Endocrinology and Diabetes Service, University Hospital Center "Mother Teresa", Tirana, Albania
The purpose of this study was to evaluate certain clinical aspects of hyperthyroidism in Albania, which is an iodine deficient country, as it is known that iodine intake may influence the type of thyroid hyperfunction. The files of sixty-six patients with thyrotoxicosis who were hospitalised for their disease were retrospectively analysed. 59.1% of these patients suffered from toxic multinodular goiter, 27.3% from Grave's disease (toxic diffuse goiter), 10.6% from toxic adenoma, 1.5% from iodide-induced hyperthyroidism and 1.5% from transient hyperthyroidism due to subacute thyroiditis. There was an increased female to male ratio (83.3% vs 16.7%, respectively, p<0.001). 83.9% of all hyperthyroid patients lived in cities, while 16.1% lived in villages. Ophthalmopathy was found in 11.1% of patients with Graves' disease, and thyrotoxic heart disease was found in 14% of patients with thyrotoxicosis. 71.9% of all patients with hyperthyroidism were treated with propylthiouracil (PTU), while 28.1% of them were treated with methimazole; 67.2% of all these patients also received propranolol hydrochloride, while 32.8% were prescribed atenolol. Compliance was lower than that reported in other studies as only 41% of all patients received their treatment regularly. Side effects from treatment with antithyroid drugs were as follows: 4.1% (2/48) of patients treated with propylthiouracil presented leukopenia with agranulocytosis, and 6.1% of them toxic hepatitis, while 11.1% (2/18) of patients treated with methimazole presented agranulocytosis. In conclusion, the mode of presentation and side effects of hyperthyroidism appears to be different in Albania when compared with other countries, probably as a result of iodine deficiency and/or possibly nutritional status. Compliance with treatment is lower than that reported in other series, while antithyroid drug side effects seem to be more frequent. The latter observation may be due to the fact that only hospitalised patients were analysed in this study.
Hyperthyroidism, Toxic nodular goiter, Graves' ophthalmopathy, Thyrotoxic heart disease, Anti-thyroid drugs, Beta-blocking drugs
INTRODUCTION
Hyperthyroidism is a clinical entity characterized by hyperfunctioning of the thyroid gland resulting in excessive production of thyroid hormones, thyroxine and triiodothyronine (T4 and T3), and increased levels of these hormones in the blood. Thyrotoxicosis is a term expressing the deleterious effects of excessively high levels of T3 and T4 on the human body.
In clinical practice, hyperthyroidism and thyrotoxicosis are often used interchangeably to describe the clinical syndrome resulting from high circulating levels of thyroid hormones.
Albania is a country where some iodine deficiency and hence increased incidence of goiter are still present; therefore, thyroid disorders including hyperthyroidism are probably the most frequently encountered endocrinopathies, if we exclude diabetes. The aim of this study was to evaluate some clinical aspects of thyrotoxicosis in hospitalised patients in this country in order to help understand diagnostic and therapeutic problems pertaining to these patients, which may be of general interest as well.
SUBJECTS AND METHODS
This is a retrospective study based on all patients who were hospitalised in the Endocrinology and Diabetes Service of UCH "Mother Teresa" for hyperthyroidism during the period January 2002 to December 2002. The medical records of 66 such patients were studied. The reason for hospitalization was not mentioned in the charts. The diagnosis of hyperthyroidism was based on signs and symptoms, free T3 and T4 and TSH levels in blood (measured by ELISA methods) and the findings of thyroid imaging by Scintigraphy (using either Iodine 123 or Tc99m pertechnetate) and ultrasonography. Thus, the diagnosis of Graves' disease (diffuse toxic goiter) was based on the aforementioned findings and did not involve immunological or genetic investigations.
Diagnosis and grading of ophthalmopathy was again based on eye signs and symptoms and ophthalmometry measurements, but autoantibodies measurements or Computerized Tomography of the orbit were not carried out.
Thyrotoxic heart disease was diagnosed on the basis of presence of atrial fibrillation and/or congestive heart failure presenting after diagnosis of thyrotoxicosis, and was confirmed independently by a cardiologist. The diagnosis of hepatotoxicity or agranulocytosis as side effects of antithyroid (AT) drugs were also confirmed by the respective specialists.
The diagnosis of subacute thyroiditis was again based on signs and symptoms of this disease, erythrocyte sedimentation rate and the thyrotoxicosis related laboratory investigation, while the diagnosis of iodide-induced thyrotoxicosis was based on history and the presence of signs and symptoms and laboratory findings of hyperthyrodism.
Statistical analysis was carried out by Student's t-test, binomial test and chi-square with Yates correction, as appropriate, and a p-value of 0.05 or smaller was used to consider any findings as statistically significant.
RESULTS
During the one-year period of the present investigation a total of 1071 patients were admitted to the Endocrinology and Diabetes Service of UCH "Mother Teresa". Of these 837 (or 78.2%) were diabetic and 66 (6.2%) were hyperthyroid. Thus diabetic patients are by far the most frequently hospitalized group of endocrinopathy in our facility (P<0.000001).
A much higher percentage of thyrotoxic patients were females as compared to males (55/66 versus 11/66 or 83.3% versus 16.7%, respectively, P<0.0001).
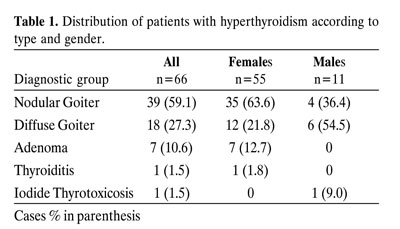
The breakdown of thyrotoxic patients according to type of thyrotoxicosis is shown in table 1. The most frequent type of hyperthyroidism (59.1%) was toxic nodular goiter, while diffuse goiter represented about half this frequency and autonomous adenoma was present in about 10% of the cases, these differences being statistically highly significant (P<0.0001). This relative frequency of the causes of thyrotoxicosis was also true of female patients, while male patients had a higher percentage of diffuse goiter. The sexual dimorphism with regard to the frequency of a different type of toxic goiter did not quite reach statistically significant levels (63.6% vs 21.8% in women and 36.3% vs 54.5% in men, x2 = 3.1, p=0.07, Table 1).
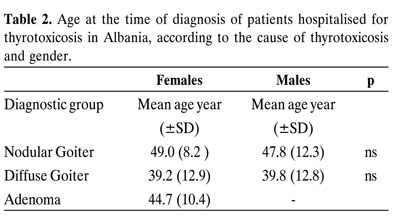
The mean age at diagnosis according to gender and type of thyrotoxicosis are shown in table 2. The differences in age were not statistically significant among the various groups.
Regarding the place of residence of these patients, 83.9% came from towns and only 16.1% from villages.
Two out of the eighteen patients with Graves' disease (11.1%) had severe ophthalmopathy while thyrotoxic heart disease was present in 8 out of 57 patients (14%) with toxic goiter (nodular and diffuse).
Forty-six out of 64 or 71.9 % of thyrotoxic patients given treatment were given Propylthiuracil (PTU), while only 18 out of 64 (28.1%) were under Methimazole treatment. The preference for PTU was statistically significant (p=0.007) and, as shown in table 3, was given irrespective of type of thyrotoxicosis. All patients under AT medication were also given beta blockers, propranolol hydrochloride being given in about two thirds of all cases, while the remaining one third were treated with atenolol (Table 3).

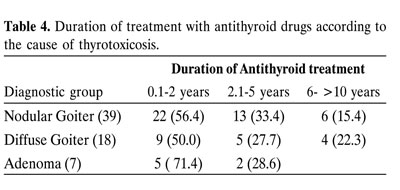
The duration of treatment with AT medication is shown in table 4 for the various groups of thyrotoxic patients. Regarding compliance, only 27 out of the 66 patients (41%) were treated regularly in consultation with their endocrinologist while the remaining 59% were not in regular consultation with a physician, on occasion interrupting their medication on their own.
Regarding AT drug side-effects, agranulocytosis was observed in 2 out of 48 patients on PTU (4.1%), while in patients treated with methimazole the percentage was somewhat higher (2 out of 18 or 11.1%). This difference however was not statistically significant (x2 = 1.1 p=0.29). Finally, hepatotoxicity was observed in the PTU group only (6%), 1/48 cases having hyperbilirubinaemia and 2 other cases showing increased levels of liver enzymes.
DISCUSSION
In our study we present data based on 66 thyrotoxic patients who were hospitalised in the Endocrinology and Diabetes Service of U.H.C. "Mother Teresa" during a period of one year. Although a much larger number of thyroid patients (incuding thyrotoxics) compared to other endocrinopathies are seen in our hospital, only a small percentage of them are hospitalised. The large majority of hyperthyroid patients in Albania, as in other countries, are investigated and treated as out-patients.
Since hospitalised patients, however, have more thorough investigation and better records, this investigation of thyrotoxicosis was based on in-patients, and we assumed that the sample is representative of the total cases of the various clinical forms of thyrotoxicosis in our endemic goiter country. However, one should take into account that data obtained form hospitalised patients may not exactly represent epidemiological data.
Based on our data, toxic multinodular goiter is the most frequent clinical form of thyrotoxicosis in comparison with other clinical forms of this disorder. Our data show a greater percentage of toxic multinodular goiter than the data of other authors, while for toxic adenoma, transient hyperthyroidism due to subacute thyroiditis and iodide-induced hyperthyroidism, our data are comparable with the data of other authors in the literature1-3.
Our data show that hyperthyroidism is more frequent in female patients than in male patients, a finding which is generally found in all other studies4-6. The same holds true with regard to the age of onset of hyperthyroidism7-9. Thus, Dougall McRoss4 reports that Graves' disease can occur at any age, though the highest incidence is at 40-60 years. The age of onset of hyperthyroidism was not different among males and females7-9.
Residence and way of life may influence the onset and course of many diseases. It is common knowledge that life in cities and towns is accompanied by much more emotional stress than in villages, and it is known that emotional stress may serve as a trigger factor for many diseases, especially of autoimmune nature. Our finding of a higher incidence of hyperthyroidism in urban as compared to rural population generally is compatible with the view that emotional negative stress can trigger Graves' disease, most likely because such stress can affect the immune system10. The population of villages from which the patients came is not known. However, is should be stated that the population of rural areas as a whole is equal to or greater than the towns population in Albania. However, it is possible that urban population is over-represented in our study because of greater awareness of thyroid problems as well as easier access to a large hospital in towns.
Ophtalmopathy of Graves' disease may also be encountered in patients with Hashimotos' thyroiditis or primary hypothyroidism11. About 3-5% of all patients with Graves' disease can present with severe ophthalmopathy12,13. Our data about ophthalmopathy show a higher incidence of this problem in comparison with the data of other authors12,13. We cannot offer a definite explanation for these differences of our figures in comparison with the figures of other authors, but probably this number is influenced by the type and quality (regularity) of treatment of our patients, as well as by the fact that our findings are based on in-patients, presumably a sub-population of hyperthyroid patients more likely to have the severest forms of this syndrome. Unfortunately, information about smoking habits was not available in our records.
It is a well known fact that hyperthyroidism may be harmful to the cardiovascular system as a consequence of direct action of the circulating high levels of T4 and T3 in the blood. This effect is clinically expressed with atrial fibrillation and/or congestive heart failure and constitutes the so-called thyrotoxic heart disease. It is potentially serious and can be associated with increased mortality in patients of all age groups14,15.
In elderly patients with heart failure or arrhythmias of recent onset, it is advisable to measure FT4 and TSH. Cobler et al16 found thyrotoxicosis to be the cause of atrial fibrillation in 31% of elderly institutionalized women and 11% of elderly men. Atrial fibrillation was present at the time of diagnosis in 10% of hyperthyroid patients reported by Williams17 and Mornex and Orgiazzi18, and in 19% in the report by Wayne19. Our data on cardiopathy in hyperthyroidism are similar to the data of other authors17,19-21.
Regarding the type of AT medication, thyroidologists in the USA preferably prescribe PTU by a ratio of more than 2:1. One explanation is the fact that PTU was introduced five years before methimazole so the experience with the former drug is greater. Another reason is the ability of PTU to inhibit the conversion of T4 to T3, a property not shared by methimazole. On the other hand, there are several reasons why methimazole may be selected over PTU, such as longer half-life and less hepatotoxicity. Thus, the choice of AT drugs seems to represent an individual choice based mainly on the physician's personal preferences and experience.
There are also national as well as individual preferences concerning which AT drug is used. While in the USA PTU is favored, in the UK and mainland European countries the drug of choice seems to be methimazole4. As we mentioned in the results section, our data concerning choice of AT drugs are similar to the findings of other authors4,22,23.
Beta adrenergic blocking drugs are also valuable in the treatment of hyperthyroidism, but in most cases they play a secondary role23. Propranolol hydrochloride is the drug that was originally used for thyrotoxicosis and is still used most widely, but there are a number of newer drugs of this class of a longer duration of action, or that are more cardio-selective, such as atenolol and metaprolol22.
Most studies report that the standard duration of treatment with AT drugs for Graves' disease is 12-18 months, and for toxic multinodular goiter this period is somewhat shorter24. Our findings are the same as to Graves' disease, but duration of treatment in our cases is longer for patients with toxic multinodular goiter and for toxic adenoma. This finding can be explained by the fact that our thyrotoxic patients with nodular disease prefer to prolong medical antithyroid therapy because they wish to avoid surgery. This is, of course, a matter of culture and personal preference.
The regularity of medical antithyroid treatment is primarily dependent on the cultural level of patients as well as a good relationship between Endocrinologists and their patients. In our series a greater percentage of patients were taking their AT medication irregularly, as compared to the data of other publications available to us4,22,23.
Finally, it is a well known fact that the use of antithyroid drugs can be associated with side effects. About 5% of patients reported in the literature experience minor side effects, such as skin rashes, arthralgias, gastrointestinal upset, and about 0.5-1% of patients develop major side effects such as agranulocytosis, hepatitis and vasculitis22,25-27. Hepatitis is associated with PTU, but apparently not with other antithyroid drugs25. Our data are in agreement with those of Hanson, J.S.28 with regard to the toxic hepatitis associated with PTU, though not methimazole, but differ as to the frequency of this complication, which is greater in our study (6% compared to reported 0.5-1%). Our figures with respect to the major side-effects of AT drugs are greater than the figures reported by other authors22,25-28. We think that these greater figures could probably be explained by the quality of antithyroid drugs that are used in Albania, but may also be attrib
uted to patient selection. It is obviously more likely for a patient with serious side-effects to be hospitalized.
In conclusion, our study shows that there are a number of demographic as well as clinical differences in the spectrum of the type of hyperthyroidism and side effects of therapy of hyperthyroidism in Albania, compared to other populations. These are most probably due to the fact that iodine deficiency is still present in the country and possibly to cultural reasons or nutritional factors. However, one should take into account the nature of our study which is retrospective and only based on hospitalized patients' data.
ACKNOWLEDGEMENTS
I would like to thank Prof. Maria ALEVIZAKI PhD for reviewing and editing of the manuscript.
I would also like to thank Prof. Ass. Dr. Jovan BASHO M.D. for statistical analyses of the results of this study, and Mr. Josif NDREÇKA for his technical assistance in the preparation of this study.
REFERENCES
1. Bransom CJ, Talbot CH, Henry L, et al, 1979 Solitary toxic adenoma of thyroid. Br J Surg 66: 590-595.
2. Hamburger JI, Hamburger SW, 1985 Diagnosis and management of large toxic multinodular goiter. J Nucl Med 26: 888-892.
3. Siegel RD, Lee SL, 1998 Toxic Nodular Goitre: Toxic adenoma and toxic multinodular goiter. Endocr Metab Clin North Am 27: 151-168.
4. Dougall Mc Ross I 1992 Hyperthyroidism In "Thyroid Disease in Clinical Practice". Oxford University Press, New York; pp, 82-162.
5. Hamburger JI, 1980 Evolution of toxicity in solitary non toxic autonomously functioning nodules. J Clin Endocrinol Metab 50: 1089-1093.
6. Psarras A, Papadopoulos SH, Livadas D, Pharmakiotis AD, Koutras DA, 1972 The single thyroid nodule. Br J Surg 59: 545-548.
7. Blum M, Shenkman L, Holander CS, 1975 The autonomous nodule of the thyroid: correlation of patient age, nodule size and functional status. Am J Med Sci 269: 43-50.
8. Burman KD, Earll JM, Johnson MC, et al, 1974 Clinical observations on the solitary autonomous thyroid nodule. Arch Intern Med 134: 915-919.
9. Goldstein R, Hart IR, 1983 Follow-up of solitary autonomous thyroid nodules treated with 131I. N Engl J Med 309: 1473-1476.
10. Bartrop RW, Lockhurst E, Lazarus L, et al, 1977 Depresed lymphocite function after bereavement. Lancet 1: 834-836.
11. Wyse EP, Mc Conahey WM, Woolner LB, et al, 1968 Ophtalmopathy without hyperthyroidism in patients with histologic Hashimoto's thyroiditis. J Clin Endocrinol Metab 28: 1623- 1629.
12. Burch B Henry 1996 Graves' Disease Ophtalmopathy In "Werner and Ingbar's The Thyroid". A Fundamental and Clinical Text. Lewis E. Braverman, Robert D Utiger (eds), Lippincott-Raven Publishers; pp, 536-553.
13. Gorman CA, 1983 Temporal relationship between onset of Graves' ophtalmopathy and diagnosis of thyrotoxicosis. Mayo Clin Proc 58: 515-519.
14. Parker JLW, Lawson DH, 1973 Death from thyrotoxicosis. Lancet 2: 894-895.
15. Magner JA, Clark W, Allenby P, 1988 Congestive heart failure and death in young women with thyrotoxicosis. West J Med 149: 86-91.
16. Cobler JL, Williams ME, Greenland P, 1984 Thyrotoxicosis in institutionalized elderly patients with atrial fibrillation. Arch Intern Med 144: 1758-1760.
17. Williams RH, 1946 Thiouracil treatment in thyrotoxicosis. J Clin Endocrinol Metab 41: 354-361.
18. Mornex R, Orgiazzi JJ, 1986 Hyperthyroidism In "The Thyroid Gland" M De Wisscher (ed), Raven Press, New York; pp, 269-279.
19. Wayne EJ, 1954 The Diagnosis of Thyrotoxicosis. Br Med J 1: 411-419.
20. Cooper DS 1996 Treatment of Thyrotoxiocosis In: "Werner and Ingbar's The Thyroid". A Fundamental and Clinical Text. Lewis E Braverman, Robert D Utiger (eds), Lippincott-Raven Publishers; pp, 713-734.
21. Klein I, Ojamaa K, 1998 Thyrotoxicosis and the heart. Endocr Metab Clin North Am 27: 51-62.
22. Klein I, Ojamaa K, 2001 Thyroid hormones and the cardiovascular system. N Engl J Med 344: 501-509
23. Mazzaferri EL, Reynolds JC, Young RL, et al, 1976 Propranolol as a primary therapy for thyrotoxicosis. Results of a long-term prospective trial. Arch Intern Med 136: 50-56.
24. Slingerland DW, Burrows BA, 1979 Long term antithyroid treatment in hyperthyroidism. JAMA 242: 2408-2410.
25. Cooper DS, 1984 Antithyroid drugs. N Engl J Med 311: 1353-1362.
26. Rosove MH, 1977 Agranulocytosis and antithyroid drugs. West J Med 126: 339-343.
27. Cooper DS, Goldmintz D, Levin AA, et al, 1983 Agranulocytosis associated with antithyroid drugs: effects of patient age and drug dose. Ann Intern Med 98: 26-29.
28. Hanson JS, 1984 Propilthyrouracil and hepatitis: two cases and a review of the literature. Arch Intern Med 44: 994-996.
Address correspondence and requests for reprints to:
Professor Feçor Agaçi Endocrinology and Diabetes Service,
University Hospital Center "Mother Teresa", Tirana, Albania,
Dibra Street Nr 372, Tirana, Albania
Received 27-10-03, Revised 20-11-03, Accepted 02-12-03