Abstract
Background
In the current cancer staging systems, the location of lymph node (LN) metastases is not considered, although LN status is defined according to the number of LN metastases.
Objectives
This study aimed to investigate the clinical impact of the location of LN metastases in esophageal cancer and to evaluate the relevance of minimizing the extent of lymphadenectomy after neoadjuvant therapy.
Methods
In 561 patients with esophageal cancer who underwent neoadjuvant chemotherapy, the therapeutic value of each LN dissection was estimated by multiplying the incidence of metastasis by the 5-year survival rate of patients with positive nodes. In addition, we examined whether the value was affected by the response to neoadjuvant therapy.
Results
Metastasis to the celiac LN and middle mediastinal LN regions was identified as an independent prognostic factor by multivariate analysis, together with the number of LN metastases; however metastasis to the cervical LN and upper mediastinal LN regions was not identified as an independent prognostic factor. The therapeutic value was high in recurrent nerve LNs, paraesophageal LNs, paracardial LNs, and left gastric LNs. The therapeutic value for each LN dissection did not change according to the response to neoadjuvant therapy, excluding the lower mediastinal LN and perigastric LN stations for which the value was relatively high in patients with a poor response.
Conclusion
The present study shows that the location and number of LN metastases have a prognostic impact in patients with esophageal cancer undergoing neoadjuvant chemotherapy. Limited lymphadenectomy according to the response to neoadjuvant therapy cannot be justified.


Similar content being viewed by others
References
Tepper J, Krasna MJ, Niedzwiecki D, et al. Phase III trial of trimodality therapy with cisplatin, fluorouracil, radiotherapy, and surgery compared with surgery alone for esophageal cancer: CALGB 9781. J Clin Oncol 2008; 26: 1086–1092.
Gebski V, Burmeister B, Smithers BM, et al. Survival benefits from neoadjuvant chemoradiotherapy or chemotherapy in oesophageal carcinoma: a meta-analysis. Lancet Oncol. 2007; 8: 226–234.
van Hagen P, Hulshof MC, van Lanschot JJ, et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med. 2012;366:2074–2084.
Medical Research Council Oesophageal Cancer Working Group. Surgical resection with or without preoperative chemotherapy in oesophageal cancer: a randomised controlled trial. Lancet 2002;359:1727–1733.
Cunningham D, Allum WH, Stenning SP, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355:11–20.
Brierley J, Gospodarowicz M, Wittekind C. TNM Classification of Malignant Tumours. Eighth edition. Oxford: Wiley: 2017.
Amin MB, Edge SB, Greene FL, et al. AJCC Cancer Staging Manual. Eighth edition. New York: Springer; 2017.
Koen Talsma A, Shapiro J, Looman CW, et al. Lymph node retrieval during esophagectomy with and without neoadjuvant chemoradiotherapy: prognostic and therapeutic impact on survival. Ann Surg. 2014;260:786–792.
Robb WB, Dahan L, Mornex F, et al. Impact of neoadjuvant chemoradiation on lymph node status in esophageal cancer: post hoc analysis of a randomized controlled trial. Ann Surg. 2015;261:902–908.
Castoro C, Scarpa M, Cagol M, et al. Nodal metastasis from locally advanced esophageal cancer: how neoadjuvant therapy modifies their frequency and distribution. Ann Surg Oncol. 2011;18:3743–3754.
Shridhar R, Hoffe SE, Almhanna K, et al. Lymph node harvest in esophageal cancer after neoadjuvant chemoradiotherapy. Ann Surg Oncol. 2013;20:3038–3043.
Vallböhmer D, Hölscher AH, DeMeester S, et al. A multicenter study of survival after neoadjuvant radiotherapy/chemotherapy and esophagectomy for ypT0N0M0R0 esophageal cancer. Ann Surg. 2010;252:744–749.
Mariette C, Piessen G, Briez N, et al. The number of metastatic lymph nodes and the ratio between metastatic and examined lymph nodes are independent prognostic factors in esophageal cancer regardless of neoadjuvant chemoradiation or lymphadenectomy extent. Ann Surg. 2008; 247:365–371.
Solomon N, Zhuge Y, Cheung M, et al. The roles of neoadjuvant radiotherapy and lymphadenectomy in the treatment of esophageal adenocarcinoma. Ann Surg Oncol. 2010;17:791–803.
Torgersen Z, Sundaram A, Hoshino M, et al. Prognostic implications of lymphadenectomy in esophageal cancer after neo-adjuvant therapy: a single center experience. J Gastrointest Surg. 2011;15:1769–1776.
Visser E, Markar SR, Ruurda JP, et al. Prognostic Value of Lymph Node Yield on Overall Survival in Esophageal Cancer Patients: A Systematic Review and Meta-analysis. Ann Surg. Epub 23 May 2018. https://doi.org/10.1097/sla.0000000000002824.
Miyata H, Yamasaki M, Takahashi T, et al. Relevance of 18F-fluorodeoxyglucose positron emission tomography-positive lymph nodes after neoadjuvant chemotherapy for squamous cell oesophageal cancer. Br J Surg 2013;100:1490–1497.
Yamasaki M, Yasuda T, Yano M, et al. Multicenter randomized phase II study of cisplatin and fluorouracil plus docetaxel (DCF) compared with cisplatin and fluorouracil plus Adriamycin (ACF) as preoperative chemotherapy for resectable esophageal squamous cell carcinoma (OGSG1003). Ann Oncol. 2017;28:116–120.
Miyata H, Yano M, Doki Y, et al. A prospective trial for avoiding cervical lymph node dissection for thoracic esophageal cancers, based on intra-operative genetic diagnosis of micrometastasis in recurrent laryngeal nerve chain nodes. J Surg Oncol. 2006; 93: 477–484.
The Japan Esophageal Society (ed). Japanese Classification of Esophageal Cancer. Tokyo: Kanehara Shuppan; 2015.
SasakoM, McCulloch P, Kinoshita T, et al. New method to evaluate the therapeutic value of lymph node dissection for gastric cancer. Br J Surg. 1995;82:346–351.
Udagawa H, Ueno M, Shinohara H, et al. The importance of grouping of lymph node stations and rationale of three-field lymphoadenectomy for thoracic esophageal cancer. J Surg Oncol. 2012;106:742–747.
Miyata H, Yamasaki M, Makino T, et al. Therapeutic value of lymph node dissection for esophageal squamous cell carcinoma after neoadjuvant chemotherapy. J Surg Oncol. 2015;112:60–65.
Tachimori Y, Ozawa S, Numasaki H, et al. Efficacy of lymph node dissection by node zones according to tumor location for esophageal squamous cell carcinoma. Esophagus. 2016;13:1–7.
Fujitani K, Miyashiro I, Mikata S, et al. Pattern of abdominal nodal spread and optimal abdominal lymphadenectomy for advanced Siewert type II adenocarcinoma of the cardia: results of a multicenter study. Gastric Cancer. 2013;16:301–308.
Miyata H, Yamasaki M, Miyazaki Y, et al. Clinical importance of supraclavicular lymph node metastasis after neoadjuvant chemotherapy for esophageal squamous cell carcinoma. Ann Surg. 2015;262:280–285.
Sepesi B, Schmidt HE, Lada M, et al. Survival in patients with esophageal adenocarcinoma undergoing trimodality therapy is independent of regional lymph node location. Ann Thorac Surg. 2016;101:1075–1080.
Talsma AK, Ong CA, Liu X, et al. Location of lymph node involvement in patients with esophageal adenocarcinoma predicts survival. World J Surg. 2014;38:106–113.
Anderegg MC, Lagarde SM, Jagadesham VP, et al. Prognostic significance of the location of lymph node metastases in patients with adenocarcinoma of the distal esophagus or gastroesophageal junction. Ann Surg. 2016;264:847–853.
Rice TW, Ishwaran H, Kelsen DP, et al. Recommendations for neoadjuvant pathologic staging (ypTNM) of cancer of the esophagus and esophagogastric junction for the 8th edition AJCC/UICC staging manuals. Dis Esophagus. 2016;29:906–912.
Phillips AW, Lagarde SM, Navidi M, et al. Impact of extent of lymphadenectomy on survival, post neoadjuvant chemotherapy and transthoracic esophagectomy. Ann Surg. 2017;265:750–756.
Noordman BJ, Klaveren D, Henegouwen MB, et al. Impact of surgical approach on long-term survival in esophageal adenocarcinoma patients with or without neoadjuvant chemoradiotherapy. Ann Surg. 2018;267(5):892–897.
Visser E, van Rossum PSN, Ruurda JP, et al. Impact of lymph node yield on overall survival in patients treated with neoadjuvant chemoradiotherapy followed by esophagectomy for cancer: a population-based cohort study in the Netherlands. Ann Surg. 2017;266:863–869.
Nakamura K, Kato K, Igaki H, et al. Three-arm phase III trial comparing cisplatin plus 5-FU (CF) versus docetaxel, cisplatin plus 5-FU (DCF) versus radiotherapy with CF (CF-RT) as preoperative therapy for locally advanced esophageal cancer (JCOG1109, NExT study). Jpn J Clin Oncol. 2013;43:752–755.
Hagens ERC, van Berge Henegouwen MI, Cuesta MA, et al. The extent of lymphadenectomy in esophageal resection for cancer should be standardized. J Thorac Dis. 2017;9 Suppl 8:S713–S723.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
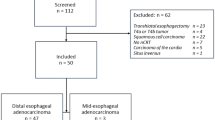
Fig. 1
Map of each lymph node, defined by the Japanese classification and AJCC cancer staging systems. Each letter represents a lymph node listed in Table 1. Upper: Japanese classification; lower: AJCC cancer staging (TIFF 2980 kb)
Fig. 2
Overall survival rate in 561 patients with esophageal cancer who underwent neoadjuvant chemotherapy followed by surgery, according to the number of metastatic lymph nodes (TIFF 2310 kb)
Fig. 3
Overall survival rate in 561 patients according to the response to neoadjuvant chemotherapy (TIFF 2398 kb)
Appendices
Surgical Treatment
Surgical resection was performed 3–6 weeks after the completion of chemotherapy. Standard procedures for middle and lower thoracic esophageal cancer in this series consisted of transthoracic esophagectomy with cervical lymphadenectomy, mediastinal lymphadenectomy, upper abdominal lymphadenectomy, reconstruction of the gastric tube, and anastomosis of the cervical incision. Cervical lymphadenectomy was sometimes omitted based on pretreatment diagnosis of LN metastases and the intraoperative genetic and pathological diagnosis of LN metastasis along the recurrent laryngeal nerves.19 Pretracheal LNs and LNs around the abdominal aorta were dissected only when those LNs seemed to be metastatic at the initial diagnosis.
Statistical Analysis
Data are expressed as the mean ± standard deviation. Overall survival was calculated from the date of commencement of neoadjuvant therapy to the occurrence of the event or the last known date of follow-up. Actual survival was calculated using the Kaplan–Meier method, and statistically evaluated using the log-rank test. The Cox proportional hazards regression model was used to analyze the simultaneous influence of various prognostic factors. A p value < 0.05 denoted the presence of statistical significance. These analyses were carried out using JMP version 9.0 software (SAS institute, Cary, NC, USA).
Rights and permissions
About this article
Cite this article
Miyata, H., Sugimura, K., Yamasaki, M. et al. Clinical Impact of the Location of Lymph Node Metastases After Neoadjuvant Chemotherapy for Middle and Lower Thoracic Esophageal Cancer. Ann Surg Oncol 26, 200–208 (2019). https://doi.org/10.1245/s10434-018-6946-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-018-6946-z