Peyronie’s disease: a literature review on epidemiology, genetics, pathophysiology, diagnosis and work-up
Introduction
Peyronie’s disease (PD) can have devastating psychological and physical consequences on patients (1). The condition is also often associated with erectile dysfunction (ED) and, therefore, can also impact the psychological well-being of the sexual partner. PD is a wound-healing disorder of which is manifested by a fibrous inelastic scar at tunica albuginea, observable with a flaccid penis. Such scarring can cause the penis to abnormally curve, narrow, and shorten, leading to painful erection and difficulty in coitus. Numerous treatment modalities have been practiced and researched around the world by scholars, but unfortunately, the treatments do not provide a cure. To date, PD remains a therapeutic dilemma for the healthcare community (2).
This literature review outlines the prevalence, genetics, pathophysiology, diagnostic methods, and work-up of PD. Recent advances in the comprehension of PD have been included; research information, which provided no significant outcomes, has been omitted from this review.
The main objective for this review is to provide a practical approach to the understanding of PD, which may lead to significant positive treatment outcomes.
To date, no cohort data has clearly characterized the incidence and/or prevalence of PD among the general population, thus epidemiologic data on PD are limited. Inconsistencies on epidemiological data on PD exist, as healthcare providers assume that most men feel embarrassed about reporting this condition (3,4). Of course, this shame prevents patients from seeking proper medical attention and getting positive outcomes when the symptoms are mild and properly manageable. Some physicians believe that the incidence of symptomatic PD may be increasing, which can explained by the increasing number of patients seeking treatment and evaluation for ED in outpatient clinics (5). A survey conducted by Sullivan et al. [2015] showed that a significant proportion of urologists (26%) considered PD rates to be less than 1%, while only 5% of urologists believed rates were higher than 10%. With this many surveyed urologists under the impression that PD is a rare clinical entity, there is clearly a lack of knowledge that likely contributes to under diagnosis in the medical community (6).
Epidemiology and etiology
Controversy exists regarding the presentation age of PD. Although PD is thought to be a disease that primarily afflicts older men, research suggests that PD occurs in younger men, and may warrant more aggressive therapy (7).
It is estimated that the condition is present in around 0.3% to 13.1% men around the world. The prevalence may increase further in certain sub-populations. For example, the prevalence of PD in men operated for radical prostatectomy is up to 16% (Table 1) (8).
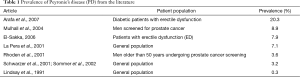
Full table
To date, Schwarzer et al. performed the biggest prevalence study for PD [2001], in which 8,000 men were sought for the questionnaire-based study, and a total of 4,432 (55.4%) responded. The results showed that 3.2% subjects had newly developed palpable plaque. The prevalence for age groups 30–39, 40–49, 50–59, and 60–69 years was 1.5%, 3%, 3%, and 4% respectively. The maximum prevalence (6.5%) was in men older than 70 years (9).
Sexual dysfunction among young men in their second decade of life is commonly under investigated and under treated. Literature on sexual dysfunction in young men is scarce. A single publication focused on penile hemodynamic testing in teenagers with ED, but did not look at PD or other sexual dysfunction in teenagers. Although PD has been studied and described in older men, it cannot be assumed to be similar in teenagers, as their sexual activity patterns may differ considerably. PD and its associated ED are projected to have huge psychological impact in teenagers with PD as they reach sexual maturity and begin sexual activity (10).
Comorbid factors such as diabetes, hypertension, and hyperlipidaemia impair vascular and neural pathways, and are commonly reported as risk factors for PD (11,12). Diabetes was detected in 40% of Peyronie’s patients presenting with ED only, which was significantly higher than other Peyronie’s patients (13).
The exact etiology of PD is not clearly understood, and out of numerous theories proposed, penile trauma is postulated to be a major causative factor. Penile trauma might be caused by acute and severe conditions like accidents or surgical procedure, or it may be due to repetitive microtrauma during coitus. Although all men are exposed to some level of penile trauma during sex, very few of them develop PD due to microtrauma. This indicates that other factors, e.g., genetics, may also contribute to the development of PD. Some potent risk factors for PD are a history of nongonococcal urethritis, smoking, inflammatory genital disease in a partner, fibromatous lesions of the genital track, and history of genital tract surgery (14).
Controversies still exists in regards to the hormonal factor as a cause of PD. Over the years, studies have suggested that hypogonadism is related to PD. Moreno et al. [2009], in their study of 121 PD, patients found that low testosterone levels (<300 ng/dL) are found in almost 74.4% PD patients. The study also suggested that hypogonadal men have more penile curvature as compared to eugonadal PD patients (15). However, a study by Kirby et al. [2015] found that although hypogonadism is prevalent in PD patients, low testosterone levels may not be associated with higher penile curvature in all the patients (16).
In another case-controlled study, Bjekic et al. [2006] evaluated the risk factors associated with PD. A total of 82 men with well-defined PD were compared with 264 men who had never had ED, nor any signs of PD. The study identified risk factors associated with PD [which is a genetic predisposition of Dupuytren’s contracture: minor vascular penile trauma either due to accident or surgery of genital track or prostatectomy; systemic vascular diseases like diabetes mellitus, hypertension, and hyperlipidemia; smoking; and alcohol abuse. Long-term use of beta-blockers, especially propranolol, and a history of non-gonococcal urethritis were also found to be prevalent in patients with PD (17). It has been suggested that an early age (40–50 years old) presentation of the disease and the presence of hypertension, diabetes mellitus, and dyslipidaemia pose a greater risk for early disease progression (11).
The natural history of PD is variable among different patients. The progression of the condition may take place over several years. PD has been observed as a self-limiting condition in earlier research and it has been found that most of the cases resolve spontaneously. Earlier studies suggest that penile angulation becomes stable once it is calcified. However, recent studies found that PD plaque is completely resolved without treatment in only 13% of cases while 40% patients feel that their condition is in progressive stage. The remaining men (47%) reported no change in their condition. From these studies, healthcare professionals suggest that the condition must be evaluated and treated as soon as the patient complains of significant coital failure, as observations suggest that the treatment is more promising with early detection (18).
Genetics
Although the current understanding of the genetic factors associated with PD is limited, significant advances have been made in the past three decades.
Different hypotheses about genetic etiology for PD have been proposed: (I) familial aggregation and genetic transmission mode via HLA-B7 cross-reacting group; (II) chromosomal abnormalities like duplication of chromosome 7 and 8 and deletion of chromosome Y; (III) single nucleotide polymorphism leading to elevated levels of transforming growth factor-β1 (TGF-β1); (IV) over expression of gene pleiotrophin (PTN/OSF-1) and monocyte chemotactic precursor protein-1 (MCP-1) gene; and (V) epigenetic regulation by histone deacetylases (HDACs). Among all these theories, the familial aggregation and genetic transmission mode via HLA-B7 cross-reacting group theory is widely accepted and understood (19).
Genetic predisposition has been suggested as a causal factor, because of the familial clustering of the condition and studies assessing mutation of human leukocyte antigen (HLA-B7), PD is strongly associated with both Dupuytren’s contracture and human leukocyte antigen B27-B7 (20,21). Another investigation on HLA class II antigens has shown the association of HLA-DR3 and HLA-DQw2 with PD. The antigen HLA-DR3 was detected in 33.3% patients and HLA-DQw2 was found in 58.8% of patients. Both HLA-DR3 and HLA-DRw2 are typically associated with organospecific autoimmune disorders, suggesting possible auto-immunological factors in PD (22).
Bias et al. [1982], through pedigree analysis of three families affected by PD and Dupuytren’s contracture, showed that the condition has an autosomal dominant mode of inheritance with incomplete penetrance (23). Controversially, other studies showed that familial segregation patterns suggest an independent assortment of HLA loci, decreasing the likelihood that these loci contribute to the development of PD (24).
Other authors detected karyotypic abnormalities in PD plaque-derived fibroblasts. Chromosomal abnormalities detected included three numerical changes, duplication of chromosomes 7 and 8 and deletion of chromosome Y (25,26).
The most common chromosomal abnormalities detected were aneuploidy of chromosomes 7 and 8, followed by chromosomes 17 and 18, and then the Y and X chromosomes (27).
Heritable single nucleotide polymorphisms (SNPs) affecting gene expression has been associated with an elevated levels of TGF-β1. However, the mechanism for the elevation has not been elucidated (19).
Genes related to myogenic conversion during wound healing and fibroblast differentiation into myofibroblasts was up-regulated. The gene with highest level of expression in PD plaque was pleiotrophin (PTN/OSF-1), a secreted heparin-binding protein or growth factor that induces fibroblast proliferation and osteoblast recruitment and osteogenesis. The monocyte chemotactic precursor protein 1 (MCP-1) gene drives the inflammatory cascade and promotes ossification has been found to be upregulated. Higher levels of MCP-1 mRNA have been observed in PD plaque-derived fibroblasts compared with fibroblasts derived from normal tunica albuginea (28). Qian et al. [2004] compared expression profiles of PD patients with those of Dupuytren’s contracture patients. A series of 15 genes were upregulated and none were downregulated in the PD plaque versus the normal TA. The upregulated genes were involved in collagen degradation: matrix metalloproteinase (MMP), with MMP2 and MMP9, and thymosins (MMP activators). MMP-2 or MMP-9 was expressed in one half of the PD plaques, in addition to genes involved in actin-cytoskeleton interactions required for fibroblasts and myofibroblast to generate the contractile forces (29). Findings of another study showed lower expression of apoptotic genes that may cause the persistence of collagen-producing cells that are upregulated, consequently resulting in plaque formation. Similar expression levels of apoptotic genes in both tunica albuginea and PD plaques may be caused by the generalized alterations in the tunica albuginea that lead to plaque formation at a vulnerable region subjected to recurrent trauma (30). Certain genes, such as the DNA-binding inhibitor Id-2, is a negative regulator of the myogenic program operative in myofibroblast differentiation, responsible for collagen synthesis and cellular contracture in fibrosis that are also expressed in PD plaques (31).
From the evidence, it can be assumed that in the PD tissue, the genes involved in collagen synthesis, myofibroblast differentiation, tissue remodeling, inflammation, ossification, and proteolysis are up-regulated, and the genes that inhibit some of these processes and collagenase are down-regulated.
Pathophysiology
Several theories for the pathogenesis of PD have been proposed, although the exact etiology remains unclear.
Anatomy based hypothesis
The anatomy of the vascular network around the tunica albuginea is unique. The arteries are on the exterior side and are protected by a cuff of loose areolar tissues, while the veins are in direct contact with the fibrous portion of tunica albuginea (21). The most widely accepted theory is trauma or microtrauma to the tunica albuginea during erection in genetically susceptible individuals. Repeated microvascular injury to the tunica albuginea causes inflammation, disruption of the elastic fibers and deposition of fibrin (32). Fibrinogen, a tissue protein responsible for the wound healing, is converted into fibrin by the action of thrombin, forming a temporary matrix for the support of endothelial cells response. Fibrin is a strong chemo-attractant, thus promoting the influx of inflammatory cells and mediators like macrophages, neutrophils, mast cells, cytokines, and fibroblasts (32,33). The influx of leukocytes and macrophages, as an inflammatory response, continues via arterial flow, resulting in production of a large amount of cytokines. Due to constrained venous outflow, cytokines cannot be dispersed or degraded, resulting in excessive production of collagen fiber and matrix, which leads to the destruction of delicate collagen network and elastic fiber (20,21). Antibodies to elastin are present in all individuals; however, Peyronie’s patients exhibit increased levels of anti-tropoelastin (reflecting elastin synthesis) and anti-α-elastin (reflecting elastin destruction), suggesting that an autoimmune mechanism may be involved in the pathogenesis of PD (34).
During the early phase, inflammation and edema irritate the nerve endings, leading to pain during and/or without an erection. The pain gradually subsides with the maturation of inflammation and death of nerve fibers. In the chronic phase of inflammation, erectile tissues are affected, leading to ED. The changes that occur during both theses phases are characterized by their clinical presentations; pain, plaque, and penile deformity during the initial phase, and plaque, penile deformity, and ED during chronic phase (21).
Ventral penile curvature has also been reported due to urethral manipulation. This is termed “Kelami syndrome” or urethral manipulation syndrome. Ultrasound evidence suggests that the underlying mechanism for penile curvature is one of periurethral scarring, perhaps secondary to inflammation from urethral manipulation (35).
In a mechanically stressed environment, and in the presence of various tissue growth factors and cytokines, myofibroblast cells demonstrated cytogenetic instability, excess production of fibrogenic cytokines, and other functional alterations. The continued exposure of these cells to tensile forces, and the underlying defective apoptotic mechanism, resulted in an inappropriate and persistent stimulation of the wound-healing process (36).
The above theories attempt to explain that PD is caused due to aberrant wound-healing process, in response to trauma within the layers of tunica albuginea.
Oxidative damage theory, autoimmunity theory, and gene theory
Fibrogenesis in many chronic hepatic, pulmonary, and neuronal degeneration diseases is caused due to oxidative stress. Free radicals generated due to oxidative stress leads to the generation of superoxide, peroxynitrite, and peroxide species, causing lipid peroxidation and tissue damage along with the enhanced activity of fibroblast and, thus, fibrogenesis. Excessive fibrous tissue generation is the main factor of PD. Therefore, the hypothesis of oxidative stress and related fibrogenesis can be applied to the pathophysiology of PD (37). Nitric oxide synthase is produced when smooth muscle cells and macrophages are stimulated. Up-regulation of nitric oxide synthase causes the generation of high levels of nitric oxide, a potent free radical leading to oxidative stress and poor vasorelaxation. It is thought that this process exists in PD (38). However, another study has shown the cavernous tissue of the penis in PD patients to have a diminished level of the enzyme nitric acid synthase (NOS). As this is required for normal penile erection, diminished concentration of this enzyme may be a cause of ED in PD (39).
Studies showed the presence of elastin antibodies like anti-tropoelastin (reflecting elastin synthesis) and anti-α-elastin (reflecting elastin destruction). Increased antibody production is another feature of autoimmunity in PD. One process of this autoimmune feature is a cell-mediated response to inflammation with excessive fibroblast activity and increased elastin production (40).
Researchers have noted that two general mechanisms aid the development of extracellular matrix in the case of PD: first, excavation of plasma protein like plasma fibronectin and fibrinogen and, second, synthesis of fibronectin variants by the wounded tissue. When hereditary trend for PD has been observed for a long time, the relation of HLA-B27 and HLA-B7 is still debatable (41).
Various observations suggested that increased expression of TGF-β1 and higher levels of pro-and anti-fibrotic gene products could be observed in PD. Also, there is an increase in the ratio of nitric oxide to reactive oxygen species (ROS) in the tunica albuginea of penis. All these factors have been found to be related to formation and progression of plaque in PD patients. Genes such as OSF-1 (osteoblast recruitment), MCP-1 (macrophage recruitment), and procollagenase IV (collagenase degradation) are responsible for the generation of this plaque and are thus considered regulatory genes for PD (42).
Molecular mechanisms: role of TGF-β
TGF-β1 is a soluble growth factor of the TGF-β superfamily, and binds to specific serine/threonine kinase receptors on cell surface, triggering the activation of Smad transcription factors. Inflammatory cells such as platelets, macrophages, and fibroblasts synthesize TGF-β1, which is an inactive latent peptide. On activation, TGF-β binds to specific cell surface receptor inducing a signal transduction cascade. A complicated signaling network of Smad transcription factors regulates the profibrotic effects of TGF-β. The network is involved in cellular proliferation, and/or differentiation, which is an essential system in the pathogenesis of fibrotic disorder. Such cascade leads to increased synthesis of connective tissue and inhibition of collagenase enzyme. It is noteworthy that TGF-β is also capable of inducing own synthesis, as well as specific receptors. Such auto-upregulation, leads to a continuous cycle of connective tissue and abnormal fibrotic changes, thus leading to plaque formation (43). Myostatin is a member of TGF-β family also known as GDF-8. Mysostatin is expressed in myofibroblasts, the cell that has a major role in fibrosis by triggering the proliferation of myofibroblasts, presumable from differentiation of fibroblast cells within the PD plaque.
The protein induces new plaques and also condenses the plaque already formed by TGF-β. Overexpression of myostatin has been found in the majority of the PD plaques. It has also been found that synthesis and release of pro-fibrotic factors like plasminogen activator inhibitor-2 and ROS, along with TGF-β, aggravate the plaque as it enters its chronic stage. This leads to a formation of dense fibrotic plaque, which also gets calcified and ossified. Osteoblasts can also be found in chronic plaques (21,44).
This evidence suggests that PD plaques and other related symptoms are developed due to various conditions, and there is no exact and clear pathophysiology. Researchers continue to explore new physiological pathways related to the development of PD.
Diagnosis and work-up
A diagnosis of PD may be made on the basis of history, clinical examination, lab testing is not necessary and that imaging is only needed if an intervention is planned.
The patients with PD can present with combination of following conditions:
- Pain in penis during erections;
- The curvature of the penis. The angulation can be noted during erection in some patients while, in some cases, palpable plaque can be noticed at the site of angulation even in a flaccid penis;
- An hourglass deformity caused at the site of the plaque due to the indentation in the penile shaft;
- Reduced erectile function due to loss of rigidity;
- Problems with intercourse due to penile buckling caused by the angulation.
The curvature of the penis can reach an angle of 90° or more and makes the treatment difficult.
Usually, the penile pain resolves without any therapy. Some patients also observe a reduction in pain or resolution before the appearance of plaque or angulation. While such change was considered as a self-resolving feature of PD in an earlier time; present research suggests that resolution in pain is due to the chronic stage of PD where the nerve fibers innervating the organ die due to extended fibrosis (45).
PD can be classified into two phases, acute (active) and chronic (stable). The acute phase (active) of the condition is characterized by penile pain, minor curvature, and a nodule in the penis and onset of the pain may be associated with history of penile trauma during intercourse, the patient will be in distress due to this pain (46). These features indicate changing inflammatory pattern and the phase lasts for around 18–24 months. Chronic phase (stable) of PD is characterized by a stable palpable plaque with a deformity that is no longer progressive. Decreased erectile function may be also present.
The most common location for plaque in PD is the dorsal midline resulting in an upward bend of the erect penis. The next most common site is a dorsal midline with septal extension. The plaque may also extend from the dorsal midline circumferentially around the corporeal bodies. Plaque between the corpus spongiosum and the ventral surface of the corpora cavernosa is rarely seen (47).
Emotional and psychological disturbances, although not a physical feature of PD, are often observed in males with ED related to PD and warrant appropriate counseling (48).
In addition to information about sexual history, history of diabetes, hypertension, elevated cholesterol, and smoking, as well as any evidence for vascular risk factors for ED, should be taken into consideration.
The recently validated PD questionnaire (PDQ) addresses not only the concerns of the patient regarding structural changes of the penis, but also how PD affects his overall psychological condition (1,49).
Assessment of the erect penis through photographs taken at home is not useful clinically because of the inability to adequately represent and measure a three-dimensional deformity (50,51).
Physical examination
The diagnosis of PD is clinically determined by the patient's history and penile examination. The physical examination should include a general assessment of the femoral pulses, and the hands and feet for detecting possible DD or Ledderhose scarring of the plantar fascia (52). Appearance of the flaccid penis, and whether it is circumcised, and measurement of stretch penile length, rigidity, girth, and curvature during erection (53,54). Assessment of erectile tissue health can be done by stretching the penile shaft. PD patients with significant corporal fibrosis, such as the one with concurrent chronic diabetes lose the stretchability of the penile shaft. On the other hand, ability to stretch the penis is usually normal in young patients with psychogenic or mild arteriogenic ED, but this needs differentiation for the diagnosis of PD.
The degree of curvature can range from nearly straight (15°), to 180° in the most severe cases. Plaques can be single or multiple and are associated with a variety of penile deformities. Usually the simplest approach to diagnosis the plaque is palpation (55-58), since 82% of plaques have an extension of more than 1.5 cm in diameter. Its exact size can be determined following a measurement with caliper or ruler (56). Although the most common direction of curvature is dorsal, ventral, lateral, and complex curvatures are also frequently seen. Deformities range from ‘notching’ to circumferential ‘hourglass’ defects. Patients are normally concerned with penile shortening, which is a common symptom (59).
Laboratory investigation
No specific blood tests are available for diagnosis of PD. While the association between the condition and overexpression of HLA-B7 antigen, TGF-β1, anti DNA, antinuclear and antielastin antibodies has been found, they cannot be considered as specific markers for the disease. Also, laboratory investigation alone of HLA-B7 is not practical, as the condition needs thorough physical examination and history taking (60,61).
Imaging studies
Imaging of penile shaft is important in the diagnosis of PD in order to note calcification of the plaque as it signifies the end point of chronic PD after which no further angulation occurs. Imaging for the diagnosis of PD is done in multiple ways as follow:
- A simple radiograph using X-ray can identify calcification/plaque in the soft tissue (62,63);
- High-resolution ultrasound of penis helps in defining the extent of the plaque. The characteristic echogenic shadowing found in a USG image helps to pinpoint calcification in the plaque. Sonographer detection rates range from 39% to 95% (58,64-68). Ultrasound is the method of choice to demonstrate plaque calcifications. A calcification grading system was published and introduced recently. Patients with grade 3, or the most extensive, calcification (>1.5 cm in any dimension or multiple plaques ≥1.0 cm) were more likely to undergo surgery when they also had satisfactory erectile function. This is in contradiction to those who had less severe calcification of grade 1 (<0.3 mm) or grade 2 (0.3 to 1.5 cm) or no calcification in whom there was no evidence of an increased likelihood of proceeding to surgery (69);
- Computerized tomography can be used to visualize non-calcified plaques (10);
- Corpus cavernosograpy can also be used to define the plaque as well as any compression of the cavernosal space. However, this test is usually not applied because of its cost, and is reserved for special cases, particularly before plaque surgery due to its invasiveness (19);
- MRI is an effective, non-invasive way to identify the plaque in its early stages, when there are only fibrous tissues present, as well as penile morphology and pathology. However, this test is usually not applied because of its cost, but can be helpful in certain questionable cases (70);
- Ultrasonography with intracavernous injection of vasoactive substance like alprostadil, and/or dynamic infusion cavernosometry and cavernosography can be applied for the PD patients with ED in order to identify underlying arteriogenic ED or corporal venoocclusive dysfunction (71). Cavernous artery peak systolic velocity (PSV) when <25 cm/s is suggested of cavernous arterial insufficiency, PSV consistently >35 cm/s define normal cavernous arterial flow. Cavernous artery end diastolic velocity (EDV) when >5 cm/s is suggested for veno-occlusive dysfunction. Resistive index (RI) when >0.9 has been associated with normal penile vascular function and <0.75 is consistent with veno-occlusive dysfunction also it visualizes penile tissues and detects areas of calcification (54).
Conclusions
The prevalence of PD is much greater than previously thought; the development of extensive screening would offer a means of evaluating associated comorbidities, and would provide a better understanding of the risk factors.
While multiple theories have been proposed for the pathophysiology of PD, further understanding of the intricate physiology of PD and genetic predisposition is required. Though trauma is a major factor causing PD, it is unlikely that it is solely responsible for it. The mechanisms leading to excessive scarring and fibrosis are still debatable.
Clinical examination as palpation and history is still the standard for initial diagnosis of PD. Ultrasound is invasive, cost-effective a repeatable method that can reveal plaques in more than 50% of cases and detects calcification in 100% cases. MRI can reveal more plaques, but does not differentiate between calcified and non-calcified plaques.
Appropriate treatment should be individualized as per patient’s goals and expectations, disease history, physical examination findings, and erectile function.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Hellstrom WJ, Feldman R, Rosen RC, et al. Bother and distress associated with Peyronie's disease: validation of the Peyronie's disease questionnaire. J Urol 2013;190:627-34. [Crossref] [PubMed]
- Levine LA. Peyronie's disease and erectile dysfunction: Current understanding and future direction. Indian J Urol 2006;22:246-50. [Crossref]
- Arafa M, Eid H, El-Badry A, et al. The prevalence of Peyronie's disease in diabetic patients with erectile dysfunction. Int J Impot Res 2007;19:213-7. [Crossref] [PubMed]
- Lindsay MB, Schain DM, Grambsch P, et al. The incidence of Peyronie's disease in Rochester, Minnesota, 1950 through 1984. J Urol 1991;146:1007-9. [PubMed]
- Hellstrom WJ. History, epidemiology, and clinical presentation of Peyronie's disease. Int J Impot Res 2003;15 Suppl 5:S91-2. [Crossref] [PubMed]
- Sullivan J, Moskovic D, Nelson C, et al. Peyronie's disease: urologist's knowledge base and practice patterns. Andrology 2015;3:260-4. [Crossref] [PubMed]
- Taylor FL, Levine LA. Peyronie's Disease. Urol Clin North Am 2007;34:517-34. vi. [Crossref] [PubMed]
- Dibenedetti DB, Nguyen D, Zografos L, et al. A Population-Based Study of Peyronie's Disease: Prevalence and Treatment Patterns in the United States. Adv Urol 2011;2011:282503.
- Schwarzer U, Sommer F, Klotz T, et al. The prevalence of Peyronie's disease: results of a large survey. BJU Int 2001;88:727-30. [Crossref] [PubMed]
- Tal R, Hall MS, Alex B, et al. Peyronie's disease in teenagers. J Sex Med 2012;9:302-8. [Crossref] [PubMed]
- Kadioglu A, Tefekli A, Erol B, et al. A retrospective review of 307 men with Peyronie's disease. J Urol 2002;168:1075-9. [Crossref] [PubMed]
- Rhoden EL, Riedner CE, Fuchs SC, et al. A cross-sectional study for the analysis of clinical, sexual and laboratory conditions associated to Peyronie's disease. J Sex Med 2010;7:1529-37. [Crossref] [PubMed]
- Kadioglu A, Oktar T, Kandirali E, et al. Incidentally diagnosed Peyronie's disease in men presenting with erectile dysfunction. Int J Impot Res 2004;16:540-3. [Crossref] [PubMed]
- Bilgutay AN, Pastuszak AW. Peyronie's disease: What's around the bend? Indian J Urol 2016;32:6-14. [Crossref] [PubMed]
- Moreno SA, Morgentaler A. Testosterone deficiency and Peyronie's disease: pilot data suggesting a significant relationship. J Sex Med 2009;6:1729-35. [Crossref] [PubMed]
- Kirby EW, Verges D, Matthews J, et al. Low testosterone has a similar prevalence among men with sexual dysfunction due to either Peyronie's disease or erectile dysfunction and does not correlate with Peyronie's disease severity. J Sex Med 2015;12:690-6. [Crossref] [PubMed]
- Bjekic MD, Vlajinac HD, Sipetic SB, et al. Risk factors for Peyronie's disease: a case-control study. BJU Int 2006;97:570-4. [Crossref] [PubMed]
- Shenoy-Bhangle A, Perez-Johnston R, Singh A. Penile imaging. Radiol Clin North Am 2012;50:1167-81. [Crossref] [PubMed]
- Herati AS, Pastuszak AW. The Genetic Basis of Peyronie's Disease: A Review. Sex Med Rev 2016;4:85-94. [Crossref] [PubMed]
- Mulhall JP. Expanding the paradigm for plaque development in Peyronie's disease. Int J Impot Res. 2003;15 Suppl 5:S93-102. [Crossref] [PubMed]
- El-Sakka AI, Salabas E, Dinçer M, et al. The pathophysiology of Peyronie's disease. Arab J Urol 2013;11:272-7. [Crossref] [PubMed]
- Rompel R, Mueller-Eckhardt G, Schroeder-Printzen I, et al. HLA antigens in Peyronie's disease. Urol Int 1994;52:34-7. [Crossref] [PubMed]
- Bias WB, Nyberg LM Jr, Hochberg MC, et al. Peyronie's disease: a newly recognized autosomal-dominant trait. Am J Med Genet 1982;12:227-35. [Crossref] [PubMed]
- Leffell MS, Devine CJ Jr, Horton CE, et al. Non-association of Peyronie's disease with HLA B7 cross-reactive antigens. J Urol 1982;127:1223-4. [PubMed]
- Somers KD, Winters BA, Dawson DM, et al. Chromosome abnormalities in Peyronie's disease. J Urol 1987;137:672-5. [PubMed]
- Guerneri S, Stioui S, Mantovani F, et al. Multiple clonal chromosome abnormalities in Peyronie's disease. Cancer Genet Cytogenet 1991;52:181-5. [Crossref] [PubMed]
- Mulhall JP, Nicholson B, Pierpaoli S, et al. Chromosomal instability is demonstrated by fibroblasts derived from the tunica of men with Peyronie's disease. Int J Impot Res 2004;16:288-93. [Crossref] [PubMed]
- Szardening-Kirchner C, Konrad L, Hauck EW, et al. Upregulation of mRNA expression of MCP-1 by TGF-beta1 in fibroblast cells from Peyronie's disease. World J Urol 2009;27:123-30. [Crossref] [PubMed]
- Qian A, Meals RA, Rajfer J, et al. Comparison of gene expression profiles between Peyronie's disease and Dupuytren's contracture. Urology 2004;64:399-404. [Crossref] [PubMed]
- Zorba OU, Sirma S, Ozgon G, et al. Comparison of apoptotic gene expression profiles between Peyronie's disease plaque and tunica albuginea. Adv Clin Exp Med 2012;21:607-14. [PubMed]
- Powell DW, Mifflin RC, Valentich JD, et al. Myofibroblasts. I. Paracrine cells important in health and disease. Am J Physiol 1999;277:C1-9. [Crossref] [PubMed]
- Devine CJ Jr, Somers KD, Jordan SG, et al. Proposal: trauma as the cause of the Peyronie's lesion. J Urol 1997;157:285-90. [Crossref] [PubMed]
- Diegelmann RF. Cellular and biochemical aspects of normal and abnormal wound healing: an overview. J Urol 1997;157:298-302. [Crossref] [PubMed]
- Stewart S, Malto M, Sandberg L, et al. Increased serum levels of anti-elastin antibodies in patients with Peyronie's disease. J Urol 1994;152:105-6. [PubMed]
- Merkle W. Cause of deviation of the erectile penis after urethral manipulations (Kelami syndrome)--demonstration of ultrasound findings and case reports. Urol Int 1990;45:183-5. [Crossref] [PubMed]
- Chung E, De Young L, Brock GB. Rat as an animal model for Peyronie's disease research: a review of current methods and the peer-reviewed literature. Int J Impot Res 2011;23:235-41. [Crossref] [PubMed]
- Moro T, Nakao S, Sumiyoshi H, et al. A Combination of Mitochondrial Oxidative Stress and Excess Fat/Calorie Intake Accelerates Steatohepatitis by Enhancing Hepatic CC Chemokine Production in Mice. PLoS One 2016;11:e0146592. [Crossref] [PubMed]
- Bivalacqua TJ, Champion HC, Leungwattanakij S, et al. Evaluation of nitric oxide synthase and arginase in the induction of a Peyronie's-like condition in the rat. J Androl 2001;22:497-506. [PubMed]
- Matkov G, Levine LA, Storm DW. Peyronie's disease affecting the younger male. Program and abstracts from the American Urological Association 95th Annual meeting; April 29-May 4, 2000; Atlanta, Georgia, USA, 2000:abstr 743.
- Paulis G, Barletta D, Turchi P, et al. Efficacy and safety evaluation of pentoxifylline associated with other antioxidants in medical treatment of Peyronie's disease: a case-control study. Res Rep Urol 2015;8:1-10. [Crossref] [PubMed]
- Dolmans GH, Werker PM, de Jong IJ, et al. WNT2 locus is involved in genetic susceptibility of Peyronie's disease. J Sex Med 2012;9:1430-4. [Crossref] [PubMed]
- Ralph D, Gonzalez-Cadavid N, Mirone V, et al. The management of Peyronie's disease: evidence-based 2010 guidelines. J Sex Med 2010;7:2359-74. [Crossref] [PubMed]
- Balza E, Borsi L, Allemanni G, et al. Transforming growth factor beta regulates the levels of different fibronectin isoforms in normal human cultured fibroblasts. FEBS Lett 1988;228:42-4. [Crossref] [PubMed]
- Cantini LP, Ferrini MG, Vernet D, et al. Profibrotic role of myostatin in Peyronie's disease. J Sex Med 2008;5:1607-22. [Crossref] [PubMed]
- Gelbard M, Goldstein I, Hellstrom WJ, et al. Clinical efficacy, safety and tolerability of collagenase clostridium histolyticum for the treatment of peyronie disease in 2 large double-blind, randomized, placebo controlled phase 3 studies. J Urol 2013;190:199-207. [Crossref] [PubMed]
- Levine LA, Greenfield JM. Establishing a standardized evaluation of the man with Peyronie's disease. Int J Impot Res 2003;15 Suppl 5:S103-12. [Crossref] [PubMed]
- Tunuguntla HS. Management of Peyronie's disease--a review. World J Urol 2001;19:244-50. [Crossref] [PubMed]
- Gontero P, Di Marco M, Giubilei G, et al. Use of penile extender device in the treatment of penile curvature as a result of Peyronie's disease. Results of a phase II prospective study. J Sex Med 2009;6:558-66. [Crossref] [PubMed]
- Rosen R, Catania J, Lue T, et al. Impact of Peyronie's disease on sexual and psychosocial functioning: qualitative findings in patients and controls. J Sex Med 2008;5:1977-84. [Crossref] [PubMed]
- Ohebshalom M, Mulhall J, Guhring P, et al. Measurement of penile curvature in Peyronie's disease patients: comparison of three methods. J Sex Med 2007;4:199-203. [Crossref] [PubMed]
- Bacal V, Rumohr J, Sturm R, et al. Correlation of degree of penile curvature between patient estimates and objective measures among men with Peyronie's disease. J Sex Med 2009;6:862-5. [Crossref] [PubMed]
- Mulhall JP, Schiff J, Guhring P. An analysis of the natural history of Peyronie's disease. J Urol 2006;175:2115-8; discussion 2118. [Crossref] [PubMed]
- Wessells H, Lue TF, McAninch JW. Penile length in the flaccid and erect states: guidelines for penile augmentation. J Urol 1996;156:995-7. [Crossref] [PubMed]
- Bekos A, Arvaniti M, Hatzimouratidis K, et al. The natural history of Peyronie's disease: an ultrasonography-based study. Eur Urol 2008;53:644-50. [Crossref] [PubMed]
- Hauck EW, Weidner W. François de la Peyronie and the disease named after him. Lancet 2001;357:2049-51. [Crossref] [PubMed]
- Weidner W, Schroeder-Printzen I, Weiske WH, et al. Sexual dysfunction in Peyronie's disease: an analysis of 222 patients without previous local plaque therapy. J Urol 1997;157:325-8. [Crossref] [PubMed]
- Hauck EW, Heitz M, Schreiter F, et al. Induratio penis plastica. Peyronie's disease. Akt Urol 1999;30:386-404.
- Vosshenrich R, Schroeder-Printzen I, Weidner W, et al. Value of magnetic resonance imaging in patients with penile induration (Peyronie's disease). J Urol 1995;153:1122-5. [Crossref] [PubMed]
- Smith JF, Walsh TJ, Lue TF. Peyronie's disease: a critical appraisal of current diagnosis and treatment. Int J Impot Res 2008;20:445-59. [Crossref] [PubMed]
- Tal R, Heck M, Teloken P, et al. Peyronie's disease following radical prostatectomy: incidence and predictors. J Sex Med 2010;7:1254-61. [Crossref] [PubMed]
- Tsafrakidis P, Blake C, Pearcy R, et al. Peyronie's disease. Trends Urology, Gynecol Sexual Health 2009;14:17-21.
- Andresen R, Wegner HE, Miller K, et al. Imaging modalities in Peyronie's disease. An intrapersonal comparison of ultrasound sonography, X-ray in mammography technique, computerized tomography, and nuclear magnetic resonance in 20 patients. Eur Urol 1998;34:128-34; discussion 135. [Crossref] [PubMed]
- Gelbard MK. Dystrophic penile calcification in Peyronie's disease. J Urol 1988;139:738-40. [PubMed]
- Helweg G, Judmaier W, Wicke K, et al. Ultrasound and MRI in the diagnosis of penile induration (Peyronie's disease). Eur Radiol 1992;2:230-2. [Crossref]
- Balconi G, Angeli E, Nessi R, et al. Ultrasonographic evaluation of Peyronie's disease. Urol Radiol 1988;10:85-8. [Crossref] [PubMed]
- Lopez JA, Jarow JP. Duplex ultrasound findings in men with Peyronie's disease. Urol Radiol 1991;12:199-202. [Crossref] [PubMed]
- Schouman-Claeys E. Valeur et place de l’imagerie de la maladie de La Peyronie. Andrologie 1998;8:148-56. [Crossref]
- Nicolai M, Carriero A, De Thomasis R, et al. Dynamic magnetic resonance imaging versus dynamic echography in the staging of Peyronie's disease. Arch Ital Urol Androl 1996;68:97-100. [PubMed]
- Levine LA, Larsen SM. Surgery for Peyronie's disease. Asian J Androl 2013;15:27-34. [Crossref] [PubMed]
- Nam HJ, Park HJ, Park NC. Does testosterone deficiency exaggerate the clinical symptoms of Peyronie's disease? Int J Urol 2011;18:796-800. [Crossref] [PubMed]
- Coyne KS, Currie BM, Thompson CL, et al. The test-retest reliability of the Peyronie's disease questionnaire. J Sex Med 2015;12:543-8. [Crossref] [PubMed]


