Abstract
Background
Sarcopenia is highly prevalent in the older population and is associated with several adverse health outcomes. Equipment to measure muscle mass and muscle strength to diagnose sarcopenia is often unavailable in clinical practice due to the related expenses while an easy physical performance measure to identify individuals who could potentially have sarcopenia is lacking.
Objectives
This study aimed to assess the association between physical performance measures and definitions of sarcopenia in a clinically relevant population of geriatric outpatients.
Design, setting and participants
A cross-sectional study was conducted, consisting of 140 community-dwelling older adults that were referred to a geriatric outpatient clinic. No exclusion criteria were applied.
Measurements
Physical performance measures included balance tests (sideby- side, semi-tandem and tandem test with eyes open and -closed), four-meter walk test, timed up and go test, chair stand test, handgrip strength and two subjective questions on mobility. Direct segmental multi-frequency bioelectrical impedance analysis was used to measure muscle mass. Five commonly used definitions of sarcopenia were applied. Diagnostic accuracy was determined by sensitivity, specificity and area under the curve.
Results
Physical performance measures, i.e. side-by-side test, tandem test, chair stand test and handgrip strength, were associated with at least one definition of sarcopenia. Diagnostic accuracy of these physical performance measures was poor.
Conclusions
Single physical performance measures could not identify older individuals with sarcopenia, according to five different definitions of sarcopenia.
Similar content being viewed by others
Introduction
Prevalence rates of sarcopenia, defined as age-related low muscle mass and muscle strength, vary between 0% and 15% in healthy older individuals and between 2% and 34% in geriatric outpatients, depending on the applied definition (1). Sarcopenia is associated with decreased mobility, a higher risk of falls, dependency in activities of daily living, morbidity and mortality (2–4). Although there is no consensus yet on the definition of sarcopenia, the majority of definitions contain a measure of muscle mass and/or muscle strength (5–10).
Equipment to measure muscle mass and muscle strength is often unavailable in clinical practice due to the related expenses (11). Poor physical performance has been shown to be associated with sarcopenia (12–14). Recently, a prediction model was proposed to identify sarcopenia with the use of demographic parameters and physical performance measures (15). However, such a prediction model is time consuming due to its inclusion of multiple physical tests and complex calculations. Identifying individuals who could potentially have sarcopenia in clinical practice would be greatly facilitated when an easy to use physical performance measure could be applied to identify individuals with sarcopenia. This could lead to the identification of individuals who could potentially have sarcopenia, who could then be referred to diagnose sarcopenia.
This study aims to assess the association between physical performance measures and different definitions of sarcopenia in a clinically relevant population of geriatric outpatients.
Methods
Study design
This cross-sectional study consisted of 140 community-dwelling older adults who were referred to a geriatric outpatient clinic of a middle-sized teaching hospital (Bronovo, The Hague, The Netherlands) between March 2011 and January 2012. These older adults were referred because of mobility problems for a comprehensive geriatric assessment. The study originally consists of 299 older adults, but muscle mass measurements were only available in 140 older adults as these measurements were later added as part of clinical care. No exclusion criteria were applied; inclusion was based on referral. The study was approved by the Medical Ethical Committee of the Leiden University Medical Center (Leiden, the Netherlands). Informed consent was waived as this study was based on regular care.
Study population characteristics
Medical charts were used to retrieve information on age, sex and medical history. Medical history included information on the presence of: hypertension, myocardial infarction, chronic obstructive pulmonary disease, diabetes mellitus, rheumatoid- or osteoarthritis, Parkinson’s disease and malignancy. The presence of two or more of these diseases was defined as multimorbidity. Anthropometric measurements included height and body weight and were measured to the nearest 0.1 decimal. Cognitive functioning was measured by the Mini Mental State Examination (MMSE) resulting in a score ranging from 0 to 30 points, higher scores indicating better cognitive function (16).
Physical performance measures, objective
Physical performance measures included balance tests, fourmeter walk test, timed up and go (TUG), chair stand test (CST) and handgrip strength (HGS).
Balance tests were performed in three different positions (side-by-side, semi-tandem and tandem) according to the protocol of the Short Physical Performance Battery (17), and were performed with eyes open and with eyes closed. Individuals were classified as unable to maintain for ten seconds (0) and able to maintain for ten seconds (1). Tandem balance test with eyes closed was excluded from the present analysis as the number of individuals who were able to maintain in the tandem position for ten seconds was less than five individuals.
Gait speed was obtained by a four-meter walk test where individuals were asked to walk at their usual pace (17). The best performance of two measurements was used and expressed in meters per second.
The TUG measures the time in seconds needed to stand up from a sitting position without using hands, walk three meters, walk around a cone, walk three meters back and return to sitting position without using hands, as fast as possible.
The CST measures the time in seconds needed to stand up five times from sitting position to a straight standing position and sit down again while keeping the arms crossed over the chest, as fast as possible (17).
HGS was measured using a hydraulic handheld dynamometer (Jamar, Sammons Preston, Inc., Bolingbrook, IL, USA). Individuals were asked to squeeze as hard as possible three times with the right and left hand side alternately. Maximal HGS of the three trials was used for analysis (18) and expressed in kilograms.
Higher gait speed and HGS implied a better physical performance while a higher TUG and CST time implied a lower physical performance. For all physical performance measures, all individuals who could not perform or finish the test or used hands to stand up from a sitting position, were given a time of 100 seconds.
Physical performance measures, subjective
In addition to the objective physical performance measures, two questions were asked: 1) Falls: “Did you fall in the past year?” (yes/no) and 2) Difficulty with walking: “Do you experience difficulty with walking?” (yes/no).
Sarcopenia definitions
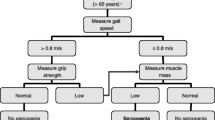
Muscle mass was measured using direct segmental multi-frequency Bioelectrical Impedance Analysis (DSM-BIA; InBody 720, Biospace Co., Ltd, Seoul, Korea) (19). Five definitions of sarcopenia were used to examine the association between physical measures and sarcopenia: 1) Baumgartner et al. using appendicular lean mass (ALM) divided by height2 (5); 2) Janssen et al. using relative skeletal muscle mass (SM) (SM divided by body mass) (6); 3) European Working Group on Sarcopenia in Older Persons (EWGSOP) using an algorithm of gait speed, HGS and skeletal muscle index (SMI; SM divided by height2) (7); 4) Foundation for National Institutes of Health (FNIH) definition one using HGS and ALM divided by body mass index (BMI) (8) and 5) The International Working Group on Sarcopenia (IWGS) using gait speed and ALM divided by height2 (9).
Statistical analysis
Continuous variables were reported by mean ± standard deviation (SD) if data was normally distributed or median [interquartile range (IQR)] for skewed distributions. Associations between physical performance measures (independent variables) with definitions of sarcopenia (dependent variables) were analyzed with binary logistic regression analysis. Two models were used: the crude model and an adjusted model for sex and age. P-values of less than 0.05 were considered statistically significant.
For the statistically significant associations between physical performance measures and definitions of sarcopenia, sensitivity, specificity and the area under the curve (AUC) were calculated to determine the diagnostic accuracy. Sensitivity and specificity were defined as low <70%, moderate 70–90% and high >90%. AUC was defined as low <0.70, acceptable 0.70–0.80, excellent 0.80–0.90 and outstanding >0.90. To test diagnostic accuracy, CST and HGS were dichotomized: CST ≥13 seconds (14, 20), and HGS <20 kilograms for females and <30 kilograms for males were considered low (21). Statistical analyses were performed using Statistical Package for Social Sciences (SPSS Inc, Chicago, USA), version 22.
Results
Table 1 shows the characteristics of the geriatric outpatients, with a mean age of 80.9 (7.1) years and 42% males. Table 2 shows the applied definitions of sarcopenia and the prevalence of sarcopenia. Prevalence of sarcopenia ranged from 3.6% to 23.6%, depending on the definition.
Table 3 shows the association between physical performance measures and sarcopenia according to the applied definitions. Out of all balance tests, the ability to perform the tandem stance with eyes open was most often associated with a decreased likelihood to have sarcopenia (Baumgartner et al., EWGSOP and IWGS). CST was associated with sarcopenia by use of the EWGSOP and IWGS definitions. HGS was associated with sarcopenia using the definition of Baumgartner et al. and IWGS. The other physical performance measures i.e. semi-tandem balance test with eyes open and eyes closed, gait speed, TUG and the subjective physical performance measures did not show an association with any of the definitions of sarcopenia.
Table 4 shows the diagnostic accuracy for physical performance measures significantly associated with sarcopenia. The tandem balance test with eyes open showed moderate sensitivity and low specificity and AUC for all three sarcopenia definitions. The side-by-side test with eyes closed showed low sensitivity, moderate specificity and low AUC for the EWGSOP definition. CST showed low sensitivity, specificity and AUC for the EWGSOP and IWGS definitions. HGS showed low sensitivity, moderate specificity and low AUC for the Baumgartner et al. and IWGS definitions.
Discussion
Physical performance measures, i.e. side-by-side test, tandem test, CST and HGS, were associated with sarcopenia using several definitions, but diagnostic accuracy was poor.
Previous studies have shown that tandem balance test, gait speed, CST and HGS are valid and reliable measures to assess physical performance (22, 23). Moreover, gait speed, CST and HGS have proven to be associated with sarcopenia according to the EWGSOP definition in community dwelling older adults (20, 24, 25). Unfortunately, the results of this study in geriatric outpatients did not show a single suitable physical performance measure to identify older individuals with sarcopenia. For a test to be suitable to identify individuals with a high risk on sarcopenia, it needs to have a high sensitivity as especially false-negatives are undesirable. Sensitivity was low to moderate, which would mean that many individuals who could potentially have sarcopenia would be missed. Moreover, specificity and AUC were low and therefore single physical performance measures have poor diagnostic accuracy to identify individuals with sarcopenia.
Sarcopenia is associated with negative health outcomes and therefore an important diagnosis in clinical practice. Nutritional and physical interventions have proven to increase muscle mass, muscle strength and physical performance (26, 27). Improving physical performance measures might reduce the risk of sarcopenia and therewith its negative health outcomes. Early recognition of sarcopenia is necessary to initiate interventions. BMI is a measurement that is often used to identify individuals who are at risk of adverse health outcomes, however, BMI does not encompass the risk of sarcopenia (28) Another proposed screening tool to identify individuals with sarcopenia is the SARC-F, a simple five-item questionnaire (subjective measures of strength, assistance in walking, rise from a chair, climb stairs, falls). This is one of the screening instruments that is increasingly being used in community-dwelling middle-aged to older adults to identify individuals who could potentially have sarcopenia (29, 30).
Multimorbidity was high in this population of geriatric outpatients and this could be an explanation for the lack of diagnostic accuracy of physical performance measures to identify older individuals with sarcopenia because physical performance could also be inflicted by disease-specific mechanisms.
To the best of our knowledge, this is the first study outlining the association between various objective physical performance measures and several commonly used definitions of sarcopenia in a clinically relevant population of geriatric outpatients. Validated physical performance measures were used. Furthermore, the population is heterogeneous and no exclusion criteria were used which makes it a good representation of the actual older population visiting outpatient clinics. A limitation of this study could be that only BIA and not Dual Energy X-ray Absorptiometry (DEXA) was used to determine muscle mass parameters of sarcopenia. However, BIA and DEXA showed high agreement in a population of community-dwelling individuals (19).
Single physical performance measures could not identify older individuals with sarcopenia, according to five different definitions. Therefore, no easy and fast method to identify individuals with sarcopenia can be recommended. Future research should focus on developing and validating screening tools so that individuals with a high probability of having sarcopenia can be identified. Individuals who are considered to be at risk of sarcopenia should be referred to diagnose sarcopenia using the diagnostic criteria that are used in the definitions of sarcopenia.
Acknowledgements: We thank M. Stijntjes and J.H. Pasma for their contribution to the study.
Funding: This study was supported by the Dutch Technology Foundation STW, which is part of the Netherlands Organization for Scientific Research (NWO) and which is partly funded by the Ministry of Economic Affairs. Furthermore, this study was supported by the seventh framework program MYOAGE (HEALTH-2007-2.4.5-10) and 050-060-810 Netherlands Consortium for Healthy Aging (NCHA). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Statement of authorship: All authors have made substantial contributions to all of the following: 1) conception and design of the study, acquisition of data or analysis and interpretation of data; 2) drafting the article or revising it critically for important intellectual content; 3) final approval of the version to be submitted.
Conflict of Interest: S.M.L.M. Looijaard: none to declare. S.J. Oudbier: none to declare. E.M. Reijnierse: none to declare. G.J. Blauw: none to declare. C.G.M. Meskers: none to declare. A.B. Maier: none to declare.
References
Reijnierse EM, Trappenburg MC, Leter MJ, et al. The Impact of Different Diagnostic Criteria on the Prevalence of Sarcopenia in Healthy Elderly Participants and Geriatric Outpatients. Gerontology. 2015;61(6): 491–6.
Beaudart C, Reginster JY, Petermans J, et al. Quality of life and physical components linked to sarcopenia: The SarcoPhAge study. Exp Gerontol. 2015;69: 103–10.
Landi F, Liperoti R, Russo A, et al. Sarcopenia as a risk factor for falls in elderly individuals: results from the ilSIRENTE study. Clin Nutr. 2012;31(5): 652–8.
Landi F, Cruz-Jentoft AJ, Liperoti R, et al. Sarcopenia and mortality risk in frail older persons aged 80 years and older: results from ilSIRENTE study. Age Ageing. 2013;42(2): 203–9.
Baumgartner RN, Koehler KM, Gallagher D, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998;147(8): 755–63.
Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. 2002;50(5): 889–96.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39(4): 412–23.
Studenski SA, Peters KW, Alley DE, et al. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci. 2014;69(5): 547–58.
Fielding RA, Vellas B, Evans WJ, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. 2011;12(4): 249–56.
Janssen I, Baumgartner RN, Ross R, Rosenberg IH, Roubenoff R. Skeletal muscle cutpoints associated with elevated physical disability risk in older men and women. Am J Epidemiol. 2004;159(4): 413–21.
Reijnierse EM, de van der Schuere MAE, Trappenburg MC, Doves M, Meskers CGM, Maier AB. Lack of knowledge and availability of diagnostic equipment could hinder the diagnosis of sarcopenia and its management. PloS one. 2017;12(10):e0185837.
Martinez BP, Gomes IB, Oliveira CS, et al. Accuracy of the Timed Up and Go test for predicting sarcopenia in elderly hospitalized patients. Clinics. 2015;70(5): 369–72.
Bijlsma AY, Meskers CG, van den Eshof N, et al. Diagnostic criteria for sarcopenia and physical performance. Age. 2014;36(1): 275–85.
Pinheiro PA, Carneiro JA, Coqueiro RS, Pereira R, Fernandes MH. “Chai. Stand Test” as Simple Tool for Sarcopenia Screening in Elderly Women. J Nutr Health Aging. 2016;20(1): 56–9.
Gray M, Glenn JM, Binns A. Predicting sarcopenia from functional measures among community-dwelling older adults. Age. 2016;38(1): 22.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3): 189–98.
Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2): 85–94.
Reijnierse EM, de Jong N, Trappenburg MC, et al. Assessment of maximal handgrip strength: how many attempts are needed? J Cachexia Sarcopenia Muscle. 2017;8(3): 466–74.
Ling CH,de Craen AJ, Slagboom PE, et al. Accuracy of direct segmental multifrequency bioimpedance analysis in the assessment of total body and segmental body composition in middle-aged adult population. Clin Nutr. 2011;30(5): 610–5.
Nishimura T, Arima K, Okabe T, et al. Usefulness of chair stand time as a surrogate of gait speed in diagnosing sarcopenia. Geriatr Gerontol Int. 2017;17(4): 659–61.
Lauretani F, Russo CR, Bandinelli S, et al. Age-associated changes in skeletal muscles and their effect on mobility: an operational diagnosis of sarcopenia. J Appl Physiol. 2003;95(5): 1851–60.
Freiberger E, de Vreede P, Schoene D, et al. Performance-based physical function in older community-dwelling persons: a systematic review of instruments. Age Ageing. 2012;41(6): 712–21.
Stevens PJ, Syddall HE, Patel HP, Martin HJ, Cooper C, Aihie Sayer A. Is grip strength a good marker of physical performance among community-dwelling older people? J Nutr Health Aging. 2012;16(9): 769–74.
Sanchez-Rodriguez D, Marco E, Miralles R, et al. Does gait speed contribute to sarcopenia case-finding in a postacute rehabilitation setting? Arch Gerontol Geriatr. 2015;61(2): 176–81.
Stoever K, Heber A, Eichberg S, Brixius K. Sarcopenia and Predictors of Skeletal Muscle Mass in Elderly Men With and Without Obesity. Gerontol Geriatr Med. 2017;3:2333721417713637.
Verlaan S, Maier AB, Bauer JM, et al. Sufficient levels of 25-hydroxyvitamin D and protein intake required to increase muscle mass in sarcopenic older adults-The PROVIDE study. Clin Nutr. 2018;37(2): 551–7.
Beaudart C, Dawson A, Shaw SC, et al. Nutrition and physical activity in the prevention and treatment of sarcopenia: systematic review. Osteoporosis Int. 2017;28(6): 1817–33.
Thibault R, Genton L, Pichard C. Body composition: why, when and for who? Clin Nutr. 2012;31(4): 435–47.
Malmstrom TK, Miller DK, Simonsick EM, Ferrucci L, Morley JE. SARC-F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia, Sarcopenia Muscle. 2016;7(1): 28–36.
Rolland Y, Dupuy C, Abellan Van Kan G, et al. Sarcopenia Screened by the SARC-F Questionnaire and Physical Performances of Elderly Women: A Cross-Sectional Study. J Am Med Dir Assoc. 2017;18(10): 848–52.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Looijaard, S.M.L.M., Oudbier, S.J., Reijnierse, E.M. et al. Single Physical Performance Measures Cannot Identify Geriatric Outpatients with Sarcopenia. J Frailty Aging 7, 262–267 (2018). https://doi.org/10.14283/jfa.2018.19
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.14283/jfa.2018.19