Published online Mar 26, 2023. doi: 10.12998/wjcc.v11.i9.2015
Peer-review started: November 15, 2022
First decision: December 26, 2022
Revised: January 5, 2023
Accepted: February 21, 2023
Article in press: February 21, 2023
Published online: March 26, 2023
Postherpetic neuralgia (PHN) is a typical neuropathic pain condition that appears in the lesioned skin regions following the healing of shingles. The pain condition tends to persist, which is often accompanied by negative emotions (e.g., anxiety and depression) and substantially reduces the quality of life. In addition to analgesia (e.g., pregabalin and gabapentin), nerve radiofrequency technology is an effective treatment for intractable PHN. However, there is still a significant portion of patients who do not benefit from this treatment. As a non-invasive form of brain stimulation, repetitive transcranial magnetic stimulation (rTMS) targeting the motor cortex is able to reduce neuropathic pain with grade A evidence.
Here we report two cases in which motor cortex rTMS was used to treat intractable PHN that did not respond to initial drug and radiofrequency therapies. Moreover, we specifically investigated rTMS efficacy at 3 mo following treatment.
Motor cortex rTMS can treat intractable PHN that did not respond to initial drug and radiofrequency therapies.
Core Tip: Postherpetic neuralgia (PHN) is a kind of refractory neuropathic pain, which seriously affects the quality of life. Repetitive transcranial magnetic stimulation can be used as an effective complement to the treatment of patients with refractory PHN.
- Citation: Wang H, Hu YZ, Che XW, Yu L. Motor cortex transcranial magnetic stimulation to reduce intractable postherpetic neuralgia with poor response to other threapies: Report of two cases. World J Clin Cases 2023; 11(9): 2015-2020
- URL: https://www.wjgnet.com/2307-8960/full/v11/i9/2015.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i9.2015
Postherpetic neuralgia (PHN) is a typical neuropathic pain condition that appears in the lesioned skin regions following the healing of shingles[1]. The pain condition tends to persist, which is often accompanied by negative emotions (e.g., anxiety and depression) and substantially reduces the quality of life[1]. In addition to analgesia (e.g., pregabalin and gabapentin), nerve radiofrequency technology is a effective treatment for intractable PHN[2,3]. However, there is still a significant portion of patients who do not benefit from this treatment.
As a non-invasive form of brain stimulation, repetitive transcranial magnetic stimulation (rTMS) targeting the motor cortex (M1) is able to reduce neuropathic pain with grade A evidence[4]. Here we report two cases in which motor cortex rTMS was used to treat intractable PHN that did not respond to initial drug and radiofrequency therapies. Moreover, we specifically investigated rTMS efficacy at 3 mo following treatment[4].
Case 1: A 65-year-old woman was admitted with persistent pain in the left chest and back (T5/T6) for 6 mo after herpes zoster.
Case 2: A 75-year-old woman was admitted with left lower back pain (T11/12) for 4 mo after herpes zoster.
Case 1: The patient’s pain was characterized by persistent tingling and burning sensations, with a visual analog scale (VAS) score of 8. She was prescribed pregabalin 150 mg bid, but she did not want to continue increasing the dose of the drug because of the side effect of dizziness, and received a spinal nerve radiofrequency surgery. However, there was no clear analgesia following these treatments.
Case 2: The patient was prescribed gabapentin 0.6 g tid. However, she had renal insufficiency so the drug dose was not increased further, as well as a spinal nerve radiofrequency surgery. The patient reported slight pain relief after treatment but still with a VAS score of 6.
Case 1: The patient claimed no history of past illness.
Case 2: The patient had a history of renal insufficiency for 5 years and was on drugs regularly.
Neither patient had any relevant personal or family history.
Physical examination of both patients revealed no abnormalities.
Laboratory examination of both patients revealed no abnormalities.
Imaging examination of both patients revealed no abnormalities.
PHN.
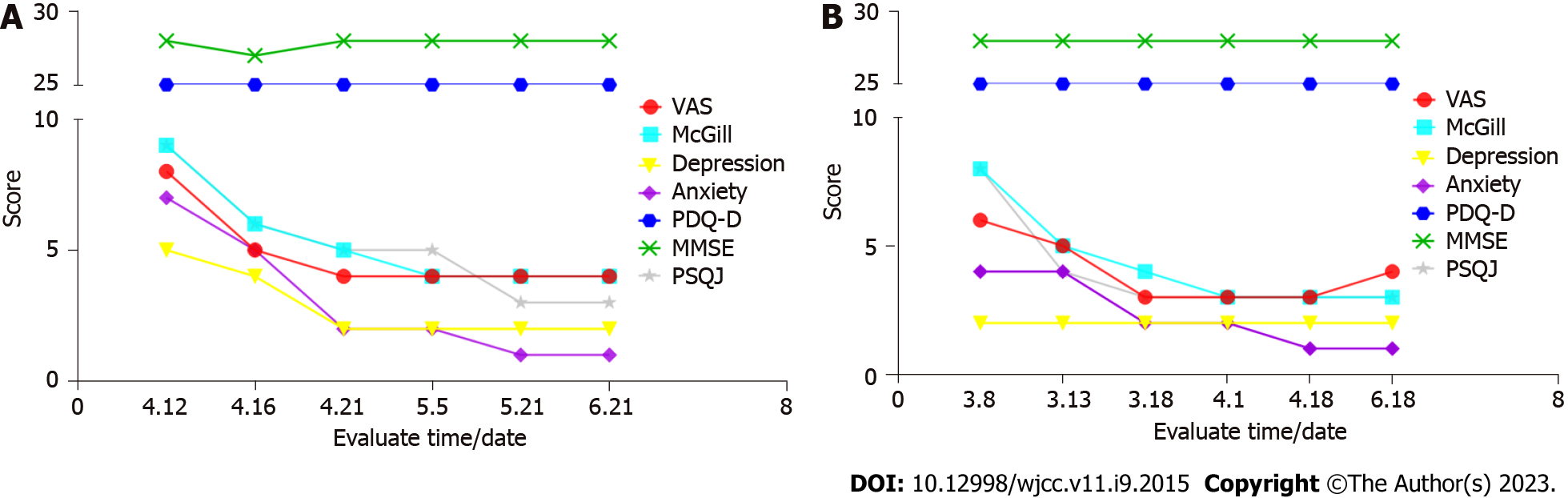
Both patients provided written informed consent for rTMS treatment. rTMS was delivered to the contralateral motor cortex once daily for 10 consecutive days using an RT-50 stimulation system connected to a figure-of-eight coil (Sichuan Junjian Wanfeng Medical Equipment Co.). Each rTMS session delivered 3000 pulses at 10 Hz with 5-sec trains and 25-sec intervals at 100% resting motor threshold. Patients were assessed at baseline, the fifth treatment, the end of treatment, and 2 wk, 1 mo, and 3 mo after treatment. Clinical assessment included VAS, McGill Pain Questionnaire (McGill), Pittsburgh Sleep Quality Index (PSQI), Hamilton Depression Scale (24 items), Hamilton Anxiety Scale (17 items), Mini-mental State Examination (MMSE), and Perceived Deficits Questionnaire-Depression (PDQ-D). Drug dose remained the same as that before this treatment.
Both patients demonstrated a promising analgesia effect, with pain experience changing from severe to mild-to-moderate level (Figure 1). There was also a protect effect on negative emotions, especially in the first case with an initial mild depressive symptom. We also observed a significant improvement in sleep quality in both cases. More importantly, the protective effects of motor cortex rTMS lasted for 3 mo following treatment (Figure 2).
Here we report two cases in which motor cortex rTMS was able to significantly reduce intractable PHN that did respond to first-line drug and radiofrequency therapies. Drugs and radiofrequency therapies are first-line treatments in clinical settings for PHN[5]. Our results indicated that motor cortex rTMS could be considered when the pain become intractable and/or the patient does not seem to benefit from regular drug and radiofrequency therapies. Some studies have shown that rTMS treatment is safe for patients with PHN and has better efficacy at 10 Hz[6], which is the frequency that we chose for these two patients. More importantly, our results indicated a long-term analgesic effect for 3 mo. Most previous studies have shown that pain relief from neuroplasticity can last for several days, usually a week to a month, after transcranial magnetic stimulation treatment[4]. This long-term 3-mo effect was potentially associated with a relatively large dose of pulses in daily treatment[7]. Previous studies tended to deliver approximately 1500 daily pulses whereby the number of pulses was doubled in these two cases.
TMS is a non-invasive stimulation technique that produces analgesic effects similar to those of invasive techniques by targeting rTMS to M1[8]. High-frequency rTMS delivered to M1 areas obtains analgesic effects by modulating several distant brain regions involved in the processing or control of nociceptive information. This pain relief can last for several weeks beyond the duration of stimulation, especially during repetition, and may be related to the process of long-term synaptic plasticity[9]. rTMS is now mainly used for the treatment of neuropathic pain and requires a trained physician or nurse to perform this procedure, which is a technique that can be widely used. The most common side effects are dizziness and scalp discomfort, which are transient and disappear after the treatment.
The mechanism of rTMS analgesia remains an open question. There is evidence that motor cortex rTMS could drive top-down pain modulation[10]. In addition, motor cortex stimulation is also able to activate cortical and subcortical regions (e.g., insular and cingulate cortex) involved in the processing of affective-emotional aspects of pain[11]. In either case, cortical and/or subcortical responses to rTMS may help explain the poor response to radiofrequency therapies, in which spinal nerves may not be well damaged by the surgery or become recurrent following surgery.
We have also observed a promising effect on negative emotions in these two cases. This is in line with the finding of a study that rTMS treatment had a significant effect on the whole brain functional network in PHN patients with inhibited sensory-motor functions and improvements in mood, cognitive, emotional, and memory functions[12]. rTMS has been approved by the United States Food and Drug Administration to treat depression by targeting the dorsolateral prefrontal cortex. Recent studies have also tried to manage comorbid pain and depression with rTMS in one setting[13]. In addition, we provide an interesting finding that motor cortex rTMS is able to improve sleep quality in the two cases, which has been rarely investigated compared to evidence on depression and neuropathic pain[14,15].
To conclude, we provide two cases in which motor cortex rTMS is able to reduce pain sensations in intractable PHN when first-line drug and radiofrequency therapies had no clear benefits. These findings need to be further validated in large, randomized controlled trials.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Clinical neurology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Higa K, Japan; Shelat VG, Singapore S-Editor: Liu JH L-Editor: Wang TQ P-Editor: Liu JH
| 1. | Gross GE, Eisert L, Doerr HW, Fickenscher H, Knuf M, Maier P, Maschke M, Müller R, Pleyer U, Schäfer M, Sunderkötter C, Werner RN, Wutzler P, Nast A. S2k guidelines for the diagnosis and treatment of herpes zoster and postherpetic neuralgia. J Dtsch Dermatol Ges. 2020;18:55-78. [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 2. | Makharita MY, El Bendary HM, Sonbul ZM, Ahmed SES, Latif MA. Ultrasound-guided Pulsed Radiofrequency in the Management of Thoracic Postherpetic Neuralgia: A Randomized, Double-blinded, Controlled Trial. Clin J Pain. 2018;34:1017-1024. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Huang X, Ma Y, Wang W, Guo Y, Xu B, Ma K. Efficacy and safety of pulsed radiofrequency modulation of thoracic dorsal root ganglion or intercostal nerve on postherpetic neuralgia in aged patients: a retrospective study. BMC Neurol. 2021;21:233. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Lefaucheur JP, André-Obadia N, Antal A, Ayache SS, Baeken C, Benninger DH, Cantello RM, Cincotta M, de Carvalho M, De Ridder D, Devanne H, Di Lazzaro V, Filipović SR, Hummel FC, Jääskeläinen SK, Kimiskidis VK, Koch G, Langguth B, Nyffeler T, Oliviero A, Padberg F, Poulet E, Rossi S, Rossini PM, Rothwell JC, Schönfeldt-Lecuona C, Siebner HR, Slotema CW, Stagg CJ, Valls-Sole J, Ziemann U, Paulus W, Garcia-Larrea L. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS). Clin Neurophysiol. 2014;125:2150-2206. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1225] [Cited by in F6Publishing: 1240] [Article Influence: 124.0] [Reference Citation Analysis (0)] |
| 5. | Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, Gilron I, Haanpää M, Hansson P, Jensen TS, Kamerman PR, Lund K, Moore A, Raja SN, Rice AS, Rowbotham M, Sena E, Siddall P, Smith BH, Wallace M. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015;14:162-173. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2249] [Cited by in F6Publishing: 2197] [Article Influence: 244.1] [Reference Citation Analysis (0)] |
| 6. | Pei Q, Wu BS, Tang YZ, Yang XH, Song LP, Wang N, Li Y, Sun CL, Ma SM, Ni JX. Repetitive transcranial magnetic stimulation at different Frequencies for postherpetic neuralgia: a double-bind, sham-controlled, randomized trial. Pain Physician. 2019;22:E303-E313. [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Cruccu G, Garcia-Larrea L, Hansson P, Keindl M, Lefaucheur JP, Paulus W, Taylor R, Tronnier V, Truini A, Attal N. EAN guidelines on central neurostimulation therapy in chronic pain conditions. Eur J Neurol. 2016;23:1489-1499. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 149] [Cited by in F6Publishing: 159] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 8. | Lefaucheur JP, Drouot X, Keravel Y, Nguyen JP. Pain relief induced by repetitive transcranial magnetic stimulation of precentral cortex. Neuroreport. 2001;12:2963-2965. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 233] [Cited by in F6Publishing: 213] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 9. | Hosomi K, Sugiyama K, Nakamura Y, Shimokawa T, Oshino S, Goto Y, Mano T, Shimizu T, Yanagisawa T, Saitoh Y; TEN-P11-01 investigators. A randomized controlled trial of 5 daily sessions and continuous trial of 4 weekly sessions of repetitive transcranial magnetic stimulation for neuropathic pain. Pain. 2020;161:351-360. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 29] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 10. | Lefaucheur JP, Drouot X, Menard-Lefaucheur I, Zerah F, Bendib B, Cesaro P, Keravel Y, Nguyen JP. Neurogenic pain relief by repetitive transcranial magnetic cortical stimulation depends on the origin and the site of pain. J Neurol Neurosurg Psychiatry. 2004;75:612-616. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 247] [Cited by in F6Publishing: 229] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 11. | Moisset X, de Andrade DC, Bouhassira D. From pulses to pain relief: an update on the mechanisms of rTMS-induced analgesic effects. Eur J Pain. 2016;20:689-700. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 87] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 12. | Pei Q, Zhuo Z, Jing B, Meng Q, Ma X, Mo X, Liu H, Liang W, Ni J, Li H. The effects of repetitive transcranial magnetic stimulation on the whole-brain functional network of postherpetic neuralgia patients. Medicine (Baltimore). 2019;98:e16105. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | Leung A, Shirvalkar P, Chen R, Kuluva J, Vaninetti M, Bermudes R, Poree L, Wassermann EM, Kopell B, Levy R; and the Expert Consensus Panel. Transcranial Magnetic Stimulation for Pain, Headache, and Comorbid Depression: INS-NANS Expert Consensus Panel Review and Recommendation. Neuromodulation. 2020;23:267-290. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 50] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 14. | Nardone R, Sebastianelli L, Versace V, Brigo F, Golaszewski S, Pucks-Faes E, Saltuari L, Trinka E. Effects of repetitive transcranial magnetic stimulation in subjects with sleep disorders. Sleep Med. 2020;71:113-121. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 15. | Guo J, Chen X, Lyu Z, Xiu H, Lin S, Liu F. Repetitive transcranial magnetic stimulation (rTMS) for post-stroke sleep disorders: a systematic review of randomized controlled trials. Neurol Sci. 2022;43:6783-6794. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |