
Lateral mass screw placement in the atlas: description of a novel surgical technique, radiographic parameters, and review of the literature
Introduction
Instability of the atlantoaxial joint can result from numerous etiologies including trauma, infection, inflammation, or congenital anomalies. The goal of surgical intervention, however, is largely the same: stabilization, along with the best possible alignment. Dating as far back as the early 1900’s attempts have been made to stabilize the atlantoaxial joint. Mixter and Osgood (1) describe a method in which braided silk soaked in benzoin was used to connect the C1 arch with the spinous processes of C2 in a child with a unilateral dislocated C1-C2 joint. Gallie described his method of C1-C2 fusion using a single piece of iliac crest bone graft placed between C1 and C2, secured with a steel wire in a sublaminar fashion (2). In an attempt to improve the reported suboptimal non-union rates of the Gallie method (3), Brooks-Jenkins offered their modification, which consisted of wedging two separate pieces of iliac crest bone graft between C1 and C2 (4). Holness et al. (5) described usage of an interlaminar clamp as a method of fusion. These clamps were used to compress the lamina of C1 and C2 between bone graft.
By the early 1980s it was widely known that Gallie fusions offered good stability in flexion and extension movements but poor rotatory stability (6). As a way to improve this, Magerl and Seemann (7) described use of posterior transarticular screws in combination with a Gallie fusion. This technique proved useful as fusion rates increased (3,8,9), but it did not come without complications. Complications such as hypoglossal nerve injuries, vertebral artery injuries and even internal carotid artery injuries were noted with this technique due to anterior screw penetration (10-13). As technology in spine surgery advanced, along with higher quality imaging, so did the techniques of attempted stabilization. Goel et al. (14) utilized a posteriorly based plate and screw construct for stabilization of the C1-C2 joint. C1 lateral mass screws were placed, and C2 pars/pedicle screws were placed. This method called for significant dissection with removal of C2 ganglia to ensure adequate exposure. Utilizing minipolyaxial screws and rods, rather than a plate, Harms et al. (15) described a method of placing C1 lateral mass screws in conjunction with C2 pedicle screws. Unlike the transarticular screw, the combination of the C1 lateral mass screw along with the C2 screw is not limited by the need for anatomic alignment prior to instrumentation. C1 screws can be placed in most patients regardless of body habitus or spinal deformity and C2 screws can be placed via pars, pedicle, or translaminar entry points (3,6). The C1 and C2 joint can then be reduced after placement of the screws, utilizing a contoured rod or other method of manipulation such as gentle reduction with a Kocher or towel clamp.
Although placement of C1 lateral mass screws is commonly performed, dissection often involves identification of the midpoint of the C1 lateral mass, which can be prone to excessive venous plexus bleeding or nerve injury. The senior authors have identified a novel technique for safe, accurate, and reproducible insertion of C1 lateral mass screws minimizing bleeding or nerve injury. The purpose of this study was (I) assess the radiographic angle of safety medially and laterally for C1 lateral mass screw placement; (II) to describe a novel technique of C1 lateral mass screw insertion. We present the study in accordance with the STROBE reporting checklist (available at https://dx.doi.org/10.21037/jss-20-566).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics review board of the Regents of the University of Michigan (HUM00186483). Individual consent for this retrospective analysis was waived. We retrospectively identified adult patients presenting to our Level-1 trauma center for non-cervical trauma, in which a computed tomography (CT) of the cervical spine was obtained and determined to be normal by an attending radiologist. The CT scans were then carefully reviewed by two independent reviewers for evidence of traumatic or congenital abnormalities. Patients with evidence of either pathology were excluded from the study. Patients with history of prior cervical spine surgery were also excluded.
Radiographic measurements
The following radiographic measurements were made on CT scans:
- On the axial CT slice of the C1 lateral mass, the angle of safety medially and lateral of the C1 lateral mass (bilaterally) with the reference point being the confluence of the posterior arch and lateral mass (Figure 1A).
- The length and width of the C1 lateral masses (Figure 1B,1C).
Statistical analysis
Averages of the medial and lateral angle of safety were obtained and reported below.
Results
Radiographic measurements
Forty-five patients with a mean age of 52.6±25.6 years (33% female) were included in the final analysis. The mean medial angle of safety of both the right and left lateral masses was 23±3.8 degrees. The mean lateral angle of safety of both the right and left lateral masses was 32±5 degrees. Angle of safety is defined as arc from a direct posterior to anterior reference line, centered at confluence of posterior arch and lateral mass to neural elements (medially) or vertebral artery (laterally). Average length and width of both lateral masses were 17.7 and 13.3 mm respectively. Table 1 depicts the radiographic measurements.
Table 1
| Parameter | Left lateral mass | Right lateral mass | |||||||
|---|---|---|---|---|---|---|---|---|---|
| AM (degrees) | AL (degrees) | Length (mm) | Width (mm) | AM (degrees) | AL (degrees) | Length (mm) | Width (mm) | ||
| Mean ± SD | 22.2±3.7 | 32.6±5.3 | 17.7±1.7 | 13.3±1.3 | 23.8±3.7 | 31.9±5.0 | 17.9±2.0 | 13.4±1.4 | |
| Min | 13.0 | 19.0 | 14.2 | 10.1 | 15.0 | 19.0 | 14.6 | 10.2 | |
| Max | 30.0 | 43.0 | 21.5 | 16.6 | 33.0 | 45.0 | 23.3 | 17.6 | |
AM, angle of safety medially in degrees; AL, angle of safety laterally in degrees.
Description of novel technique
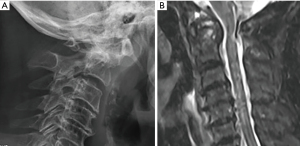
We present the case of an 82-year-old female who presented to our hospital after a ground level fall complaining of neck pain. Upon questioning she noted months of progressively worsening coordination, balance, and completion of fine motor tasks. Imaging performed revealed a subacute appearing dens fracture, significant cord signal changes and an anomalous vertebral artery at C2 (Figure 2A,2B). Imaging demonstrated C1–C2 instability with significantly reduced space available for the cord on upright cervical radiographs. She was consented for posterior stabilization and fusion from C1 to C4, with no fixation of C2 given her anomalous vertebral artery anatomy at C2.
Following appropriate informed consent, the patient was brought into the operating room and intubated per anesthesia protocol. Fiberoptic or glidescope intubation may be utilized based on cervical stability. Neuromonitoring leads were placed and baselines obtained. A Mayfield clamp was secured and the patient was placed prone on the operative bed. Once again neuromonitoring signals are obtained to ensure no change from baseline. Stealth clamp was placed opposite of the Mayfield clamp and draped out sterile. After a standard time out, the surgical field was prepped and draped in a sterile fashion. Using fluoroscopy incision is marked from C1 down to the appropriate level as indicated. After skin incision, meticulous subperiosteally dissection is performed. A solution of normal saline is placed into the wound and O-arm (Medtronic, Minneapolis, MN, USA) spin is performed. Dissection below the C1 arch is performed, with careful attention to start at the midline and work laterally. A curved curette was placed under the C1 arch, and dissection is carefully carried out laterally to identify the confluence of the medial aspect of the posterior arch and lateral mass. This confluence was then marked out as the C1 screw start point. Bleeding is controlled with Gelfoam patties and thrombin. A navigated probe is used to determine optimal screw length. In a large majority of patients, the C2 dorsal root ganglion is retracted inferior to protect it during screw insertion. Due to the medial starting point, screws are not angled in the coronal plane and are inserted at zero degrees. Further, the slightly medial starting point limits the amount of retraction on the C2 nerve, thus minimizing postoperative C2 neuralgia. Using a combination of fluoroscopy and navigation, a sequential series of burr, ball-tip feeler, navigated drill, tap, and screw is performed. If any venous bleeding occurs this is managed with a combination of hemostatic agents and bipolar cautery. At this point progression of the case ensues depending on what pathology is being addressed during the case.
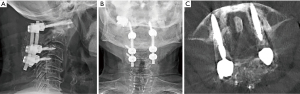
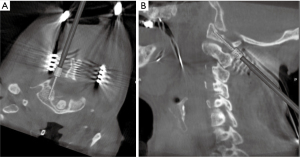
The patient underwent safe and efficacious stabilization of her atlantoaxial instability. Figure 3A-3C shows postoperative upright radiographic following stabilization and axial CT scan and cut at level of lateral mass. Figure 4A,4B display an intra-operative O-arm guided C1 lateral mass screw insertion with zero degrees of angulation and a start point at the confluence of the medial aspect of posterior arch of C1 and lateral mass. Given her poor bone quality, she was immobilized in a hard collar for 6 weeks.
Discussion
Surgeons of the cervical spine must have thorough knowledge of the anatomy of the C1-C2 region to avoid complications. In most cases, C1 lateral mass anatomy is predictable and, in most individuals, lateral mass screws can be safely placed (16,17). Pre-operative advanced imaging is often obtained to evaluate for any anatomic variations, and to evaluate bony morphology. This study demonstrates that utilizing a directly posterior to anterior oriented lateral mass screw at the C1 level is safe and if sized appropriately will not violate the bony cortex of the lateral mass. Due to its orientation, the starting point of the screw as compared to prior publications will also have to be altered.
The advantages of the proposed new entry point compared to the entry point used by most surgeons are numerous. Due to its location at a bony intersection, this technique is easier, to be reproduced rather than attempting to identify the center of the lateral mass. There is no need for angulation to avoid the vital medial or lateral structures. Also, with minimal posterior dissection, the risk of injury to the venous plexus or the C2 nerve root is minimized as bony landmarks will guide placement of the screw.
Sectioning or neurectomy of the C2 nerve root allows for better visualization of the C1-C2 joint but this does not come without a cost. Witiw et al. (18), performed a prospective questionnaire study of twenty-eight patients undergoing placement of C1 lateral mass screws. Eight patients underwent transection and in twenty cases the C2 nerve was preserved. They concluded that C2 trans-sectioning was associated with decrease operative time, decreased blood loss, and occipital numbness. They noted that this occipital numbness had no impact on patient reported quality of life. In those cases, where the C2 nerve root was preserved, those patients reported occipital neuralgia, had higher scores on mean disability surveys, and negatively impacted patient disability and quality of life scores.
Resnick et al. performed a cohort study on 60 consecutive patients undergoing standard computed tomography (CT) scans of their cervical spine. He noted a mean length of the C1 lateral mass screw that could be placed as 26±2 mm, and a mean diameter of 7±1.6 mm (17). These screws would be fully contained within the bone, though the authors note with shorter screws there is increased leeway from lateral mass breaching. Building upon this Christensen et al. (19) sought to determine if 3.5 mm cortical screws could safely and reliably be placed in the lateral mass of C1. Using 120 C1 vertebrae he documented various mean dimensions of the lateral mass. They noted a mean anterior-posterior dimension of 16.93 mm, a mean medial-lateral dimension of 8.68 and a mean cranial-caudal working dimension of 8.99. Working dimension entails measurements from the bottom of the inferior facet to the cranial aspect of the posterior arch at the level of the vertebral artery groove. Ebraheim et al. (20) meticulously studied this region of the C1 arch and the vertebral artery groove. The authors noted that in fifty dry C1 vertebrae (twenty-eight males, twenty-two female) the most medial aspect of the groove was located on average 10.4 and 8.9 mm from midline for males and females respectively. They also concluded that dissection over the ring should be limited to 12 mm from midline but dissection on the superior aspect of the ring should be limited to 8 mm to avoid injury to vertebral artery. Large amounts of venous bleeding can occur with safe dissection of undersurface of C1 posterior arch. If dissection of the is carried out to aggressively into the lateral gutter of the C1 lateral mass, injury to not only the C2 ganglion can occur but also the vertebral artery. Injury of the vertebral artery at this level can lead to significant blood loss, neurological impairment due to altered blood flow to the brain and even death.
The key anatomic landmark for accurate placement of the C1 lateral mass screw is the C1-C2 joint (15). In the Harms et al. (15) method the C2 dorsal root ganglion is retracted inferiorly at this point, while in Goel’s method (14) the C2 ganglion is sacrificed. Harms (15) called for a start point at the inferior border of the posterior arch of C1 and the midpoint of the C1 lateral mass. Goel (14) on the other hand inserted the screw at the center of the posterior surface of the lateral mass, 1–2 mm cranial to the C1-C2 facet. The screws are angled approximately 15 degrees medially (towards anterior arch of C1) and approximately 30 degrees cranially according to Goel (14). Harms suggested that no angulation of the screw was needed, while others debated the optimal angulation of C1 lateral mass screw (6,15,19,21,22). Both angulation and the start point of the ideal C1 lateral mass screw has debated, with no clear consensus of the ideal angulation and location. Hu et al. (22) attempted determine an anatomical optimal entry point and medial angulation of C1 lateral mass screws. In their anatomic study, using volumetric and three-dimensional cephalometric imaging they performed an analysis of 70 patients. They determined that the ideal medial angulation of a C1 lateral mass screw was 20.86 degrees and the ideal start point was at the center of the posterior surface of the inferior articular process, about 2 mm cranial to the articular surface. In a similar study Blagg et al. (23) performed an anatomic study on fifty patients undergoing CT scans on their cervical spines. His group noted the safest entry point to be at the junction of the medial edge of the posterior arch and the lateral mass. Screws here should be inserted parallel to the posterior arch and angled 20 degrees medially. Utilizing this method, they noted a mean distance of 8.8 mm between vertebral artery foramen laterally and the screw. As an alternative to starting screw insertion directly on the lateral mass, methods of C1 screw placement through the posterior arch were described (19,24-26). Lin et al. (27) performed a radiological study comparing the feasibility and safety of the various techniques for lateral mass screw placement via the posterior arch. Using thin cut CT scans and virtual surgery soft wear, virtual lateral mass screws were placed according to described starting points in the literature (19,24-26). He concluded that none of the described techniques are universally safe or feasible as there exists significant variability between each individual and their C1 vertebrae (27). They did note that limitations to the study were its purely radiological nature, and they arbitrary notion that safety was defined as lack of violation of anatomic structure.
Imaging navigation in spine surgery has been increasing in popularity since the 1990’s. Although not a substitute for understanding anatomy, navigation is helpful in cases of altered normal anatomy, or in cases where minimal dissection or exposure is desired (28,29). Advantages of utilization of navigation include; higher rates of acceptable screw placement and screw placement accuracy as compared to open or fluoroscopic techniques (30), and less overall radiation exposure to the surgeon and operative team as compared to traditional fluoroscopic methods (31-33). Disadvantages of navigation include, need for costly navigation machinery, operative staff training on devices, and the learning curve associated set up and utilization (34-36).
With the lack of a single “best” method of C1 lateral mass screw insertion, herein we present a novel method of C1 screw insertion via a navigated method. This method we believe is more reproducible as compared to other techniques as the start point is established via bony intersection. Furthermore, it avoids dissection on the superior aspect of the C1 arch, excessive lateral retraction of the C1 lateral mass, and minimizes soft tissue retraction. Imaging navigation improves screw placement accuracy, though not required for this technique.
Limitations
Several limitations she be noted in this study. This was a radiographic study in 45 healthy patients with cervical spine imaging. In the setting of instability due to degenerative processes, trauma or other etiologies, the anatomy may be altered. We understand that posterior to anterior screws with zero degrees of angulation may not be appropriate in all instances. Next, this was not a cohort study of patients, thus the biomechanics of the C1 lateral mass screw with zero degrees of angulation has not been compared to prior constructs. Further research is required to validate this method in a larger scale manner.
Conclusions
This study describes a novel method of C1 lateral mass screw placement starting at the confluence of the medial aspect of the posterior arch and lateral mass. Using radiographic measurements, we demonstrate that there is sufficient space for safe, accurate and reproducible C1 lateral mass screw placement using this technique. Further research is required to assess outcomes of patients utilizing this method as well as potential difference in fusion rates, complications, and pullout strength.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: We present the study in accordance with the STROBE reporting checklist (available at https://dx.doi.org/10.21037/jss-20-566).
Data Sharing Statement: Available at https://dx.doi.org/10.21037/jss-20-566
Peer Review File: Available at https://dx.doi.org/10.21037/jss-20-566
Conflict of Interest: All authors have completed the ICMJE uniform disclosure form (available at: https://dx.doi.org/10.21037/jss-20-566). PP reports personal fees from Globus, personal fees from NuVasive, grants from ISSG, grants from Depuy, personal fees from Allosource, personal fees from Medtronic, outside the submitted work. ISA reports Research Funding from OrthoFix, outside the submitted work. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics review board of the Regents of the University of Michigan (HUM00186483). Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mixter SJ, Osgood RB. IV. Traumatic Lesions of the Atlas and Axis. Ann Surg 1910;51:193-207. [Crossref] [PubMed]
- Gallie WE. Fractures and dislocations of the cervical spine. The American Journal of Surgery 1939;46:495-9. [Crossref]
- Bransford RJ, Lee MJ, Reis A. Posterior fixation of the upper cervical spine: contemporary techniques. J Am Acad Orthop Surg 2011;19:63-71. [Crossref] [PubMed]
- Brooks AL, Jenkins EB. Atlanto-axial arthrodesis by the wedge compression method. J Bone Joint Surg Am 1978;60:279-84. [Crossref] [PubMed]
- Holness RO, Huestis WS, Howes WJ, et al. Posterior stabilization with an interlaminar clamp in cervical injuries: technical note and review of the long term experience with the method. Neurosurgery 1984;14:318-22. [Crossref] [PubMed]
- Mummaneni PV, Haid RW. Atlantoaxial fixation: overview of all techniques. Neurol India 2005;53:408-15. [Crossref] [PubMed]
- Magerl F, Seemann PS. Stable posterior fusion of the atlas and axis by transarticular screw fixation. In: Kehr P, Weidner A. editors. Cervical Spine I. Vienna: Springer, Cervical Spine 1987:322-7.
- Haid RW Jr, Subach BR, McLaughlin MR, et al. C1-C2 transarticular screw fixation for atlantoaxial instability: a 6-year experience. Neurosurgery 2001;49:65-8; discussion 9-70. [PubMed]
- Henriques T, Cunningham BW, Olerud C, et al. Biomechanical comparison of five different atlantoaxial posterior fixation techniques. Spine (Phila Pa 1976) 2000;25:2877-83. [Crossref] [PubMed]
- Gluf WM, Schmidt MH, Apfelbaum RI. Atlantoaxial transarticular screw fixation: a review of surgical indications, fusion rate, complications, and lessons learned in 191 adult patients. J Neurosurg Spine 2005;2:155-63. [Crossref] [PubMed]
- Cyr SJ, Currier BL, Eck JC, et al. Fixation strength of unicortical versus bicortical C1-C2 transarticular screws. Spine J 2008;8:661-5. [Crossref] [PubMed]
- Wright NM, Lauryssen C. Vertebral artery injury in C1-2 transarticular screw fixation: results of a survey of the AANS/CNS section on disorders of the spine and peripheral nerves. American Association of Neurological Surgeons/Congress of Neurological Surgeons. J Neurosurg 1998;88:634-40. [Crossref] [PubMed]
- Currier BL, Todd LT, Maus TP, et al. Anatomic relationship of the internal carotid artery to the C1 vertebra: A case report of cervical reconstruction for chordoma and pilot study to assess the risk of screw fixation of the atlas. Spine (Phila Pa 1976) 2003;28:E461-7. [Crossref] [PubMed]
- Goel A, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien) 1994;129:47-53. [Crossref] [PubMed]
- Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976) 2001;26:2467-71. [Crossref] [PubMed]
- Gupta T. Cadaveric morphometric anatomy of C-1 vertebra in relation to lateral mass screw placement. Surg Radiol Anat 2008;30:589-93. [Crossref] [PubMed]
- Resnick DK, Lapsiwala S, Trost GR. Anatomic suitability of the C1-C2 complex for pedicle screw fixation. Spine (Phila Pa 1976) 2002;27:1494-8. [Crossref] [PubMed]
- Witiw CD, Mansouri A, Badhiwala JH, et al. Journal Club: C2 Nerve Root Transection During C1 Lateral Mass Screw Fixation: Does It Affect Functionality and Quality of Life? Neurosurgery 2015;76:638-40. [Crossref] [PubMed]
- Christensen DM, Eastlack RK, Lynch JJ, et al. C1 anatomy and dimensions relative to lateral mass screw placement. Spine (Phila Pa 1976) 2007;32:844-8. [Crossref] [PubMed]
- Ebraheim NA, Xu R, Ahmad M, et al. The quantitative anatomy of the vertebral artery groove of the atlas and its relation to the posterior atlantoaxial approach. Spine (Phila Pa 1976) 1998;23:320-3. [Crossref] [PubMed]
- Simsek S, Yigitkanli K, Turba UC, et al. Safe zone for C1 lateral mass screws: anatomic and radiological study. Neurosurgery 2009;65:1154-60; discussion 60. [Crossref] [PubMed]
- Hu Y, Dong WX, Spiker WR, et al. An anatomic study to determine the optimal entry point, medial angles, and effective length for safe fixation using posterior C1 lateral mass screws. Spine (Phila Pa 1976) 2015;40:E191-8. [Crossref] [PubMed]
- Blagg SE, Don AS, Robertson PA. Anatomic determination of optimal entry point and direction for C1 lateral mass screw placement. J Spinal Disord Tech 2009;22:233-9. [Crossref] [PubMed]
- Resnick DK, Benzel EC. C1-C2 pedicle screw fixation with rigid cantilever beam construct: case report and technical note. Neurosurgery 2002;50:426-8. [PubMed]
- Ma XY, Yin QS, Wu ZH, et al. Anatomic considerations for the pedicle screw placement in the first cervical vertebra. Spine (Phila Pa 1976) 2005;30:1519-23. [Crossref] [PubMed]
- Tan M, Wang H, Wang Y, et al. Morphometric evaluation of screw fixation in atlas via posterior arch and lateral mass. Spine (Phila Pa 1976) 2003;28:888-95. [Crossref] [PubMed]
- Lin JM, Hipp JA, Reitman CA. C1 lateral mass screw placement via the posterior arch: a technique comparison and anatomic analysis. Spine J 2013;13:1549-55. [Crossref] [PubMed]
- Kim JS, Eun SS, Prada N, et al. Modified transcorporeal anterior cervical microforaminotomy assisted by O-arm-based navigation: a technical case report. Eur Spine J 2011;20:S147-52. [Crossref] [PubMed]
- Austin MS, Vaccaro AR, Brislin B, et al. Image-guided spine surgery: a cadaver study comparing conventional open laminoforaminotomy and two image-guided techniques for pedicle screw placement in posterolateral fusion and nonfusion models. Spine (Phila Pa 1976) 2002;27:2503-8. [Crossref] [PubMed]
- Patton AG, Morris RP, Kuo YF, et al. Accuracy of fluoroscopy versus computer-assisted navigation for the placement of anterior cervical pedicle screws. Spine (Phila Pa 1976) 2015;40:E404-10. [Crossref] [PubMed]
- Smith HE, Welsch MD, Sasso RC, et al. Comparison of radiation exposure in lumbar pedicle screw placement with fluoroscopy vs computer-assisted image guidance with intraoperative three-dimensional imaging. J Spinal Cord Med 2008;31:532-7. [Crossref] [PubMed]
- Dusad T, Kundnani V, Dutta S, et al. Comparative Prospective Study Reporting Intraoperative Parameters, Pedicle Screw Perforation, and Radiation Exposure in Navigation-Guided versus Non-navigated Fluoroscopy-Assisted Minimal Invasive Transforaminal Lumbar Interbody Fusion. Asian Spine J 2018;12:309-16. [Crossref] [PubMed]
- Bratschitsch G, Leitner L, Stucklschweiger G, et al. Radiation Exposure of Patient and Operating Room Personnel by Fluoroscopy and Navigation during Spinal Surgery. Sci Rep 2019;9:17652. [Crossref] [PubMed]
- Tajsic T, Patel K, Farmer R, et al. Spinal navigation for minimally invasive thoracic and lumbosacral spine fixation: implications for radiation exposure, operative time, and accuracy of pedicle screw placement. Eur Spine J 2018;27:1918-24. [Crossref] [PubMed]
- Kleck CJ, Johnson C, Akiyama M, et al. One-step Minimally Invasive Pedicle Screw Instrumentation Using O-Arm and Stealth Navigation. Clin Spine Surg 2018;31:197-202. [Crossref] [PubMed]
- Chachan S, Bin Abd Razak HR, Loo WL, et al. Cervical pedicle screw instrumentation is more reliable with O-arm-based 3D navigation: analysis of cervical pedicle screw placement accuracy with O-arm-based 3D navigation. Eur Spine J 2018;27:2729-36. [Crossref] [PubMed]



