Abstract
Background
Spirituality/religion is an important factor in health and illness, but more work is needed to determine its link to quality of life in patients with HIV/AIDS.
Objective
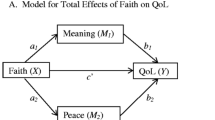
To estimate the direct and indirect effects of spirituality/religion on patients’ perceptions of living with HIV/AIDS.
Design
In 2002 and 2003, as part of a multicenter longitudinal study of patients with HIV/AIDS, we collected extensive demographic, clinical, and behavioral data from chart review and patient interviews. We used logistic regression and path analysis combining logistic and ordinary least squares regression.
Subjects
Four hundred and fifty outpatients with HIV/AIDS from 4 sites in 3 cities.
Measures
The dependent variable was whether patients felt that life had improved since being diagnosed with HIV/AIDS. Spirituality/religion was assessed by using the Duke Religion Index, Functional Assessment of Chronic Illness Therapy—Spiritual Well-Being—Expanded, and Brief RCOPE measures. Mediating factors included social support, self-esteem, healthy beliefs, and health status/health concerns.
Results
Approximately one-third of the patients felt that their life was better now than it was before being diagnosed with HIV/AIDS. A 1-SD increase in spirituality/religion was associated with a 68.50% increase in odds of feeling that life has improved—29.97% due to a direct effect, and 38.54% due to indirect effects through healthy beliefs (29.15%) and health status/health concerns (9.39%). Healthy beliefs had the largest effect on feeling that life had improved; a 1-SD increase in healthy beliefs resulted in a 109.75% improvement in feeling that life changed.
Conclusions
In patients with HIV/AIDS, the level of spirituality/religion is associated, both directly and indirectly, with feeling that life is better now than previously. Future research should validate our new conceptual model using other samples and longitudinal studies. Clinical education interventions should focus on raising awareness among clinicians about the importance of spirituality/religion in HIV/AIDS.
Similar content being viewed by others
References
Dunkel-Schetter C, Feinstein LG, Taylor SE, Falke RL. Patterns of coping with cancer. Health Psychol. 1992;11:79–87.
Davies B, Reimer JC, Brown P, Martens N. Fading Away: the Experience of Transition in Families with Terminal Illness. Arnityville: Baywood: 1995.
Idler EL. Religion, health, and nonphysical senses of self. Social Forces. 1995;74:683–704.
Ellison CG, Levin JS. The religion-health connection: evidence, theory, and future directions. Health Educ Behav. 1998;25:700–20.
Meraviglia MG. The effects of spirituality on well-being of people with lung cancer. Oncol Nurs Forum. 2004;31:89–94.
Pargament KI, Smith B, Koenig HG. Patterns of positive and negative religious coping with major life stressors. J Sci Study Religion. 1998;37:710–24.
Pargament KI, Koenig HG, Tarakeshwar N. Negative Religious Coping Predicts Mortality Among the Medically Ill. Annual Meeting of the American Psychological Association. Washington, DC: American Psychological Association; 2000.
Pargament KI, Tarakeshwar N, Ellison CG, Wulff KM. Religious coping among the religious: the relationships between religious coping and well-being in a national sample of Presbyterian clergy, elders, and members. J Sci Study Religion. 2001;40:497–514.
McCullough ME. Research on religion-accommodative counseling: review and meta-analysis. J Counsel Psychology, 1999;46:1–7.
McCullough ME, Hoyt WT, Larson DB, Koenig HG, Thoresen C. Religious involvement and mortality: a meta-analytic review. Health Psychol. 2000;19:211–22.
Hill PC, Pargament KI. Advances in the conceptualization and measurement of religion and spirituality. Implications for physical and mental health research. Am Psychol. 2003;58:64–74.
Miller WR, Thoresen CE. Spirituality, religion, and health, An emerging research field. Am Psychol. 2003;58:24–35.
Centers for Disease Control and Prevention. HIV/AIDS among Hispanics in the United States. Available at: http://www.cdc.gov/hiv/pubs/facts/hispanic.htm. Accessed June 26. 2004.
Pargament KI, McCarthy S, Shah P, et al. Religion and HIV a review of the literature and clinical implications. South Med J 2004;97:1201–9.
Kaldjian LC, Jekel JF, Friedland G. End of life decisions in HIV positive patients: the role of spiritual beliefs. AIDS 1998;12:103–7.
Lorenz KA, Hays RD, Shapiro MF, Cleary PD, Asch SM, Wenger NS. Religiousness and spirituality among HIV-infected Americans. J Palliat Med. 2005;8:774–81.
Ironson G, Solomon GF, Balbin EG, et al. The Ironson-Woods Spirituality/Religiousness Index is associated with long survival, health behaviors, less distress, and low cortisol in people with HIV/AIDS. Ann Behav Med. 2002;24:34–48.
Tsevat J, Sherman SN, McElwee JA, et al. The will to live among HIV-infected patients. Ann Intern Med. 1999;131:194–8.
Honiden S, Sundaram V, Nease RF, et al. The effect of diagnosis with HIV infection on health-related quality of life. Qual Life Res. 2006;15:69–82.
Belcher AE, Dettmore D, Holzemer SP. Spirituality and sense of well-being inpersons with AIDS. Holist Nurs Pract. 1989;3:16–25.
Klitzman R. The Lives of Men and Women with HIV. Chicago: Ivan R. Dee; 1997.
World Health Organization. Adherence to Long-Term Therapies: Evidence for Action. Geneva, Switzerland: World Health Organization; 2003.
Beckley RE, Koch JR. The Continuing Challenge of AIDS: Clergy Responses to Patients, Friends, and Families. Westport: Auburn House; 2002.
Sowell R, Moneyham L, Hennessy M, Guillory J, Demi A, Seals B. Spiritual activities as a resistance resource for women with human immunodeficiency virus. Nurs Res. 2000;49:73–82.
Peterman AH, Fitchett G, Cella DF. Modeling the Relationship Between Quality of Life Dimensions and an Overall Sense of Well Being. New York: Third World Congress of Psycho-oncology; 1996.
Koenig H, Parkerson GR Jr, Meador KG. Religion index for psychiatric research. Am J Psychiatry, 1997;154:885–6.
Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: the Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being scale (FACIT-Sp). Ann Behav Med. 2002;24:49–58.
Pargament KI, Koenig HG, Perez LM. The many methods of religious coping: development and initial validation of the RCOPE. J Clin Psychol. 2000;56:519–43.
Brown TA. Confirmatory Factor Analysis for Applied Research. New York: Guilford Press; 2006.
Holmes WC, Shea JA. A new HIV/AIDS-targeted quality of life (HAT-QoL) instrument: development, reliability, and validity. Med Care. 1998;36:138–54.
Justice A, Holmes W, Gifford A, et al. Development and validation of a self-completed HIV symptom index. J Clin Epidemiol. 2001;54(suppl 1): S77–90.
Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10:77–84.
Kilbourne AM, Justice AC, Rollman BL, et al. Clinical importance of HIV and depressive symptoms among veterans with HIV infection. J Gen Intern. Med. 2002;17:512–20.
Chesney MA, Ickovics JR, Chambers DB, et al. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: the AACTG adherence instruments. Patient Care Committee & Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG). AIDS Care. 2000;12:255–66.
Cohen S, Mermelstein R, Kamarck T, Hoberman S Measuring the functional components of social support. In: Sarason I, Sarason B, eds. Social Support: Theory, Research and Applications. The Hague: Martinus Nijhoff: 1985;73–94.
Robinson J, Shaver P. Measuring Social Psychological Attitudes. Ann Arbor: Institute for Social Research; 1969.
Scheier M, Carver C. Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health Psychol. 1985;4:219–47.
Kline RB. Principles and Practice of Structural Equation Modeling. 2nd ed. New York: Guilford Press; 2005.
Pedhazur EJ. Multiple Regression in Behavioral Research: Explanation and Prediction. 3rd ed. Fort Worth: Harcourt Brace College Publishers: 1997.
Mickley JR, Soeken K, Belcher A. Spiritual well-being, religiousness and hope among women with breast cancer. Image J Nurs Sch. 1992;24:267–72.
Mickley J, Soeken K. Religiousness and hope in Hispanic- and Anglo-American women with breast cancer. Oncol Nurs Forum. 1993; 20:1171–7.
Cotton SP, Levine EG, Fitzpatrick CM, Dold KH, Targ E Exploring the relationships among spiritual well-being quality of life, and psychological adjustment in women with breast cancer, Psycho-oncology. 1999;8: 429–38.
Bourjolly JN. Differences in religiousness among black and white women with breast cancer. Soc Work Health Care. 1998;28:21–39.
Idler EL, Kasl SV. Religion among disabled and nondisabled persons II: attendance at religious services as a predictor of the course of disability. J Gerontol B Psychol Sci Soc Sci. 1997;52:S306–16.
Simoni JM, Ortiz MZ. Mediational models of spirituality and depressive symptomatology among HIV-positive Puerto Rican women. Cultur Divers Ethnic Minor Psychol. 2003;9:3–15.
McCullough ME, Laurenceau JP. Religiousness and the trajectory of self-rated health across adulthood. Pers Soc Psychol Bull. 2005;31: 560–73.
Folkman S. Positive psychological states and coping with severe stress. Soc Sci Med. 1997;45:1207–21.
Schwartz CE, Sprangers MAG. Adaptation to Changing Health: Response Shift in Quality-of-Life Research. Washington, DC: American Psychological Association; 2000.
Beaton DE, Tarasuk V, Katz JN, Wright JG, Bombardier C “Are you better?” A qualitative study of the meaning of recovery. Arthritis Rheum. 2001;45:270–9.
Elliott AM, Smith BH, Hannaford PC, Smith WC, Chambers WA. Assessing change in chronic pain severity: the chronic pain grade compared with retrospective perceptions. Br J Gen Pract. 2002;52:269–74.
Guyatt GH, Norman GR, Juniper EF, Griffith LE. A critical look at transition ratings. J Clin Epidemiol. 2002;55:900–8.
Fischer D, Stewart AL, Bloch DA, Lorig K, Laurent D, Holman H. Capturing the patient’s view of change as a clinical outcome measure. JAMA. 1999;282:1157–62.
Association of American Medical Colleges. Report III of the medical school objectives project. Contemporary issues in medicine: communication in medicine; 1999.
Barnett KG, Fortin AH. Spirituality and medicine. A workshop for medical students and residents. J Gen Intern Med. 2006;21:481–5.
JCAHO. Spiritual Assessments. Availabic at: http://www.jointcommission.org/AccreditationPrograms/HomeCare/Standards/FAQs/Provision+of+Care /Assessment/Spiritual_Assessment.htm. Accessed August 10, 2006.
Puchalski C. Spirituality in health: the role of spirituality in critical care. Crit Care Clin. 2004;20:487–504.
Puchalski C, Romer AL. Taking a spiritual history allows clinicians to understand patients more fully. J Palliat Med. 2000;3:129–37.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no conflicts of interest to report.
Rights and permissions
About this article
Cite this article
Szaflarski, M., Ritchey, P.N., Leonard, A.C. et al. Modeling the effects of spirituality/religion on patients’ perceptions of living with HIV/AIDS. J GEN INTERN MED 21 (Suppl 5), S28–S38 (2006). https://doi.org/10.1111/j.1525-1497.2006.00646.x
Issue Date:
DOI: https://doi.org/10.1111/j.1525-1497.2006.00646.x