variant MDR1 alleles among European Americans and African Americans. Clin Pharmacol Ther 2001; 70: 189–199.
Sayyah M, Kamgarpour F, Maleki M, Karimipoor M, Gharagozil K, Shamshiri AR . Association analysis of intractable epilepsy with C3435T and G2677T/A ABCB1 gene polymorphisms in Iranian patients. Epileptic Disord 2011; 13: 155–165.
Haerian BS, Lim KS, Mohamed EHM, Tan HJ, Tan CT, Raymond AA et al. Lack of association of ABCB1 haplotypes on five loci with response to treatment in epilepsy. Seizure 2011; 20: 546–553.
Milojkovic M, Stojnew S, Jovanovic I, Ljubisavljevic S, Stefanovic V, Sunder-Plassman R . Frequency of the C1236T, G2677T/A and C3435T MDR1 gene polymorphisms in the Serbian population. Pharmacol Rep 2011; 63: 808–814.
Sipeky C, Csongei V, Jaromi L, Safrany E, Maasz A, Takacs I et al. Genetic variability and haplotype profile of MDRI (ABCB1) in Roma and Hungarian population samples with a review of the literature. Drug Metab Pharmacokinet 2011; 26: 2006–2215.
Drain S, Flannely L, Drake MB, Kettle P, Orr N, Bjourson AJ et al. Multidrug resistance gene expression and ABCB1 SNPs in plasma cell myeloma. Leuk Res 2011; 35: 1457–1463.
Gumus-Akay G, Rustemoglu A, Karadag A, Sunguroglu A . Haplotype-based analysis of MDR1/ABCB1 gene polymorphisms in a Turkish population. DNA Cell Biol 2010; 29: 83–90.
Dong Q, Xu B, Tan Y, Liu Z, Tian L, Zhang B et al. The genetic variability of MDR1 C3435T polymorphisms in four Southern Chinese populations. Biomed Pharmacotherapy 2009; 63: 658–662.
Kato M, Fukuda T, Serretti A, Wakeno M, Okugawa G, Ikenaga Y et al. ABCB1 (MDR1) gene polymorphisms are associated with the clinical response to paroxetine in patients with major depressive disorder. Prog Neuro-Psychol Biol Psych 2008; 32: 398–404.
Jeannesson E, Albertini L, Siest G, Gomes AM, Ribeiro V, Aslanidis C et al. Determination of ABCB1 polymorphisms and haplotypes frequencies in a French population. Fundam Clin Pharmacol 2007; 21: 411–418.
Basic S, Hajnsek S, Bozina N, Filipcic I, Sporis D, Mislov D et al. The influence of C3435T polymorphism of ABCB1 gene on penetration of phenobarbital across the blood–brain barrier in patients with generalized epilepsy. Seizure 2008; 17: 524–530.
Kimchi-Sarfaty C, Oh JM, Kim IW, Sauna ZE, Calcagno AM, Ambudkar SV et al. A ‘silent’ polymorphism in the MDR1 gene changes substrate specificity. Science 2007; 315: 525–528.
Uhr M, Grauer MT, Holsboer F . Differential enhancement of antidepressant penetration into the brain in mice with abcb1ab (mdr1ab) P-glycoprotein gene disruption. Biol Psychiatry 2003; 54: 840–846.
Weiss J, Dormann SMG, Martin-Facklam M, Kerpen CJ, Ketabi-Kiyanvach N, Haefeli WE . Inhibition of P-glycoprotein by newer antidepressants. J Pharmacol Experi Therap 2003; 305: 197–204.
Uhr M, Grauer MT, Yassouridis A, Ebinger M . Blood–brain barrier penetration and pharmacokinetics of amitriptyline and its metabolites in p-glycoprotein (abcb1ab) knock-out mice and controls. J Psychiatr Res 2007; 41: 179–188.
Uhr M, Steckler T, Yassouridis A, Holsboer F . Penetration of amitriptyline, but not of fluoxetine, into brain is enhanced in mice with bloodbrain barrier deficiency due to mdr1a P-glycoprotein gene disruption. Neuropsychopharmacology 2000; 22: 380–387.
Uhr M, Tontsch A, Namendorf C, Ripke S, Lucae S, Ising M et al. Polymorphisms in the drug transporter gene ABCB1 predict antidepressant treatment response in depression. Neuron 2008; 57: 203–209.
Wang J-S, Zhu H-J, Gibson BB, Markowitz JS, Donovan JL, DeVane Cl . Sertraline and its metabolite desmethylsertraline, but not bupropion or its three major metabolites, have high affinity for P-glycoprotein. Biol Pharm Bull 2008; 31: 231–234.
de Klerk OL, Nolte IM, Bet PM, Bosker FJ, Snieder H, den Boer JA et al. ABCB1 gene variants influence tolerance to selective serotonin reuptake inhibitors in a large sample of Dutch cases with major depressive disorder. Pharmacogenomics J (e-pub ahead of print 27 October 2012).
Jensen BP, Roberts RL, Vyas R, Bonke G, Jardine DL, Begg EJ . Influence of ABCB1 (P-glycoprotein) haplotypes on nortriptyline pharmacokinetics and nortriptyline-induced postural hypotension in healthy volunteers. Br J Clin Pharmacol 2012; 73: 619–928.
Lin KM, Chiu YF, Tsai IJ, Ch Chen, Shen WW, Liu SC et al. ABCB1 gene polymorphisms are associated with the severity of major depressive disorder and its response to escitalopram treatment. Pharmacogenet Genomics 2011; 21: 163–170.
Nierenberg AA, Wright EC . Evolution of remission as the new standard in the treatment of depression. J Clin Psychiatry 1999; 60: 7–11.
Fournier JC, DeRubeis RJ, Hollon SD, Dimidjian S, Amsterdam JD, Shelton RC et al. Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA 2010; 303: 47–53.
Lingjaerde O, Ahlfors UG, Bech P, Dencker SJ, Elgen K . The UKU side effect rating scale. A new comprehensive rating scale for psychotropic drugs and a cross-sectional study of side effects in neuroleptic-treated patients. Acta Psychiatr Scand Suppl 1987; 334: 1–100.
Porcelli S, Fabbri C, Serretti A . Meta-analysis of serotonin transporter gene promoter polymorphism (5-HTTLPR) association with antidepressant efficacy. Eur Neuropsychopharmacol 2012; 22: 239–258.
Gaunt TR, Rodríguez S, Day INM . Cubic exact solutions for the estimation of pairwise haplotype frequencies: implications for linkage disequilibrium analyses and a web tool ‘CubeX’. BMC Bioinform 2007; 8: 428.
Porcelli S, Drago A, Fabbri C, Gibiino S, Calati R, Serretti A . Pharmacogenetics of antidepressant response. J Psychiatry Neurosci 2011; 36: 87–113.
Keers R, Uher R, Huezo-Diaz P et al. Interaction between serotonin transporter gene variants and life events predicts response to antidepressants in the GENDEP project. Pharmacogenomics J 2011; 11: 138–145.
Nanni V, Uhr R, Danese A . Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: a meta-analysis. Am J Psychiatry 2012; 169: 141–151.
Acknowledgements
Ajeet Singh acknowledges a young investigator grant awarded by The Royal Australian and New Zealand College of Psychiatrists, Healthscope Molecular for providing the genotyping, and also thanks Dr Cameron Osborne and Professor Brian Dean, as well as Dr. Lai Huat Peh, Changi General Hospital, Singapore; and Professor Chay Hoon Tan, Department of Pharmacology, National University of Singapore.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
AB Singh: Self-employed psychiatrist. Casual speaker for Astra Zeneca Australia, Lilly Australia, Pfizer Australia, Lundbeck Australia. CA Bousman: John McKenzie Post-Doctoral Fellow,The University of Melbourne. Adjunct Research Fellow, Swinburne University of Technology, Centre for Human Psychopharmacology; Research Fellow, Mental Health Research Institute; and consultant to Abbott. CH Ng: Served in the Wyeth and Eli Lilly Advisory Boards, received research grant support from Wyeth and Lundbeck and speaker honoraria from Bristol-Myers Squibb, Organon, Eli Lilly, GlaxoSmithKline, Janssen Cilag, Astra-Zenaca, Wyeth and Pfizer; K Byron: Employee of Healthscope Pathology. M Berk: Professor of Psychiatry, Deakin University, Professorial Research Fellow, Mental Health Research Institute, Orygen Research Centre and the University of Melbourne, consultant to Astra Zeneca, Bristol Meyers Squibb, Eli Lilly, GlaxoSmithKline, Janssen Cilag, Lundbeck and Servier; is on the speaker’s bureau of Astra Zeneca, Bristol Meyers Squibb, Eli Lilly, GlaxoSmithKline, Janssen Cilag, Lundbeck, Pfizer, Sanofi, Synthlabo, Servier, Solvay and Wyeth; has received grant/research support from Astra Zeneca, Beyond Blue, Bristol Meyers Squibb, Eli Lilly, GlaxoSmithKline, Janssen Cilag, Lundbeck, Mayne Pharma, MBF Bioscience, National Health and Medical Research Council, Novartis, Organon, Servier and Stanley Medical Research Foundation; and has received honoraria from Astra Zeneca, Bristol Meyers Squibb, Eli Lilly, GlaxoSmithKline, Janssen Cilag, Lundbeck, Pfizer, Sanofi, Synthlabo, Servier, Solvay and Wyeth.
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Singh, A., Bousman, C., Ng, C. et al. ABCB1 polymorphism predicts escitalopram dose needed for remission in major depression. Transl Psychiatry 2, e198 (2012). https://doi.org/10.1038/tp.2012.115
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tp.2012.115
Keywords
This article is cited by
-
Influence of CYP2B6 activity score on the pharmacokinetics and safety of single dose efavirenz in healthy volunteers
The Pharmacogenomics Journal (2020)
-
Proliferation rates and gene expression profiles in human lymphoblastoid cell lines from patients with depression characterized in response to antidepressant drug therapy
Translational Psychiatry (2016)
-
A common polymorphism in the ABCB1 gene is associated with side effects of PGP-dependent antidepressants in a large naturalistic Dutch cohort
The Pharmacogenomics Journal (2016)
-
Pharmacogenetics and Imaging–Pharmacogenetics of Antidepressant Response: Towards Translational Strategies
CNS Drugs (2016)
-
Systems biology approaches to adverse drug effects: the example of cardio-oncology
Nature Reviews Clinical Oncology (2015)