Abstract
Introduction
Quality of surgical resection metrics (QSRMs) have been used as surrogates for long-term oncologic outcomes in non-inferiority randomized clinical trials (RCTs) comparing laparoscopic and open surgery for rectal cancer. However, non-inferiority margins (ΔNI) for QSRMs have not been previously defined.
Methods
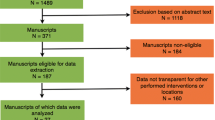
A two-round, web-based Delphi was used to define ΔNI for four QSRMs: positive circumferential resection margin (CRM), incomplete plane of mesorectal excision (PME), positive distal resection margin (DRM), and a composite of these outcomes. Overall, 130 international experts in rectal cancer (68 surgeons, 20 medical oncologists, 16 radiation oncologists, and 26 pathologists) were invited to participate. Experts were presented with evidence syntheses summarizing the association between QSRMs and long-term outcomes, and pooled quality of surgical resection outcomes for open surgery, and were asked to provide ΔNI for all outcomes balancing the risks and benefits of minimally invasive surgery.
Results
Seventy-two experts participated: 57 completed the initial questionnaire and 58 completed the revised questionnaire, with 43 participating in both rounds. Consensus was reached for all individual QSRM ΔNI but not for the composite. The mean (standard deviation) ΔNI was an absolute difference of 2.33% (1.59%) for the proportion of positive CRMs when comparing surgical interventions for the treatment of rectal cancer: 2.85% (1.83%) for incomplete PME; 1.28% (1.13%) for positive DRMs; and 2.71% (2.28%) for the composite. However, opinions varied widely for the composite outcome.
Conclusions
Web-based Delphi processes are a feasible approach to generate ΔNI to evaluate novel surgical interventions. The generated ΔNI for QSRMs for rectal cancer can be used for future RCTs and non-inferiority meta-analyses.



Similar content being viewed by others
References
Schwenk W, Haase O, Neudecker J, Muller JM. Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev. 2005;3:CD003145.
Mulla SM, Scott IA, Jackevicius CA, You JJ, Guyatt GH. How to use a noninferiority trial: users’ guides to the medical literature. JAMA. 2012;308(24):2605–11.
Baber N. International conference on harmonisation of technical requirements for registration of pharmaceuticals for human use (ICH). Br J Clin Pharmacol. 1994;37(5):401–4.
Committee for Medicinal Products for Human Use (CHMP) guideline on the choice of the non-inferiority margin. Stat Med. 2006;25(10):1628.
Rothmann M, Li N, Chen G, Chi GY, Temple R, Tsou HH. Design and analysis of non-inferiority mortality trials in oncology. Stat Med. 2003;22(2):239–64.
Rothmann MD, Tsou HH. On non-inferiority analysis based on delta-method confidence intervals. J Biopharm Stat. 2003;13(3):565–83.
Wyrwich KW, Spertus JA, Kroenke K, et al. Clinically important differences in health status for patients with heart disease: an expert consensus panel report. Am Heart J. 2004;147(4):615–22.
Bellamy N, Carette S, Ford P, et al. Osteoarthritis antirheumatic drug trials. III. Setting the delta for clinical trials—results of a consensus development (Delphi) exercise. J Rheumatol. 1992;19(3):451–7.
McGlothlin AE, Lewis RJ. Minimal clinically important difference: defining what really matters to patients. JAMA. 2014;312(13):1342–3.
Wells G, Beaton D, Shea B, et al. Minimal clinically important differences: review of methods. J Rheumatol. 2001;28(2):406–12.
Treadwell JR, Uhl S, Tipton K, et al. Assessing equivalence and noninferiority. J Clin Epidemiol. 2012;65(11):1144–9.
Stevenson AR, Solomon MJ, Lumley JW, et al. Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA. 2015;314(13):1356–63.
Fleshman J, Branda M, Sargent DJ, et al. Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA. 2015;314(13):1346–55.
Kennedy RH, Francis EA, Wharton R, et al. Multicenter randomized controlled trial of conventional versus laparoscopic surgery for colorectal cancer within an enhanced recovery programme: EnROL. J Clin Oncol. 2014;32(17):1804–11.
van der Pas MH, Haglind E, Cuesta MA, et al. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol. 2013;14(3):210–8.
Gong J, Shi D-B, Li X-X, Cai S-J, Guan Z-Q, Xu Y. Short-term outcomes of laparoscopic total mesorectal excision compared to open surgery. World J Gastroenterol. 2012;18(48):7308.
Liang XB, Hou SH, Li GD, et al. Randomized controlled trial of rectal laparoscopic surgery compared to open surgery 3-year efficacy summary. European Surgery—Acta Chirurgica Austriaca. 2015. In: Conference: 8th annual meeting of the chinese college of surgeons and 19th annual meeting of the European Society of Surgery. Beijing. Conference Publication: (var.pagings), vol. 47, p. S79.
Kang SB, Park JW, Jeong SY, et al. Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol. 2010;11(7):637–45.
Lujan J, Valero G, Hernandez Q, Sanchez A, Frutos M, Parrilla P. Randomized clinical trial comparing laparoscopic and open surgery in patients with rectal cancer. Br J Surg. 2009;96(9):982–9.
Pechlivanides G, Gouvas N, Tsiaoussis J, et al. Lymph node clearance after total mesorectal excision for rectal cancer: laparoscopic versus open approach. Dig Dis. 2007;25(1):94–9.
Braga M, Frasson M, Vignali A, Zuliani W, Capretti G, Di Carlo V. Laparoscopic resection in rectal cancer patients: outcome and cost-benefit analysis. Dis Colon Rectum. 2007;50(4):464–471.
Guillou PJ, Quirke P, Thorpe H, et al. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365(9472):1718–26.
Ng SS, Leung KL, Lee JF, et al. Laparoscopic-assisted versus open abdominoperineal resection for low rectal cancer: a prospective randomized trial. Ann Surg Oncol. 2008;15(9):2418–25.
Ng SS, Leung KL, Lee JF, Yiu RY, Li JC, Hon SS. Long-term morbidity and oncologic outcomes of laparoscopic-assisted anterior resection for upper rectal cancer: ten-year results of a prospective, randomized trial. Dis Colon Rectum. 2009;52(4):558–66.
Ng SS, Lee JF, Yiu RY, et al. Laparoscopic-assisted versus open total mesorectal excision with anal sphincter preservation for mid and low rectal cancer: a prospective, randomized trial. Surg Endosc. 2014;28(1):297–306.
Zhou X, Liu F, Lin C, et al. Hand-assisted laparoscopic surgery compared with open resection for mid and low rectal cancer: a case-matched study with long-term follow-up. World J Surg Oncol. 13(1) (no pagination), 2015. 2015;Article Number:199. Date of Publication: June 110.
Araujo SEA, Sousa Jr AHdS, Campos FGCMd, et al. Conventional approach × laparoscopic abdominoperineal resection for rectal cancer treatment after neoadjuvant chemoradiation: results of a prospective randomized trial. Revista do Hospital das Clínicas. 2003;58(3):133–40.
Hsu C-C, Sandford BA. The Delphi technique: making sense of consensus. Pract Assess Res Eval. 2007;12(10):1–8.
Lee AC, Cousens S, Darmstadt GL, et al. Care during labor and birth for the prevention of intrapartum-related neonatal deaths: a systematic review and Delphi estimation of mortality effect. BMC Public Health. 2011;11(Suppl 3):S10.
Roxburgh CS, Guillem JG. Outcomes of open vs laparoscopic rectal cancer resection. JAMA Oncol. 2017;3(1):115–6.
Rehal S, Morris TP, Fielding K, Carpenter JR, Phillips PPJ. Non-inferiority trials: are they inferior? A systematic review of reporting in major medical journals. BMJ Open. 2016;6(10):e012594.
Gayet-Ageron A, Agoritsas T, Rudaz S, Courvoisier D, Perneger T. The choice of the noninferiority margin in clinical trials was driven by baseline risk, type of primary outcome, and benefits of new treatment. J Clin Epidemiol. 2015;68(10):1144–51.
Funding
This study was funded by a Canadian Institutes of Health Research (CIHR) Operating Grant (Funding Reference No. 115164) and CIHR Foundation Grant (Funding Reference No. 148470). The funding sources had no role in the design or conduct of the study; collection, management, analysis or interpretation of the data; or preparation, review or approval of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Sergio A. Acuna, Tyler R. Chesney, Sonali T. Amarasekera, and Nancy N. Baxter have no conflicts of interest to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Acuna, S.A., Chesney, T.R., Amarasekera, S.T. et al. Defining Non-inferiority Margins for Quality of Surgical Resection for Rectal Cancer: A Delphi Consensus Study. Ann Surg Oncol 25, 3171–3178 (2018). https://doi.org/10.1245/s10434-018-6639-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-018-6639-7