Abstract
Introduction
The symptom profile in cancer patients and the association between palliative care (PC) and symptoms has not been studied in the general population. We addressed these gaps in gastrointestinal (GI) cancer patients in the final year of life.
Methods
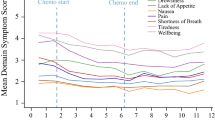
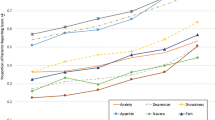
Patients dying of esophageal, gastric, colon, and anorectal cancers during 2003–2015 were identified. Symptom scores were recorded in the year before death using the Edmonton Symptom Assessment System (ESAS), which includes scores from 0 to 10 in nine domains. Symptom severity was categorized as none–mild (≤ 3) or moderate–severe (≥ 4–10). Adjusted associations between outpatient PC and moderate–severe ESAS scores were determined, and the effect of PC initiation on ESAS scores was estimated.
Results
The cohort included 11,242 patients who died (esophageal [17%], gastric [20%], colon [38%], and anorectal [26%] cancers). Fifty percent experienced moderate–severe scores in tiredness, lack of well-being, and lack of appetite earlier (weeks 18 to 12 before death), whereas 50% experienced moderate–severe scores in drowsiness, pain, and shortness of breath later (weeks 5 to 2 before death) in the disease course. Outpatient PC was associated with an increased likelihood of moderate–severe scores in all domains, with the highest score in pain (odds ratio [OR] 1.86, 95% confidence interval [CI] 1.68–2.05). In PC-naïve patients with moderate–severe scores, initiation of outpatient PC was associated with a 1- to 3-point decrease in subsequent scores, with the greatest reductions in pain (OR − 1.91, 95% CI − 2.11 to − 1.70) and nausea (OR − 3.01, 95% CI − 3.31 to − 2.71).
Conclusion
GI cancer patients experience high symptom burden in the final year of life. Outpatient PC initiation is associated with a decrease in symptoms.



Similar content being viewed by others
References
Seow H, Barbera L, Sutradhar R, Howell D, Dudgeon D, Atzema C, et al. Trajectory of performance status and symptom scores for patients with cancer during the last 6 months of life. J Clin Oncol. 2011;29(9):1151–8.
Barbera L, Seow H, Howell D, Sutradhar R, Earle C, Liu Y, et al. Symptom burden and performance status in a population-based cohort of ambulatory cancer patients. Cancer. 2010;116(24):5767–76.
Bubis LD, Davis L, Mahar A, Barbera L, Li Q, Moody L, et al. Symptom burden in the first year after cancer diagnosis: an analysis of patient-reported outcomes. J Clin Oncol. 2018;36(11):1103–11.
Wen FH, Chen JS, Chou WC, Hsieh CH, Chang WC, Shen WC, et al. Quality of life and psychological distress are differentially associated with distinct symptom-functional states in terminally ill cancer patients’ last year of life. Psychooncology. 2018;27(9):2111–8.
Wilson KG, Chochinov HM, Skirko MG, Allard P, Chary S, Gagnon PR, et al. Depression and anxiety disorders in palliative cancer care. J Pain Symptom Manag. 2007;33(2):118–29.
Brooks GA, Abrams TA, Meyerhardt JA, Enzinger PC, Sommer K, Dalby CK, et al. Identification of potentially avoidable hospitalizations in patients with GI cancer. J Clin Oncol. 2014;32(6):496–503.
Barbera L, Atzema C, Sutradhar R, Seow H, Howell D, Husain A, et al. Do patient-reported symptoms predict emergency department visits in cancer patients? A population-based analysis. Ann. Emerg Med. 2013;61(4):427–37.
Hui D, Bruera E. The edmonton symptom assessment system 25 years later: past, present, and future developments. J Pain Symptom Manag. 2017;53(3):630–43.
Bruera E, Kuehn N, Miller MJ, Selmser P, Macmillan K. The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care. 1991;7(2):6–9.
Chang VT, Hwang SS, Feuerman M. Validation of the edmonton symptom assessment scale. Cancer. 2000;88(9):2164–71.
Pereira J, Green E, Molloy S, Dudgeon D, Howell D, Krzyzanowska MK, et al. Population-based standardized symptom screening: cancer care Ontario’s edmonton symptom assessment system and performance status initiatives. J Oncol Pract. 2014;10(3):212–4.
Seow H, Sussman J, Martelli-Reid L, Pond G, Bainbridge D. Do high symptom scores trigger clinical actions? An audit after implementing electronic symptom screening. J Oncol Pract. 2012;8(6):e142–8.
Okafor PN, Stobaugh DJ, Nnadi AK, Talwalkar JA. Determinants of palliative care utilization among patients hospitalized with metastatic gastrointestinal malignancies. Am J Hosp Palliat Care. 2017;34(3):269–274.
Merchant SJ, Lajkosz K, Brogly SB, Booth CM, Nanji S, Patel SV, et al. The final 30 days of life: a study of patients with gastrointestinal cancer in Ontario, Canada. J Palliat Care. 2017;32(3–4)92–100.
Merchant SJ, Brogly SB, Goldie C, Booth CM, Nanji S, Patel SV, et al. Palliative care is associated with reduced aggressive end-of-life care in patients with gastrointestinal cancer. Ann Surg Oncol. 2018;25(6):1478–87.
Clarke EA, Marrett LD, Kreiger N. Cancer registration in Ontario: a computer approach. IARC Sci Publ. 1991;(95):246–57.
Li KK, Harris K, Hadi S, Chow E. What should be the optimal cut points for mild, moderate, and severe pain? J Palliat Med. 2007;10(6):1338–46.
Selby D, Cascella A, Gardiner K, Do R, Moravan V, Myers J, et al. A single set of numerical cutpoints to define moderate and severe symptoms for the edmonton symptom assessment system. J Pain Symptom Manag. 2010;39(2):241–9.
Hui D, Kilgore K, Fellman B, Urbauer D, Hall S, Fajardo J, et al. Development and cross-validation of the in-hospital mortality prediction in advanced cancer patients score: a preliminary study. J Palliat Med. 2012;15(8):902–9.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–9.
McMaster University. Ontario Marginalization Index 2012 [cited 1 Nov 2016]. https://crunch.mcmaster.ca/documents/ON-Marg_user_guide_1.0_FINAL_MAY2012.pdf.
Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162(3):199–200.
Wang M. Generalized estimating equations in longitudinal data analysis: a review and recent developments. Adv Stat. 2014;2014:303728. https://doi.org/10.1155/2014/303728.
Spoozak L, Seow H, Liu Y, Wright J, Barbera L. Performance status and symptom scores of women with gynecologic cancer at the end of life. Int J Gynecol Cancer. 2013;23(5):971–8.
Wong AKY. Referral patterns to palliative care: an inpatient snapshot study. J Clin Oncol. 2016;34(26 Suppl):119.
Morita T, Akechi T, Ikenaga M, Kizawa Y, Kohara H, Mukaiyama T, et al. Late referrals to specialized palliative care service in Japan. J Clin Oncol. 2005;23(12):2637–44.
Cherny N, Catane R, Schrijvers D, Kloke M, Strasser F. European society for medical oncology (ESMO) program for the integration of oncology and palliative care: a 5-year review of the designated centers’ incentive program. Ann Oncol. 2010;21(2):362–9.
Ferrell BR, Temel JS, Temin S, Alesi ER, Balboni TA, Basch EM, et al. Integration of palliative care into standard oncology care: American society of clinical oncology clinical practice guideline update. J Clin Oncol. 2017;35(1):96–112.
Barbera L, Seow H, Husain A, Howell D, Atzema C, Sutradhar R, et al. Opioid prescription after pain assessment: a population-based cohort of elderly patients with cancer. J Clin Oncol. 2012;30(10):1095–9.
Hui D, Shamieh O, Paiva CE, Perez-Cruz PE, Kwon JH, Muckaden MA, et al. Minimal clinically important differences in the edmonton symptom assessment scale in cancer patients: a prospective, multicenter study. Cancer. 2015;121(17):3027–35.
Hui D, Park M, Shamieh O, Paiva CE, Perez-Cruz PE, Muckaden MA, et al. Personalized symptom goals and response in patients with advanced cancer. Cancer. 2016;122(11):1774–81.
Shamieh O, Khamash O, Khraisat M, Jbouri O, Awni M, Al-Hawamdeh A, et al. Impact of outpatient palliative care (PC) on symptom burden in patients with advanced cancer at a tertiary cancer center in Jordan. Support Care Cancer. 2017;25(1):177–83.
Kang JH, Kwon JH, Hui D, Yennurajalingam S, Bruera E. Changes in symptom intensity among cancer patients receiving outpatient palliative care. J Pain Symptom Manag. 2013;46(5):652–60.
Nicholls SG, Langan SM, Benchimol EI. Routinely collected data: the importance of high-quality diagnostic coding to research. CMAJ Can Med Assoc. 2017;189(33):E1054–E5.
Acknowledgement
This study was funded by a Faculty of Health Sciences Research Initiation Grant (SM), the Department of Surgery at Queen’s University, and the Women’s Giving Circle, and was supported by the ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by the ICES or the Ontario MOHLTC is intended or should be inferred. Parts of this material are based on data and information compiled and provided by the CIHI. However, the analyses, conclusions, opinions, and statements expressed herein are those of the authors, and not necessarily those of the CIHI.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to study conception and design, or analysis and interpretation of data; contributed to drafting the article or revising it critically for important intellectual content; provided final approval of the version to be published; and agreed to be accountable for all aspects of this work.
Corresponding author
Ethics declarations
Disclosures
Shaila J. Merchant, Susan B. Brogly, Christopher M. Booth, Craig Goldie, Sulaiman Nanji, Sunil V. Patel, Katherine Lajkosz, and Nancy N. Baxter have no disclosures to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10434_2019_7320_MOESM1_ESM.docx
Fig. 1 Proportion of the cohort with moderate–severe (≥ 4–10) symptom scores at any time in the final year of life, by week and domain (DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Merchant, S.J., Brogly, S.B., Booth, C.M. et al. Palliative Care and Symptom Burden in the Last Year of Life: A Population-Based Study of Patients with Gastrointestinal Cancer. Ann Surg Oncol 26, 2336–2345 (2019). https://doi.org/10.1245/s10434-019-07320-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07320-z