Abstract
In this work, we describe the synthesis of 5-(perylen-3-ylethynyl)uridine and its ability to effectively inhibit the replication of respiratory disease pathogens in cell culture, namely: influenza A virus (IVA); type 3 parainfluenza virus (PIV-3); and human respiratory syncytial virus (RSV). Related known compounds were also analyzed: 5-(perylen-3-ylethynyl)-2′-deoxy-uridine; 5-(perylen-3-ylethynyl)-arabino-uridine; and 1-carboxymethyl-3-pivaloyloxymethyl-5-(perylen-3-ylethynyl)uracil.
Similar content being viewed by others
INTRODUCTION
Respiratory diseases are a significant problem affecting the health of the world’s population. One of the most dangerous among them is the influenza virus, which causes annual epidemics (about one billion cases, up to 5 million of which are severe, and 0.65 million deaths) [1, 2]. Historically, it has caused several global pandemics, including the 1918 ‘Spanish flu,’ which killed about 50 million people [3]. The epidemiological danger surrounding the influenza virus lies in its high mutational variability and the diversity of its environmental routes of circulation [4].
Although the pharmaceutical market is filled with a variety of cold and flu products, most are directed at symptoms, and few feature any direct inhibitory effect on the pathogen. Three groups of antiviral drugs are etiotropic: M2-channel blockers (amantadine, remantadine); neuraminidase inhibitors (oseltamivir, zanamivir); and protease inhibitors (baloxavir marboxil and faviperavir). Drugs in the first group have now lost their potential as influenza agents due to high resistance to them among circulating strains [5]. Drugs in the second group are still the most effective, but the emergence and spread of resistant strains is possible. For example, in 2008, 68% of influenza A (H1N1) virus isolates in Norway were resistant to oseltamivir [6]. The third group of anti-influenza agents is not yet registered in Russia. It should be noted that all three groups of drugs, as well as the latest drugs under development [7], are aimed at protein targets.
Although they cause less mortality than the influenza virus, the parainfluenza (PIV) and respiratory syncytial (RSV) viruses are nevertheless dangerous. High-risk patients (preschool children, the elderly, persons with immune disorders) are especially vulnerable. There are no etiotropic drugs to treat illness caused by these pathogens, only symptomatic treatments. Thus, there is an urgent need to develop new, effective means of respiratory virus control. Preparations featuring entirely new mechanisms of action, relative to existing drugs, are of special interest.

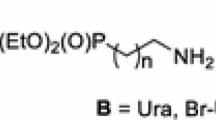
Previously, we found that perylene derivatives of uracil nucleosides dUY11 (I) and aUY11 (II) are highly active against a broad spectrum of enveloped viruses: herpes simplex type 1 and type 2; Sindbis; hepatitis C; vesicular stomatitis [8–11]; tick-borne encephalitis [12]; African swine fever [13]; and the influenza A virus serotypes H1N1 and H3N2 [10]. Despite the formal nucleoside structure, there is evidence in favor of a ‘non-nucleoside’ mechanism of antiviral action of substances (I) and (II). Two main hypotheses have been proposed: (1) introduction of the drug into the virion lipid membrane causing mechanical disturbance of its rheological properties, which, in turn, leads to inhibition of penetration of viral genetic material into the cell (of the act of fusion of virion and cell lipid membranes) [9–11]; (2) drug-mediated photosensitized generation of singlet oxygen, oxidizing unsaturated lipids in virion membrane, which has no systems for membrane reparation [15]. Both hypotheses explain the broad spectrum activity of perylene derivatives against enveloped viruses, have consensus on the target (virion outer lipid membrane), and imply pharmacophoric importance of the perylene part of the molecule. Indeed, the carbohydrate fragment in such compounds is not a necessary precondition for antiviral activity. Recently, we have demonstrated the activity of a non-nucleoside derivative of cm1pUY11 (III) against enveloped viruses herpes simplex type 1 [11] and tick-borne encephalitis [14]. Thus, the lipid nature of the proposed antiviral target of perylene derivatives fundamentally distinguishes them from the three aforementioned groups of influenza drugs.
Ribonucleoside (IV) has not been previously described. Nor has the antiviral activity of perylene compounds, in relation to other respiratory viruses, been tested previously. The aim of this work was to synthesize the ribo derivative (IV) and to obtain data on the antiviral activity of compounds (I)–(IV) in relation to the influenza A virus and two other respiratory pathogens: type 3 parainfluenza virus and respiratory syncytial virus.
RESULTS AND DISCUSSION
Compound (IV) was prepared in four steps from uridine (V) (Scheme 1). Perylenylethynyl nucleoside derivatives have low solubility in most solvents, which makes it difficult to purify them using column chromatography. Therefore, acylic protection of hydroxyl groups of the carbohydrate fragment is usually applied, which allows to increase the solubility of the sp–sp2 coupling product and to carry out its chromatographic purification after this step [8, 11, 15, 16]. The isobutyryl group was chosen as such a protective group. Acylation of uridine with isobutyric anhydride resulted in 2′,3′,5′-O-acyl nucleoside (VI), which was further halogenated into a 5-iodo derivative (VII). The latter was alkynylated with 3-ethynylperylene under Sonogashira reaction conditions to afford a product (VIII), which had sufficient solubility for facile purification by means of silica gel column chromatography. To remove the protective groups, compound (VIII) was subjected to alkaline hydrolysis under mild conditions to yield the desired ribonucleoside rUY11 (IV). As with other perylenethynyl derivatives of nucleosides, compound (IV) is only slightly soluble in water but fairly soluble in DMSO. Solutions of compound (IV) feature the bright yellow-green fluorescence characteristic of perylenylethynyluracil derivatives.

Scheme 1. Reagents and reaction conditions: (i) isobutyric anhydride, 4-dimethylaminopyridine (DMAP), pyridine, 83%; (ii) iodine, ammonium-cerium(IV) nitrate (CAN), acetonitrile, 80°C, 93%; (iii) 3-ethynylperylene, tetrakis(triphenylphosphine)palladium(0), copper(I) iodide, triethylamine, DMF, 78%; (iv) potassium carbonate, methanol, 85%.
For compounds (I)–(IV), antiviral activity was tested in vitro against influenza A, human parainfluenza type 3, and respiratory syncytial virus. Data on their antiviral activity and cytotoxicity are given in Table 1.
It can be seen, from the data presented in Table 1, that the cytotoxicities of the preparations in both cell cultures were generally similar. At the same time, three of the four studied compounds feature low toxicity in cell cultures (CC50 in the range 492–998 µM), while the non-nucleoside compound cm1pUY11 (III) showed significantly more pronounced cytotoxic properties; this is probably due to the presence of the pivaloyloxymethyl group, which may hydrolyze to free pivalate, thus inhibiting L-carnitine metabolism in cells [17].
The EC50 values for all drugs were also similar and ranged from 0.5 to 7.1 µM, resulting in high selectivity index (SI) values. For all tested compounds, the SI was higher than the threshold value of 10, which allows considering a preparation promising for further studies, even despite the high values of CC50, as in the case of compound cm1pUY11.
Thus, all of the compounds used in this study can be characterized as having high antiviral activity against influenza, parainfluenza, and respiratory syncytial viruses when tested in vitro using cell cultures.
EXPERIMENTAL SECTION
All solvents and reagents were used without additional purification. 3-Ethynylperylene [8, 18], as well as compounds (I) [8], (II) [9, 19] and (III) [14], were synthesized as described previously. 1H and 13C NMR spectra were recorded with the Bruker Avance III 500 MHz NMR spectrometer with signal attribution by residual proton peaks in solvents: CDCl3 (7.26 ppm for 1H and 77.16 ppm for 13C); and DMSO-d6 (2.50 ppm for 1H and 39.52 ppm for 13C). 1H NMR coupling constants are reported in Hertz (Hz) for the respective multiplets. UV spectra were recorded using a Varian Cary 100 spectrophotometer. Fluorescence spectra were recorded using a Perkin Elmer LS 55 spectrometer. Thin layer chromatography was performed on TLC Silica gel 60 F254 (Merck) aluminum plates.
2',3',5'-O-Triisobutyryluridine (VI). To a solution of uridine (5.00 g, 20.48 mmol) and 4-dimethylaminopyridine (20 mg) in dried pyridine (35 mL), isobutyric anhydride (10.2 mL, 61.43 mmol) was added at once. The mixture was stirred at room temperature for 24 h, diluted with methanol (5 mL), and evaporated in a vacuum. The residue was dissolved in dichloromethane (200 mL), and washed with saturated aqueous NaHCO3 (2 × 150 mL) and brine (150 mL). The organic phase was dried with Na2SO4, filtered, and evaporated in a vacuum. The residue was purified by column chromatography on silica gel (0 → 2% methanol in dichloromethane, (vol)), and compound (VI) (7.72 g, 83%) was obtained as a white foam. Rf 0.65 (n‑hexane–ethyl acetate, 1 : 1 (vol)). 1H NMR (500 MHz, CDCl3): δ 9.26 (s, 1H), 7.42 (d, J 8.1, 1H), 6.13–6.04 (m, 1H), 5.77 (d, J 8.2, 1H), 5.33–5.28 (m, 2H), 4.42–4.26 (m, 3H), 2.67–2.49 (m, 3H), 1.26–1.08 (m, 18H). 13С NMR (126 MHz, CDCl3): δ 176.44, 175.83, 175.81, 162.93, 150.29, 139.23, 103.47, 87.16, 80.53, 72.86, 70.23, 63.32, 34.11, 33.86, 33.79, 19.10, 19.05, 18.97, 18.88, 18.82, 18.80.
2',3',5'-O-Triisobutyryl-5-iodouridine (VII). Ammonium-cerium(IV) nitrate (9.17 g, 16.72 mmol) and iodine (2.49 g, 10.03 mmol) were added to a solution of compound (VI) (7.60 g, 16.72 mmol) in dry acetonitrile (210 mL). The reaction mixture was stirred at 80°C for 1 h and evaporated in a vacuum. The residue was dissolved in ethyl acetate (200 mL) and washed with brine (100 mL). The organic phase was separated, washed with 5% aqueous NaHSO3 (100 mL), dried over Na2SO4, filtered, and evaporated to dryness. The residue was purified by column chromatography on silica gel (0 → 1% methanol in dichloromethane (vol)), and compound (VII) (9.00 g, 93%) was obtained as a white foam. Rf 0.75 (n-hexane–ethyl acetate, 1 : 1 (vol)). 1H NMR (CDCl3): δ 9.16 (s, 1H), 7.86 (s, 1H), 6.10 (d, J 5.9, 1H), 5.35–5.25 (m, 2H), 4.44 (dd, J 12.5, 3.1, 1H), 4.36 (q, J 3.0, 1H), 4.30 (dd, J 12.5, 2.4, 1H), 2.74 (p, J 7.0, 1H), 2.59 (dp, J 21.1, 7.0, 2H), 1.26 (dd, J 7.0, 0.8, 6H), 1.19 (dd, J 6.9, 0.9, 6H), 1.15 (d, J 7.0, 6H). 13С NMR (CDCl3): δ 176.49, 175.84, 175.80, 159.69, 149.99, 143.63, 86.89, 80.96, 73.14, 70.28, 69.80, 63.22, 34.14, 33.87, 33.78, 19.36, 19.20, 18.97, 18.88, 18.81, 18.78.
2',3',5'-O-Triisobutyryl-5-(perylen-3-ylethynyl)uridine (VIII). To a solution of protected iodide (VII) (280 mg, 0.48 mmol) and 3-ethynylperylene (177 mg, 0.64 mmol) in dry DMF (13 mL), tetrakis(triphenylphosphine)palladium (67 mg, 0.058 mmol), copper(I) iodide (22 mg, 0.12 mmol), and triethylamine (268 µL, 1.93 mmol) were added. The flask was then evacuated and purged with argon three times successively. The reaction mixture was stirred at 35°C for 12 h and evaporated to dryness. The residue was dissolved in ethyl acetate (30 mL), washed with water (20 mL), NaHCO3 saturated water (20 mL), and brine (20 mL). The organic phase was dried over Na2SO4, filtered, and evaporated in a vacuum. The residue was purified by column chromatography on silica gel (toluene ethyl acetate), and compound (VIII) (273 mg, 78%) was obtained in the form of brown foam. Rf 0.55 (n-hexane–ethyl acetate, 2 : 1 (vol)). 1H NMR (DMSO-d6): δ 11.96 (s, 1H), 8.51–8.33 (m, 4H), 8.33–8.23 (m, 2H), 7.90–7.78 (m, 2H), 7.75–7.64 (m, 2H), 7.57 (t, J 7.7, 2H), 5.98 (d, J 4.6, 1H), 5.63–5.51 (m, 1H), 5.43 (s, 1H), 4.37 (s, 3H), 2.69–2.54 (m, 3H), 1.15–1.04 (m,18H). 13С NMR (DMSO-d6): δ 175.79, 174.94, 161.38, 149.32, 143.73, 134.21, 133.84, 131.43, 131.06, 130.60, 130.09, 129.79, 128.76, 128.42, 127.93, 127.81, 127.62, 127.06, 127.02, 125.72, 121.74, 121.49, 121.38, 120.34, 119.19, 99.26, 91.13, 88.22, 88.01, 79.48, 72.50, 69.39, 62.71, 33.22, 33.07, 18.79, 18.69, 18.62, 18.54, 18.51.
5-(Perylen-3-ylethynyl)uridine (IV). One portion of saturated aqueous K2CO3 (2 mL) was added to compound (VIII) solution (250 mg, 0.34 mmol) in pyridine (2 mL). The reaction mixture was stirred for 10 h at 45°C and diluted with water (2 mL). The precipitate was filtered off, washed three times (water 5 mL, ethanol 2 mL, diethyl ether 5 mL), and dried in a vacuum to yield product (IV) (151 mg, 85%) as a brown powder. Rf 0.40 (CH2Cl2–MeOH, 1 : 1 (vol)). 1H NMR (500 MHz, DMSO-d6) δ 8.58–8.21 (m, 6H), 7.82 (d, J 7.7, 2H), 7.74–7.61 (m, 2H), 7.55 (t, J 7.8, 2H), 5.84 (d, J 4.2, 1H), 5.70–4.93 (m, 2H), 4.19–3.97 (m, 2H), 3.89 (d, J 4.5, 1H), 3.83–3.57 (m, 2H). 13С NMR (126 MHz, DMSO-d6): δ 143.53, 134.15, 133.71, 130.81, 130.58, 130.14, 129.99, 129.89, 128.35, 128.15, 127.73, 127.67, 127.56, 126.90, 126.87, 126.04, 121.31, 121.26, 121.06, 120.24, 120.19, 98.81, 98.09, 89.76, 88.94, 84.44, 73.94, 69.28, 60.41. UV (96% EtOH, λmax, nm (ε, М–1 сm–1)): 268 (27800), 291 (25000), 320 (16400), 339 (16000), 369 (12800), 457 (18200), 513 (1600). Fluorescence (96% EtOH, λmax, nm) (excitation 560 nm): 239, 289, 363, 440, 514; (emission 490 nm): 552.
Measurement of Anti-Influenza Activity
MDCK cell culture and influenza virus strain A/PR/8/34 (H1N1) were used in the study. Drugs were dissolved in DMSO (2000 µg/mL) and diluted in culture medium to a concentration corresponding to CC50 (the drug concentration causing 50% cell death). Following that, a series of 3-fold dilutions were prepared from this solution. A virus dilution (corresponding to multiplicity of infection (m.o.i.) = 1) was prepared using culture media.
Cell cultures were washed with media, and experimental drug solutions (100 µL per well) were applied to them at the appropriate concentrations, followed by incubation for 1 h in the dark (CO2 incubator, 37°C, 5% CO2). Virus (in a volume of 100 µL) was then added, followed by incubation for 24 h (37°C, 5% CO2). At the end of the incubation period, 10-fold serial dilutions (10–1–10–7) were prepared from each sample in support medium. These were applied to 1‑day-old monolayers and then incubated for 72 h (37°C, 5% CO2). Viral titers were determined by hemagglutination reaction. For this, culture medium was transferred to the appropriate wells of multi-well plates (U-bottom, immunology grade), and an equal volume of chicken red blood cell suspension (1% in physiological saline) was added. After 40 minutes, the presence or absence of hemagglutination in the wells was visually assessed. Viral titers were calculated using the Reed and Mench method [20] and expressed as 50% tissue infection doses (TID50) per 100 µL volume. Drug antiviral activities were estimated based on decreased viral titers in relation to controls.
Measurement of Antiviral Activity against Parainfluenza Virus and Respiratory Syncytial Virus
HEp-2 cell culture, parainfluenza type 3 strain v2932, and respiratory syncytial virus A2 were used for analysis. Drugs were dissolved in DMSO (2000 µg/mL) and then in culture medium to a concentration corresponding to CC50. Next, a series of 3-fold dilutions were prepared from the initial solution. A series of 10-fold virus dilutions (10–1–10–7) was also prepared in a support medium.
Cell cultures were washed with medium, and drug preparations (in volumes of 200 µL per well) were applied at the appropriate concentrations, followed by incubation for 1 h (37°C, 5% CO2). All culture media were then removed, and drug solutions were added to wells again (100 µL per well at twice the original concentration). Viral suspensions (100 µL) were immediately added, and plates were incubated for 1 h (37°C, 5% CO2). Plates were then washed free of virus, drug solutions were re-applied (at their original concentrations), and plates incubated for 6 days (at 37°C, 5% CO2).
Viral titers were determined using cellular immunoassay (cell-ELISA). For the analysis, cell cultures were fixed with cold 80% acetone for 15 min and washed with PBS-T buffer. Next, a solution of mouse primary antibodies (anti-parainfluenza virus HN protein) was applied and incubated for 2 h at room temperature with continuous stirring, followed by washing with buffer. Secondary antibodies were then applied and incubated again for 2 h with continuous stirring. The antibodies were washed out, and substrate-chromogenic mixture with 3,3′,5,5′-tetramethylbenzidine (TMB) was applied. After 5 min, reactions were stopped with 0.1 M sulfuric acid, and optical densities of the solutions were measured at 450 nm. Presence of infection was defined as sample optical densities exceeding those of the controls. Viral titers were calculated by the Reed and Muench method [20].
Cytotoxicity Measurement
For each compound, 2-fold serial dilutions were prepared (in culture media), starting from the original drug stocks in DMSO (2000 µg/mL). Cell cultures were washed with media, and drug (100 µL per well) was applied at the appropriate concentrations, followed by incubation for 24 h (37°C, 5% CO2). Cells were washed with PBS, and 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) solution was applied (0.5 µg/mL in culture medium), followed by incubation for 1.5 hours (37°C, 5% CO2). MTT solution was removed, slurry was dissolved in 96% ethyl alcohol, and optical densities of solutions were determined at 535 nm on a Wallas Perkin Elmer plate reader. Based on data analysis using GraphPad Prizm 5.0 software, CC50 values were determined.
REFERENCES
Krammer, F., Smith, G.J.D., Fouchier, R.A.M., Peiris, M., Kedzierska, K., Doherty, P.C., Palese, P., Shaw, M.L., Treanor, J., Webster, R.G., and García-Sastre, A., Nat. Rev. Dis. Primers, 2018, vol. 4, article 3.
Iuliano, A.D., Roguski, K.M., Chang, H.H., Muscatello, D.J., Palekar, R., Tempia, S., Cohen, C., Gran, J.M., Schanzer, D., Cowling, B.J., Wu, P., Kyncl, J., Ang, L.W., Park, M., Redlberger-Fritz, M., Yu, H., Espenhain, L., Krishnan, A., Emukule, G., van Asten, L., Silva, S.P., Aungkulanon, S., Buchholz, U., Widdowson, M.-A., and Bresee, J.S., Lancet, 2018, vol. 391, pp. 1285–1300.
Monto, A.S. and Fukuda, K., Clin. Inf. Dis., 2020, vol. 70, pp. 951–957.
Long, J.S., Mistry, B., Haslam, S.M., and Barclay, W.S., Nat. Rev. Microbiol., 2019, vol. 17, pp. 67–81.
Gubareva, L.V., Besselaar, T.G., Daniels, R.S., Fry, A., Gregory, V., Huang, W., Hurt, A.C., Jorquera, P.A., Lackenby, A., Leang, S.K., Lo, J., Pereyaslov, D., Rebelo-de-Andrade, H., Siqueira, M.M., Takashita, E., Odagiri, T., Wang, D., Zhang, W., and Meijer, A., Antivir. Res., 2017, vol. 146, pp. 12–20.
Hauge, S.H., Dudman, S., Borgen, K., Lackenby, A., and Hungnes, O., Emerg. Inf. Dis., 2009, vol. 15, pp. 155–162.
van Dongen, M.J.P., Kadam, R.U., Juraszek, J., Lawson, E., Brandenburg, B., Schmitz, F., Schepens, W.B.G., Stoops, B., van Diepen, H.A., Jongeneelen, M., Tang, C., Vermond, J., van Eijgen-Obregoso Real, A., Blokland, S., Garg, D., Yu, W., Coutier, W., Lanckacker, E., Klap, J.M., Peeters, D.C.G., Wu, J., Buyck, C., Jonckers, T.H.M., Roymans, D., Roevens, P., Vogels, R., Koudstaal, W., Friesen, R.H.E., Raboisson, P., Dhanak, D., Goudsmit, J., and Wilson, I.A., Science, 2019, vol. 363, eaar6221.
Andronova, V.L., Skorobogatyi, M.V., Manasova, E.V., Berlin, Y.A., Korshun, V.A., and Galegov, G.A., Russ. J. Bioorg. Chem., 2003, vol. 29, pp. 262–266.
Vincent, M.R., Colpitts, C.C., Ustinov, A.V., Muqadas, M., Joyce, M.A., Barsby, N.L., Epand, R.F., Epand, R.M., Khramyshev, S.A., Valueva, O.A., Korshun, V.A., Tyrrell, D.L.J., and Schang, L.M., Proc. Natl. Acad. Sci. U. S. A., 2010, vol. 107, pp. 17339–17344.
Colpitts, C.C., Ustinov, A.V., Epand, R.F., Epand, R.M., Korshun, V.A., and Schang, L.M., J. Virol., 2013, vol. 87, pp. 3640–3654.
Speerstra, S., Chistov, A.A., Proskurin, G.V., Aralov, A.V., Ulashchik, E.A., Streshnev, P.P., Shmanai, V.V., Korshun, V.A., and Shang, L.M., Antivir. Res., 2018, vol. 149, pp. 164–173.
Orlov, A.A., Chistov, A.A., Kozlovskaya, L.I., Ustinov, A.V., Korshun, V.A., Karganova, G.G., and Osolodkin, D.I., Med. Chem. Commun., 2016, vol. 7, pp. 495–499.
Hakobyan, A., Galindo, I., Nanez, A., Arabyan, E., Karalyan, Z., Chistov, A.A., Streshnev, P.P., Korshun, V.A., Alonso, C., and Zakaryan, H., J. Gen. Virol., 2018, vol. 99, pp. 148–156.
Chistov, A.A., Orlov, A.A., Streshnev, P.P., Slesarchuk, N.A., Aparin, I.O., Rathi, B., Brylev, V.A., Kutyakov, S.V., Mikhura, I.V., Ustinov, A.V., Westman, G., Palyulin, V.A., Jain, N., Osolodkin, D.I., Kozlovskaya, L.I., and Korshun, V.A., Eur. J. Med. Chem., 2019, vol. 171, pp. 93–103.
Vigant, F., Hollmann, A., Lee, J., Santos, N.C., Jung, M.E., and Lee, B., J. Virol., 2014, vol. 88, pp. 1849–1853.
Chistov, A.A., Ivanov, N.M., Kutyakov, S.V., Ustinov, A.V., Glybin, A.V., Streshnev, P.P., Mikhura, I.V., and Korshun, V.A., Tetrahedron Lett., 2016, vol. 57, pp. 4821–4823.
Brass, E.R., Pharmacol. Rev., 2002, vol. 54, pp. 589–598.
Chistov, A.A., Kutyakov, S.V., Ustinov, A.V., Aparin, I.O., Glybin, A.V., Mikhura, I.V., and Korshun, V.A., Tetrahedron Lett., 2016, vol. 57, pp. 1003–1006.
Chistov, A.A., Kutyakov, S.V., Guz, A.V., Mikhura, I.V., Ustinov, A.V., and Korshun, V.A., Org. Prep. Proced. Int., 2017, vol. 49, pp. 377–381.
Reed, L.J. and Muench, H., Am. J. Hygiene, 1938, vol. 27, pp. 493–497.
Cohen, J., Kupferschmidt, K., Science, 2020, vol. 367, pp. 962–963.
ACKNOWLEDGMENTS
The work was supported by the Russian Science Foundation (RSF) grant no. 15-15-00053. A. A. Chistov was supported by a RF President’s Scholarship (project SP-4083.2018.4).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
COMPLIANCE WITH ETHICAL STANDARDS
This article does not contain any research involving humans or animals as research subjects.
Conflict of Interests
The authors declare that there is no conflict of interests.
NOTE ADDED IN PROOF
During production of the article (December 2019–February 2020), mankind was faced with a sudden outbreak of acute respiratory illness (with significant mortality) caused by the SARS-CoV-2 enveloped coronavirus. Currently (28.02.20), COVID-19 has been recorded in many countries and is threatening to become a pandemic [21]. The unexpected emergence of the novel virus, and its rapid spread, further highlight the urgency of developing broad-spectrum antiviral therapies targeting the lipid bilayer of enveloped viruses.
Additional information
Corresponding author: phone: +7 (499) 724-67-15; e-mail: v-korshun@yandex.ru.
Rights and permissions
About this article
Cite this article
Nikolayeva, Y.V., Ulashchik, E.A., Chekerda, E.V. et al. 5-(Perylen-3-ylethynyl)uracil Derivatives Inhibit Reproduction of Respiratory Viruses. Russ J Bioorg Chem 46, 315–320 (2020). https://doi.org/10.1134/S1068162020030139
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S1068162020030139