There are comparatively few studies on the early course and outcome of first-episode psychosis (Reference Tohen, Stoll and StrakowskiTohen et al, 1992; Reference Lieberman, Koreen and ChakosLieberman et al, 1996; Reference Gupta, Anderson and ArndtGupta et al, 1997; Reference Vázquez-Barquero, Cuesta and CastanedoVázquez-Barquero et al, 1999). The outcome of first-episode affective psychoses, and substance-related psychoses, in particular, has received scant attention. We report primary observational data on a three-year follow-up study of an inception cohort of first-episode ICD—10 (World Health Organization, 1994) psychoses treated in a modern, community-oriented mental health service. We examined the predictive validity of ICD—10 criteria by comparing outcomes of non-affective and affective psychoses. We compared three-year outcomes with two-year outcomes of an earlier similar cohort, the Nottingham subset of the Determinants of Outcome of Severe Mental Disorders (DOSMED) Study (Reference Cooper and BostockCooper & Bostock, 1988). We hypothesised better outcome of affective than non-affective psychoses in the current cohort and no differences in outcome between the current and the DOSMED cohort.
METHODOLOGY
Sample (1992-1994)
This comprised an inception cohort of all cases of first-onset psychoses (in patients aged 16-64 years) identified in Nottingham (total 16- to 64-year population, 397 048; Office of Population Censuses and Surveys (1992) data) between 1 June 1992 and 31 May 1994. Details of case ascertainment and the characteristics of the cohort have been reported previously (Reference Brewin, Cantwell and DalkinBrewin et al, 1997). The cohort was identified by screening all potential patients with psychoses making first-ever contact with psychiatric services. An over-inclusive screening schedule, which is based upon symptoms rather than diagnosis, was used (Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992). A leakage study was undertaken to ensure inclusion of cases missed by the screening process. This involved scrutinising the central patient information system, which records all new psychiatric contacts in both the hospital and the community. Patients with an organic mental illness or with severe learning disabilities were excluded.
FOLLOW-UP STUDY (1995-1997)
Tracing exercise
The follow-up assessments were conducted by S.A. and S.P.S. between 1 June 1995 and 31 May 1997 and occurred in chronological order of initial contact with psychiatric services, as close as possible to three years since initial contact. Patients currently in psychiatric care were approached through their National Health Service (NHS) consultant psychiatrist or keyworker. Patients who had left Nottingham since the original intake were traced by contacting family members, their general practitioner (GP) notes or through their NHS Central Register and Family Health Services Authorities throughout Great Britain. Patients living in Nottingham but no longer in contact with the services were sent a letter explaining the purpose of the study, following confirmation with their GP that such an approach was appropriate. If it was thought necessary, patients were approached only after the study had been explained to them first by their GP. Informed consent was sought for participation in the study and for gathering additional information from family members and carers.
Follow-up assessment
The follow-up assessment included interviews with subjects, family members and the treating psychiatric teams, and perusal of psychiatric case notes, general medical notes, community mental health team notes and GP records.
In addition the following instruments were used:
-
(a) SCAN: Schedules for Clinical Assessment in Neuropsychiatry (World Health Organization, 1992). This interview schedule measures and classifies psychopathology and behavioural disturbances associated with adult psychiatric disorders.
-
(b) DAS: Disability Assessment Schedule (Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992). This is a semi-structured assessment of functions such as self-care, social interaction, employment, etc. Items can be grouped together to derive average disability score, role handicap score and social disability score (Reference Cooper and BostockCooper & Bostock, 1988).
-
(c) SANS: Scale for Assessment of Negative Symptoms (Reference AndreasenAndreasen, 1982). This instrument measures the presence and magnitude of five negative symptoms: affective blunting, alogia, avolition/apathy, anhedonia/asociality and attentional impairment.
-
(d) BRS: Broad Rating Schedule (Reference Sartorius, Gulbinat and HarrisonSartorius et al, 1995). This incorporates Bleuler's four categories of outcome (recovered, mild, moderate, severe) of current severity of psychotic symptoms. In addition we used the Global Assessment of Functioning scales for symptoms and disability (GAF—s and GAF—d) derived from the Global Assessment Scale (Reference Endicott, Spitzer and FleissEndicott et al, 1976). The GAF rates the severity of symptoms and disability in the last month, with scores from 1 (most severe) to 90 (no symptoms). Scores of 61 and above are generally taken to represent a favourable outcome.
-
(e) Strauss-Carpenter and McGlashan Scales: (Reference Strauss and CarpenterStrauss & Carpenter, 1974; Reference McGlashanMcGlashan, 1984). These two scales measure outcomes across five domains: hospitalisation, employment, social activity, symptoms and global functioning. The latter measures longitudinal outcomes (over the total follow-up period) and the former assesses cross-sectional status (over the past year, except for clinical outcome, which is measured for the past month).
-
(f) OCCPI/OPCRIT system (Reference McGuffin, Farmer and HarveyMcGuffin et al, 1991). This check-list and computer program uses operational diagnostic criteria for psychotic disorders.
-
(g) Patient Satisfaction Rating. We used a six-item questionnaire that assessed patient satisfaction with services on a five-point scale from 1 (excellent) to 5 (terrible). This was adapted from selected items in the Verona Service Satisfaction Scale (Reference Ruggeri and Dall'AgnolaRuggeri & Dall'Agnola, 1993). For analysis, responses were dichotomised into ‘satisfied’ and ‘not satisfied’.
Mode of onset was defined as the period between the first reported symptom or noticeable behavioural change and the emergence of psychotic symptoms. The OPCRIT mode of onset categories were summarised as: onset less than one week; one week to one month; and more than one month. Ethnicity was categorised according to ethnic family origins. The main categories were White (both parents born in the UK), Indo-Asian (one or both parents born in the Indian sub-continent) and African-Caribbean (one or both parents born in the Caribbean). The rationale for recording and analysing data on ethnicity and the findings have been reported previously (Reference Harrison, Amin and SinghHarrison et al, 1999).
Reliability exercise
Both S.A. and S.P.S. carried out an inter-rater reliability exercise before the study began by concurrently rating ten subjects with psychotic illness who were not included in the sample. The OPCRIT reliability was calculated by the completion of ten case vignettes. Intra-class correlation coefficients (ICCs) were calculated for SCAN profile scores, SANS sub-scale scores, Strauss-Carpenter global rating, McGlashan global rating, GAF scores and OPCRIT subsection scores. Kappa values were calculated for the Bleuler severity rating, DAS global rating and SCAN-generated CATEGO diagnoses. Reliability was considered satisfactory if the ICC or kappa value was 0.7 or greater.
The ICC values were as follows: for SCAN profile scores, 0.67-1.0; for SANS sub-scale scores, 0.75-0.88; for McGlashan global rating, 0.92; for Strauss-Carpenter global rating, 0.86; for GAF—s, 0.97; for GAF—d, 0.98; and for OPCRIT sub-scale scores, 0.85-1.0. Kappa values were as follows: for Bleuler severity rating, 0.84; for DAS global rating, 0.88; for SCAN-generated CATEGO diagnoses, 0.75.
In some cases, the absence of any ratings led to a spuriously ‘perfect’ agreement (ICC or kappa=1.0). This occurred in the following: SCAN profile scores for Autistic Speech and Behaviour, Appetite Problems, Cognitive Impairment and Somatic and Dissociative Symptoms; and OPCRIT Substance Abuse or Dependence sub-scale (items 78-83).
Classification and description of outcomes
Both longitudinal and cross-sectional outcomes were measured in the domains of symptoms, employment, social activity, hospitalisation, compulsory detentions, course type and global functioning. Outcomes are reported for the entire cohort of first-episode psychoses and for four diagnostic groups: non-affective psychoses (all non-affective, non-substance-related psychoses: ICD—10 categories F20-29); affective psychoses (ICD—10 F30-33); schizophrenia (ICD—10 F20); and substance-related psychoses (ICD—10 F1x). We compared three characteristics of outcome with the two-year DOSMED follow-up. These were the proportion of patients in remission, the proportion currently in hospital and disability as measured by the DAS.
Comparison of outcome with prior Nottingham cohort
For comparison with the DOSMED cohort, only patients younger than 54 years, residing in the catchment area of the DOSMED study and not having a substance-induced psychosis (the inclusion criteria for the DOSMED study) were included. A total of 54/166 patients from the present cohort were thus excluded and data from 112 patients were used for direct comparison with the DOSMED cohort (n=99).
Analysis
Outcomes were compared statistically between non-affective and affective psychoses. No statistical analysis was done for patients with substance-related psychoses owing to the small numbers. Discrete/categorical outcome variables were summarised using percentages and compared using odds ratios and 95% confidence intervals. Continuous outcome measures were summarised with means and confidence intervals and compared using the t-test or one-way ANOVA.
RESULTS
The sample
Between June 1992 and May 1994, 209 patients were referred to the study. Seventy-one cases were excluded because of a previous history of psychosis or an organic aetiology. A leakage study identified another 30 patients for inclusion, giving an inception cohort of 168 cases with first-episode psychosis. One patient was found to have an organic psychosis and another refused consent to be in the study. A total of 166 patients were therefore included in the follow-up.
We traced 164 subjects (99%) to residence, obtained face-to-face interviews with 135 (81%) and another 8 (5%) were interviewed by phone. Two subjects had died, including one by suicide. Of the direct assessments, 97% were done 35-37 months after inclusion in the original cohort, thus ensuring that subjects were homogeneous with respect to time since contact with the services. We collected collateral information (from the treating psychiatry teams, the carers known to the service and GPs) on all cases, including those not interviewed. Follow-up data were therefore available for almost the entire cohort. Over the entire study, from first presentation to follow-up, 33 patients (19.9%) were never admitted to hospital, being treated entirely within the community. At the time of the followup assessment, eight subjects (4.8%) were in-patients or under the care of rehabilitation services.
Table 1 shows the socio-demographic and clinical profile of the cohort according to ICD—10 diagnostic categories at onset, made blind to outcome. A re-diagnosis exercise was conducted at three years, blind to onset diagnosis, and is reported elsewhere (Reference Amin, Singh and BrewinAmin et al, 1999). Almost two-thirds of the total sample (103/166) and over three-quarters of the group with substance-related psychoses (10/13) were less than 30 years of age. In comparison with non-affective psychoses, the group with affective psychoses had a significantly greater proportion of women and more often had an acute onset. They were also older at the time of contact and appeared to be of higher socio-economic status in that they were more likely to be employed and a house-owner, but these differences were not statistically significant. The diagnostic groups were comparable on ethnic status, except for the group with substance-related psychoses, which almost exclusively comprised White males.
Table 1 Demographic and clinical characteristics of the cohort at intake, stratified by ICD-10 diagnostic groups

| Variable | Total group (n=166) | Non-affective psychoses F20-29 (n=112) | Affective psychoses F30-33 (n=41) | Narrow schizophrenia F20 (n=56) | Substance-related psychoses F1x (n=13) |
|---|---|---|---|---|---|
| Age band (years) | |||||
| 15-30 | 103 (62.0) | 69 (61.6) | 24 (58.5) | 39 (69.6) | 10 (76.9) |
| 31-50 | 48 (28.9) | 32 (28.6) | 13 (31.7) | 13 (23.2) | 3 (23.1) |
| > 51 | 15 (9.0) | 11 (9.8) | 4 (9.8) | 4 (7.1) | 0 |
| Male | 98 (59.0) | 70 (62.5) | 16 (39.0)* | 38 (67.9) | 12 (92.3) |
| Ethnic group | |||||
| White | 121 (72.9) | 83 (74.8) | 28 (68.3) | 42 (75.0) | 12 (92.3) |
| African-Caribbean | 33 (19.9) | 23 (20.7) | 10 (24.4) | 12 (21.4) | 0 |
| Indo-Asian/other | 11 (6.6) | 5 (4.5) | 3 (7.3) | 2 (3.6) | 1 (7.7) |
| Accommodation | |||||
| Owner/rented | 106 (63.9) | 68 (62.4) | 31 (75.6) | 29 (53.7) | 7 (53.9) |
| With relative/carer | 52 (31.3) | 37 (33.9) | 10 (24.4) | 23 (42.6) | 5 (38.5) |
| Sheltered accommodation/hostel/detained | 5 (3.0) | 4 (3.7) | 0 | 2 (3.7) | 1 (7.7) |
| Employment status | |||||
| Employed/household | 42 (25.30) | 27 (24.3) | 15 (36.6) | 10 (18.9) | 0 |
| Unemployed/sickness benefit | 100 (60.24) | 71 (64.0) | 17 (41.5) | 39 (73.5) | 12 (92.3) |
| Retired/student/other | 23 (13.86) | 13 (11.7) | 9 (22.0) | 4 (7.6) | 1 (7.7) |
| Education: GCSEs | 76 (46.4) | 51 (46.4) | 18 (43.9) | 32 (58.1) | 7 (53.9) |
| Age at first contact | 30.82 (11.41) | 31.21 (11.41) | 31.41 (12.27) | 29.28 (9.73) | 25.54 (7.26) |
| Mode of onset | |||||
| < 1 week | 36 (21.7) | 21 (19.6) | 10 (25.6)** | 6 (11.5) | 5 (38.5) |
| 1 week-1 month | 24 (14.5) | 17 (15.9) | 3 (7.7) | 9 (17.3) | 4 (30.8) |
| > 1 month | 99 (59.6) | 69 (64.5) | 26 (66.7) | 37 (71.2) | 4 (30.8) |
Cross-sectional outcome
Table 2 shows the cross-sectional outcome of the total cohort, outcomes for the four diagnostic groups and comparison between non-affective psychoses (ICD—10 F20-29) and affective psychoses (ICD—10 F30-33). Numbers in parentheses in the variable column show the number of subjects for whom data were available for each outcome variable. More than half of the cohort had experienced no or minimal symptoms in the preceding month. In the preceding year, 42% had been in at least weekly social contact with friends or family, three-quarters had no hospitalisations, one-third had worked part-time or full-time and over half had no or minimal overall impairment. Schizophrenia (ICD—10 F20) had the worst outcome on almost all indices, with substance-related psychosis (ICD—10 F10-19) having an intermediate outcome between non-affective and affective psychoses.
Table 2 Cross-sectional outcomes at three years of all ICD-10 psychoses and comparison between non-affective (F20-29) and affective (F30-33) psychoses

| Outcome variable | Total group (n = 166) | Schizophrenia F20 (n = 56) | Substance-related psychoses F1x (n = 13) | Non-affective psychoses F20-29 (n = 112) | Affective psychoses F30-33 (n = 41) | Non-affective v. affective psychoses1 | P |
|---|---|---|---|---|---|---|---|
| Good outcome categories (Strauss-Carpenter, n = 148) | |||||||
| No/minimal symptoms in past month | 93 (56.0) | 22 (43.1) | 9 (69.2) | 55 (52.4) | 29 (70.7) | 2.20 (1.01, 4.76) | 0.04 |
| No hospitalisation in past year | 122 (73.5) | 40 (75.5) | 11 (84.6) | 81 (75.7) | 30 (73.2) | 1.14 (0.50, 2.59) | 0.83 |
| Weekly social contact in past year | 69 (41.6) | 11 (21.6) | 7 (53.8) | 36 (34.3) | 26 (63.4) | 3.32 (1.56, 7.05) | <0.001 |
| Employed (full- or part-time) in past year | 52 (31.3) | 8 (15.7) | 4 (30.8) | 26 (25.2) | 22 (53.7) | 3.43 (1.61, 7.32) | 0.02 |
| No/minimal impairment in past year | 90 (54.2) | 18 (34.6) | 8 (61.5) | 52 (49.1) | 30 (73.2) | 2.83 (1.29, 6.23) | 0.01 |
| GAF scores (n = 160) | |||||||
| Symptom score >61 | 98 (59.0) | 22 (42.3) | 9 (69.2) | 54 (50.9) | 35 (85.4) | 3.57 (1.55, 8.17) | <0.01 |
| Disability score > 61 | 100 (60.2) | 22 (42.3) | 8 (61.5) | 59 (55.7) | 33 (80.5) | 2.87 (1.28, 6.45) | 0.01 |
| Disability DAS scores (n = 152) | |||||||
| Average disability | 2.89 (1.38) | 3.46 (1.34) | 2.60 (1.48) | 3.08 (1.41) | 2.47 (1.16) | 0.62 (0.13, 1.10) | 0.38 |
| Role handicap | 3.19 (1.72) | 3.82 (1.61) | 2.92 (1.84) | 3.40 (1.69) | 2.60 (1.68) | 0.80 (0.19, 1.41) | 0.58 |
| Social disability | 2.37 (1.32) | 2.72 (1.06) | 2.01 (0.95) | 2.45 (1.33) | 2.17 (1.28) | 0.27 (-0.20, 0.75) | 0.54 |
| SCAN scores (n = 143) | |||||||
| Depressive symptoms | 5.17 (6.63) | 5.21 (5.70) | 6.15 (8.30) | 4.99 (6.55) | 5.33 (6.37) | 0.34 (-2.76, 2.07) | 0.78 |
| Psychotic symptoms | 3.56 (7.65) | 5.65 (9.90) | 3.38 (6.74) | 4.19 (8.32) | 1.92 (5.71) | 2.27 (-0.59, 5.13) | 0.12 |
| Total score | 25.80 (25.60) | 29.18 (29.23) | 34.31 (26.70) | 26.28 (27.35) | 21.69 (19.42) | 4.59 (-4.86, 14.04) | 0.34 |
| SANS score: global (n = 153) | 3.41 (3.65) | 5.24 (3.44) | 2.92 (3.38) | 4.18 (3.93) | 1.53 (1.94) | 2.65 (1.33, 3.97) | < 0.001 |
Figure 1 shows a comparison of non-affective psychoses and affective psychoses on the Strauss-Carpenter outcome categories. As compared to patients with non-affective psychoses, patients with affective psychoses were about three times more likely to be in weekly social contact with friends or relatives, to be employed and to have minimal impairment. The GAF and DAS score data on symptoms and disability also showed significantly better outcome for patients with affective psychoses. The two groups did not differ on the mood and psychotic symptom scores on SCAN, but non-affective psychoses had significantly higher negative symptom ratings.

Fig. 1 Cross-sectional outcome at three years of ICD—10 first-episode psychoses: comparison of (□) non-affective (F20-29) and (▪) affective (F30-33) psychoses.
Longitudinal outcome
Table 3 shows longitudinal outcome over three years for the total cohort, outcomes for the four diagnostic groups and comparison between non-affective psychoses and affective psychoses. Within the entire cohort: 60% of the patients had an episodic course with full inter-episodic remissions; around 40% had good symptomatic and social outcome; 27% had good occupational outcome; and 40% had good global functioning. As in cross-sectional outcome, schizophrenia had the worst outcome on most domains. Patients with substance-related psychosis were employed for the least proportion of time over the three-year period, despite having an episodic course with full remissions and good global functioning.
Table 3 Three-year longitudinal outcome of all ICD-10 psychoses and comparison between non-affective (F20-29) and affective (F30-33) psychoses

| Outcome variable | Total group (n = 166)1 | Schizophrenia F20 (n = 56)1 | Substance-related psychoses F1x (n = 13)1 | Non-affective psychoses F20-29 (n = 112)1 | Affective psychoses F30-33 (n = 41)1 | Non-affective v. affective psychoses2 | P |
|---|---|---|---|---|---|---|---|
| Hospitalisation (n = 153) | |||||||
| Number of in-patient days | 81.58 (128.87) | 92.59 (144.56) | 67.85 (114.78) | 87.25 (129.42) | 70.46 (133.38) | 16.79 (-30.27, 63.84) | 0.48 |
| Total number of admissions | 1.74 (1.56) | 1.61 (1.26) | 2.08 (1.89) | 1.74 (1.53) | 1.63 (1.53) | 0.11 (-0.45, 0.66) | 0.70 |
| Any compulsory detention (n = 164) | 76 (45.8) | 28 (50.9) | 6 (46.2) | 55 (50.0) | 15 (36.6) | 0.58 (0.28, 1.21) | 0.14 |
| Good longitudinal outcome | |||||||
| Episodic course, full remission (n = 149) | 97 (59.9) | 20 (37.0) | 9 (69.23) | 56 (50.00) | 32 (78.05) | 0.30 (0.13, 0.69) | < 0.01 |
| McGlashan outcome categories (n = 147) | |||||||
| Symptomatic < 25% | 63 (39.4) | 10 (19.6) | 8 (62.54) | 34 (30.36) | 21 (51.23) | 2.22 (1.06, 4.64) | 0.04 |
| Weekly social contact | 58 (37.9) | 11 (21.2) | 7 (53.8) | 34 (31.8) | 24 (58.5) | 3.03 (1.44, 6.37) | 0.003 |
| Employed > 75 follow-up period | 45 (26.8) | 7 (13.5) | 1 (7.7) | 26 (24.5) | 18 (43.9) | 2.41 (1.01, 1.71) | 0.03 |
| Global functioning 75-100% of normal | 66 (39.8) | 10 (19.2) | 9 (69.23) | 35 (31.25) | 22 (53.66) | 2.34 (1.14, 4.97) | 0.02 |
| Satisfied with services (n = 112) | 88 (53.0) | 23 (41.1) | 6 (46.2) | 55 (49.1) | 27 (65.8) | 2.45 (0.76, 7.90) | 0.20 |
Non-affective and affective psychoses did not differ significantly in the rates of compulsory detention and treatment, number of hospital admissions or the overall length of stay. Significantly more patients with non-affective than affective psychoses had a chronic, unremitting course. On the McGlashan outcome categories, patients with affective psychoses were two to three times as likely to have good symptomatic, occupational, social and global outcome as compared to those with non-affective psychoses. There was a statistically non-significant trend towards patients with affective psychoses being more satisfied with the services than patients with non-affective psychoses.
Figure 2 shows a comparison of outcome of the present cohort with the two-year outcome of the Nottingham subset of the DOSMED cohort. Similar proportions of the two cohorts were in remission at the time of follow-up but a higher proportion of the DOSMED cohort was in hospital. The three components of disability — average disability, role handicap and social disability — were rated higher in the current cohort. In the DOSMED cohort most of the DAS ratings showed mild dysfunction, whereas the current cohort had considerably more variability in the scores, with the majority indicating serious dysfunction (see Table 2). Re-analysing the data after excluding hospitalised patients from both cohorts did not alter these results.
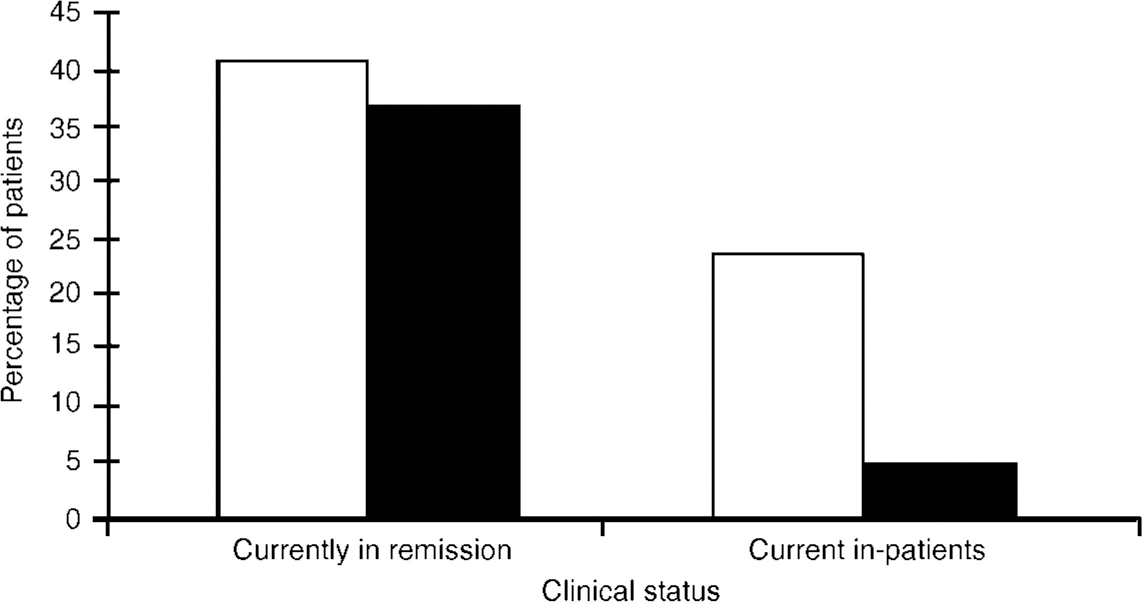
Fig. 2 Outcome of first-episode psychoses in Nottingham: comparison of (□) two-year (DOSMED cohort) and (▪) three-year (current cohort) outcomes.
DISCUSSION
Methodology
The present study has assessed three-year cross-sectional and longitudinal outcomes of an inception cohort of patients with first-onset psychoses within a geographically defined catchment area. Patients were homogeneous for time since first contact with mental health services. Multiple sources of information were used and data were collected on several established research instruments. The strengths of the study are the completeness and comprehensive tracing of the intake cohort, a high proportion of face-to-face interviews, use of international operational criteria for diagnosis and the use of standardised instruments with high interrater reliability. To the best of our knowledge, this is the first such study to use ICD—10 criteria.
Cross-sectionally about half and longitudinally between 30 and 40% of the total cohort had good outcome in all domains. These results are broadly comparable with previous outcome reports (Reference Leff, Sartorius and JablenskyLeff et al, 1992; Scottish Schizophrenia Research Group, 1992; Reference Gupta, Anderson and ArndtGupta et al, 1997; Reference Strakowski, Keck and McElroyStrakowski et al, 1998; Reference Vázquez-Barquero, Cuesta and CastanedoVázquez-Barquero et al, 1999). Our rate of 20% of patients treated entirely within the community is the same as reported earlier (Reference Castle, Phelan and WesselyCastle et al, 1994). Just over half of the patients expressed satisfaction with the effectiveness of mental health care that they had received. Only one-third of the entire cohort had been employed in any capacity in the year preceding follow-up assessment, despite symptomatic recovery and no hospital admissions, confirming the poor occupational outcome in these patients (Reference Leary, Johnstone and OwensLeary et al, 1991; Reference Mason, Harrison and GlazebrookMason et al, 1995; Reference Gupta, Anderson and ArndtGupta et al, 1997). Occupational rehabilitation has been associated with symptom reduction and improvement of insight in psychoses (Reference Bell, Lysaker and MilsteinBell et al, 1996). The poor occupational outcome in first-episode psychoses suggests that early and assertive efforts should be made at vocational rehabilitation.
Outcome of first-episode affective psychoses
Earlier outcome studies have suggested that affective disorders have a poor symptomatic, social and occupational outcome even relatively early in the course of the illness (Reference Coryell, Scheftner and KellerCoryell et al, 1993; Reference Gitlin, Swendsen and HellerGitlin et al, 1995; Reference Goldberg, Harrow and GrossmanGoldberg et al, 1995). Most of these studies are based on in-patient samples rather than first-episode affective psychoses. In a one-year follow-up study of patients with first-hospitalisation affective psychoses, Strakowski et al (Reference Strakowski, Keck and McElroy1998) reported symptomatic recovery (as defined by an eight-week period of minimal psychiatric symptoms) in 35% of patients and functional recovery (eight weeks of functioning at premorbid level) in 35% patients. Our corresponding figures of good outcome (as defined by minimal symptoms and minimal impairment) are much higher: 70% and 73%, respectively. Strakowski et al had a follow-up loss of 23% of the original cohort. The better outcome of affective psychoses in the present study may therefore be due to low attrition of good outcome cases, thus avoiding a selection bias towards a poorer outcome group.
Predictive validity of ICD—10 diagnostic criteria: comparison of outcomes between affective and non-affective psychoses
Both cross-sectional and longitudinal outcomes were significantly better for affective psychoses than for non-affective psychoses, confirming previous reports (Reference Leff, Sartorius and JablenskyLeff et al, 1992; Reference Harrow, Sands and SilversteinHarrow et al, 1997). Affective and non-affective psychoses did not differ on indices of hospitalisation, despite a more benign and remitting course in the former. A possible explanation for this might be that the ‘style of working’ of psychiatrists and other professionals influences this outcome measure more than any illness characteristic. Our finding that affective psychoses (F30-33) had a better outcome than non-affective psychoses (F20-29), with schizophrenia (F20) having the poorest outcome, provides confirmation that ICD—10 criteria for the diagnostic stratification of non-organic psychoses have good predictive validity.
Outcome of first-episode substance-related psychoses
The prevalence and pattern of substance misuse in this cohort have been reported previously (Reference Cantwell, Brewin and GlazebrookCantwell et al, 1999). The diagnosis of substance-related psychosis was stable in the majority of the cases, and over a period of three years 9/13 subjects retained their original diagnosis. The positive predictive value of the diagnosis was 69% (Reference Amin, Singh and BrewinAmin et al, 1999). On most domains, these patients had an outcome intermediate between those for schizophrenia and affective psychoses. However, despite an episodic course, benign symptomatic outcome and good overall functioning, they had the worst occupational outcome of the entire cohort. The cultural lifestyle of drug misuse may militate against work rehabilitation, although other factors, such as stigma of drug abuse or employers' concerns about health and safety issues, may also contribute to such poor occupational outcome.
Outcome of first-episode psychoses: comparison with DOSMED cohort
Despite a similar three-year clinical outcome to the DOSMED two-year outcome, the present cohort was rated as having higher levels of disability. Raters in the present study were blind to this comparison, hence there was no systematic bias towards a higher disability rating in the present cohort. However, there were methodological differences in data collection between the two studies, in addition to the different follow-up period. In the DOSMED two-year follow-up, raters collected data on DAS alone, and the key carer was the key informant. In the present study, raters completed the DAS using all sources of information, including patient interview. This raises the possibility that a prior comprehensive assessment of clinical, social and interpersonal functioning might provide a global view of disability and therefore a higher DAS rating. Patients and their carers may also differ in how they perceive the type and magnitude of the patient's disability.
These methodological differences may entirely explain the different disability ratings between the cohorts. However, we are left with the possibility that there was a true difference in the magnitude of disability between these two cohorts collected over a decade apart. This would be an important finding, although difficult to confirm, with major implications for service provision.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ In a modern community-orientated mental health service, between 30 and 60% of all patients with first-episode psychosis experience a good outcome at three years.
-
▪ The ICD—10 criteria for the diagnostic stratification of psychotic disorders have good predictive validity.
-
▪ In cohorts collected over a decade apart, the proportion of patients with first-episode psychosis in remission at two to three years appears not to have changed.
LIMITATIONS
-
▪ Outcome measures may not detect subtle differences between patients, and within diagnostic categories, which contribute to the varied outcomes of first-episode psychoses.
-
▪ Comparison of level of disability in the current cohort with the DOSMED cohort is tentative because of methodological differences in data collection.
-
▪ The findings apply to treated outcomes in an established community service and may have limited generalisability.
ACKNOWLEDGEMENT
Professor John Cooper gave invaluable advice on the DOSMED comparison.










eLetters
No eLetters have been published for this article.