Abstract
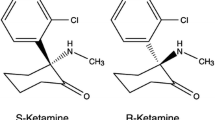
Ropivacaine is a long-acting amide-type local anaesthetic, released for clinical use in 1996. In comparison with bupivacaine, ropivacaine is equally effective for subcutaneous infiltration, epidural and peripheral nerve block for surgery, obstetric procedures and postoperative analgesia. Nevertheless, ropivacaine differs from bupivacaine in several aspects: firstly, it is marketed as a pure S(−)-enantiomer and not as a racemate, and secondly, its lipid solubility is markedly lower. These features have been suggested to significantly improve the safety profile of ropivacaine, and indeed, numerous studies have shown that ropivacaine has less cardiovascular and CNS toxicity than racemic bupivacaine in healthy volunteers.
Extensive clinical data have demonstrated that epidural 0.2% ropivacaine is nearly identical to 0.2% bupivacaine with regard to onset, quality and duration of sensory blockade for initiation and maintenance of labour analgesia. Ropivacaine also provides effective pain relief after abdominal or orthopaedic surgery, especially when given in conjunction with opioids or other adjuvants. Nevertheless, epidurally administered ropivacaine causes significantly less motor blockade at low concentrations. Whether the greater degree of blockade of nerve fibres involved in pain transmission (Aδ− and C-fibres) than of those controlling motor function (Aα− and Aβ-fibres) is due to a lower relative potency compared with bupivacaine or whether other physicochemical properties or stereoselectivity are involved, is still a matter of intense debate.
Recommended epidural doses for postoperative or labour pain are 20–40mg as bolus with 20–30mg as top-up dose, with an interval of ≥30 minutes. Alternatively, 0.2% ropivacaine can be given as continuous epidural infusion at a rate of 6–14 mL/h (lumbar route) or 4–10 mL/h (thoracic route).
Preoperative or postoperative subcutaneous wound infiltration, during cholecystectomy or inguinal hernia repair, with ropivacaine 100–175mg has been shown to be more effective than placebo and as effective as bupivacaine in reducing wound pain, whereby the vasoconstrictive potency of ropivacaine may be involved. Similar results were found in peripheral blockades on upper and lower limbs. Ropivacaine shows an identical efficacy and potency to that of bupivacaine, with similar analgesic duration over hours using single shot or continuous catheter techniques.
In summary, ropivacaine, a newer long-acting local anaesthetic, has an efficacy generally similar to that of the same dose of bupivacaine with regard to postoperative pain relief, but causes less motor blockade and stronger vasoconstriction at low concentrations. Despite a significantly better safety profile of the pure S(−)-isomer of ropivacaine, the increased cost of ropivacaine may presently limit its clinical utility in postoperative pain therapy.
Similar content being viewed by others
References
Horlocker TT. Peripheral nerve blocks: regional anesthesia for the new millennium. Reg Anesth Pain Med 1998; 23: 237–40
Faccenda KA, Finucane BT. Complications of regional anaesthesia: incidence and prevention. Drug Saf 2001; 24: 413–42
Albright GA. Cardiac arrest following regional anesthesia with etidocaine or bupivacaine. Anesthesiology 1979; 51: 285–7
Zink W, Seif C, Bohl JRE, et al. The acute myotoxic effects of bupivacaine and ropivacaine after continuous peripheral nerve blockades. Anesth Analg 2003; 97: 1173–9
Vanhoutte F, Vereecke J, Verbeke N, et al. Stereoselective effects of the enantiomers of bupivacaine on the electrophysiological properties of the guinea-pig papillary muscle. Br J Pharmacol 1991; 103: 1275–81
Clarkson CW, Hondeghem LM. Mechanism for bupivacaine depression of cardiac conduction: fast block of sodium channels during the action potential with slow recovery from block during diastole. Anesthesiology 1985; 62: 396–405
Whiteside JB, Wildsmith JA. Developments in local anaesthetic drugs. Br J Anaesth 2001; 87: 27–35
Polley LS, Columb MO, Naughton NN, et al. Relative analgesic potencies of levobupivacaine and ropivacaine for epidural analgesia in labor [abstract]. Anesthesiology 2002; 96: A1052
Casati A, Leoni A, Aldegheri G, et al. A double-blind study of axillary brachial plexus block by 0.75% ropivacaine or 2% mepivacaine. Eur J Anaesthesiol 1998; 15: 549–52
Gristwood RW. Cardiac and CNS toxicity of levobupivacaine: strengths of evidence for advantage over bupivacaine. Drug Saf 2002; 25: 153–63
Groban L, Deal DD, Vernon JC, et al. Cardiac resuscitation after incremental overdosage with lidocaine, bupivacaine, levobupivacaine, and ropivacaine in anesthetized dogs. Anesth Analg 2001; 92: 37–43
Nancarrow C, Rutten A, Runciman W, et al. Myocardial and cerebral drug concentrations and the mechanisms of death after fatal intravenous doses of lidocaine, bupivacaine, and ropivacaine in the sheep. Anesth Analg 1989; 69: 276–83
Huang Y, Pryor M, Mather L, et al. Cardiovascular and central nervous system effects of intravenous levobupivacaine and bupivacaine in sheep. Anesth Analg 1998; 86: 797–804
Lee A, Fagan D, Lamont M, et al. Disposition kinetics of ropivacaine in humans. Anesth Analg 1989; 69: 736–8
Halldin MM, Bredberg E, Angelin B, et al. Metabolism and excretion of ropivacaine in humans. Drug Metab Dispos 1996; 24: 962–8
McCann ME, Sethna NF, Mazoit JX, et al. The pharmacokinetics of epidural ropivacaine in infants and young children. Anesth Analg 2001; 93: 893–7
Hansen TG, Ilett KF, Lim SI, et al. Pharmacokinetics and clinical efficacy of long-term epidural ropivacaine infusion in children. Br J Anaesth 2000; 85: 347–53
Ala-Kokko TI, Partanen A, Karinen J, et al. Pharmacokinetics of 0.2% ropivacaine and 0.2% bupivacaine following caudal blocks in children. Acta Anaesthesiol Scand 2000; 44: 1099–102
Karmakar MK, Aun CS, Wong EL, et al. Ropivacaine undergoes slower systemic absorption from the caudal epidural space in children than bupivacaine. Anesth Analg 2002; 94: 259–65
Habre W, Bergesio R, Johnson C, et al. Pharmacokinetics of ropivacaine following caudal analgesia in children. Paediatr Anaesth 2000; 10: 143–7
Akerman B, Hellberg IB, Trossvik C. Primary evaluation of the local anaesthetic properties of the amino amide agent ropivacaine (LEA 103). Acta Anaesthesiol Scand 1988; 32: 571–8
McGlade DP, Kalpokas MV, Mooney PH, et al. Comparison of 0.5% ropivacaine and 0.5% bupivacaine in lumbar epidural anaesthesia for lower limb orthopaedic surgery. Anaesth Intensive Care 1997; 25(3): 262–6
McGlade DP, Kalpokas MV, Mooney PH, et al. A comparison of 0.5% ropivacaine and 0.5% bupivacaine for axillary brachial plexus anaesthesia. Anaesth Intensive Care 1998; 26: 515–20
Eddleston JM, Holland JJ, Griffin RP, et al. A double-blind comparison of 0.25% ropivacaine and 0.25% bupivacaine for extradural analgesia in labour. Br J Anaesth 1996; 76: 66–77
Hickey R, Rowley CL, Candido KD, et al. A comparative study of 0.25% ropivacaine and 0.25% bupivacaine for brachial plexus block. Anesth Analg 1992; 75: 602–6
Kopacz DJ, Emanuelsson BM, Thompson GE, et al. Pharmacokinetics of ropivacaine and bupivacaine for bilateral intercostal blockade in healthy male volunteers. Anesthesiology 1994; 81: 1139–48
Ivani G, DeNegri P, Conio A, et al. Comparison of racemic bupivacaine, ropivacaine, and levo-bupivacaine for pediatric caudal anesthesia: effects on postoperative analgesia and motor block. Reg Anesth Pain Med 2002; 27: 157–61
Casati A, Borghi B, Fanelli G, et al. A double-blinded, randomized comparison of either 0.5% levobupivacaine or 0.5% ropivacaine for sciatic nerve block. Anesth Analg 2002; 94: 987–90
Hickey R, Hoffman J, Ramamurthy S. A comparison of ropivacaine 0.5% and bupivacaine 0.5% for brachial plexus block. Anesthesiology 1991; 74: 639–42
Da Conceicao MJ, Coelho L. Caudal anaesthesia with 0.375% ropivacaine or 0.375% bupivacaine in paediatric patients. Br J Anaesth 1998; 80: 507–8
Gautier P, De Kock M, Van Steenberge A, et al. A double-blind comparison of 0.125% ropivacaine with sufentanil and 0.125% bupivacaine with sufentanil for epidural labor analgesia. Anesthesiology 1999; 90: 772–8
Santorsola R, Casati A, Cerchierini E, et al. Levobupivacaine for peripheral blocks of the lower limb: a clinical comparison with bupivacaine and ropivacaine [in Italian]. Minerva Anestesiol 2001; 67(9 Suppl. 1): 33–6
Casati A, Fanelli G, Albertin A, et al. Interscalene brachial plexus anesthesia with either 0.5% ropivacaine or 0.5% bupivacaine. Minerva Anestesiol 2000; 66: 39–44
Uy HS, de Jesus AA, Paray AA, et al. Ropivacaine-lidocaine versus bupivacaine-lidocaine for retrobulbar anesthesia in cataract surgery. J Cataract Refract Surg 2002; 28: 1023–6
Brockway MS, Bannister J, McClure JH, et al. Comparison of extradural ropivacaine and bupivacaine. Br J Anaesth 1991; 66: 31–7
McDonald SB, Liu SS, Kopacz DJ, et al. Hyperbaric spinal ropivacaine: a comparison to bupivacaine in volunteers. Anesthesiology 1999; 90: 971–7
Polley LS, Columb MO, Naughton NN, et al. Relative analgesic potencies of ropivacaine and bupivacaine for epidural analgesia in labor: implications for therapeutic indexes. Anesthesiology 1999; 90: 944–50
Capogna G, Celleno D, Fusco P, et al. Relative potencies of bupivacaine and ropivacaine for analgesia in labour. Br J Anaesth 1999; 82: 371–3
Casati A, Fanelli G, Magistris L, et al. Minimum local anesthetic volume blocking the femoral nerve in 50% of cases: a double-blinded comparison between 0.5% ropivacaine and 0.5% bupivacaine. Anesth Analg 2001; 92: 205–8
Rosenberg PH, Heinonen E. Differential sensitivity of A and C nerve fibres to long-acting amide local anaesthetics. Br J Anaesth 1983; 55: 163–7
Bader AM, Datta S, Flanagan H, et al. Comparison of bupivacaine- and ropivacaine-induced conduction blockade in the isolated rabbit vagus nerve. Anesth Analg 1989; 68: 724–7
Wildsmith JA, Brown DT, Paul D, et al. Structure-activity relationships in differential nerve block at high and low frequency stimulation. Br J Anaesth 1989; 63: 444–52
McClure JH. Ropivacaine. Br J Anaesth 1996; 76: 300–7
Wildsmith JA. Relative potencies of ropivacaine and bupivacaine. Anesthesiology 2000; 92: 283–4
McCrae AF, Jozwiak H, McClure JH. Comparison of ropivacaine and bupivacaine in extradural analgesia for the relief of pain in labour. Br J Anaesth 1995; 74: 261–5
Erichsen CJ, Vibits H, Dahl JB, et al. Wound infiltration with ropivacaine and bupivacaine for pain after inguinal herniotomy. Acta Anaesthesiol Scand 1995; 39: 67–70
Capogna G, Celleno D, Laudano D, et al. Alkalinization of local anesthetics: which block, which local anesthetic? Reg Anesth 1995; 20: 369–77
Arthur GR, Wildsmith JAW, Tucker GT. Pharmacology of local anaesthetic drugs. In: Wildsmith JAW, Armitage EN, editors. Principles and practice of regional anesthesia. London: Churchill Livingstone, 1993: 29–45
Joshi GP, White PF. Management of acute and postoperative pain. Curr Opin Anaesth 2002; 14: 417–21
Joshi GP. Recent developments in regional anesthesia for ambulatory surgery. Curr Opin Anaesth 1999; 12: 643–7
Johr M. Postoperative pain management in infants and children: new developments. Curr Opin Anaesth 2000; 13: 285–9
Dahl JB, Moiniche S, Kehlet H. Wound infiltration with local anaesthetics for postoperative pain relief. Acta Anaesthesiol Scand 1994; 38: 7–14
Kopacz DJ, Carpenter RL, Mackey DC. Effect of ropivacaine on cutaneous capillary blood flow in pigs. Anesthesiology 1989; 71: 69–74
Nakamura K, Toda H, Kakuyama M, et al. Direct vascular effect of ropivacaine in femoral artery and vein of the dog. Acta Anaesthesiol Scand 1993; 37: 269–73
Cederholm I, Evers H, Lofstrom JB. Effect of intradermal injection of saline or a local anaesthetic agent on skin blood flow: a methodological study in man. Acta Anaesthesiol Scand 1991; 35: 208–15
Cederholm I, Akerman B, Evers H. Local analgesic and vascular effects of intradermal ropivacaine and bupivacaine in various concentrations with and without addition of adrenaline in man. Acta Anaesthesiol Scand 1994; 38: 322–7
Cederholm I, Evers H, Lofstrom JB. Skin blood flow after intradermal injection of ropivacaine in various concentrations with and without epinephrine evaluated by laser Doppler flowmetry. Reg Anesth 1992; 17: 322–8
Guinard J, Carpenter R, Owens B, et al. Comparison between ropivacaine and bupivacaine after subcutaneous injection in pigs: cutaneous blood flow and surgical bleeding. Reg Anesth 1991; 16: 268–71
Tetzlaff JE, editor. Ropivacaine, clinical pharmacology of local anesthetics. Boston: Butterworth Heinemann, 2000: 125–31
Burke D, Joypaul V, Thomson MF. Circumcision supplemented by dorsal penile nerve block with 0.75% ropivacaine: a complication. Reg Anesth Pain Med 2000; 25: 424–7
Johansson B, Glise H, Hallerback B, et al. Preoperative local infiltration with ropivacaine for postoperative pain relief after cholecystectomy. Anesth Analg 1994; 78: 210–4
Johansson B, Hallerback B, Stubberod A, et al. Preoperative local infiltration with ropivacaine for postoperative pain relief after inguinal hernia repair: a randomised controlled trial. Eur J Surg 1997; 163: 371–8
Mulroy MF, Wills RP. Spinal anesthesia for outpatients: appropriate agents and techniques. J Clin Anesth 1995; 7: 622–7
Pettersson N, Emanuelsson BM, Reventlid H, et al. High-dose ropivacaine wound infiltration for pain relief after inguinal hernia repair: a clinical and pharmacokinetic evaluation. Reg Anesth Pain Med 1998; 23: 189–96
Pettersson N, Berggren P, Larsson M, et al. Pain relief by wound infiltration with bupivacaine or high-dose ropivacaine after inguinal hernia repair. Reg Anesth Pain Med 1999; 24(6): 569–75
Fanelli G, Casati A, Beccaria P, et al. A double-blind comparison of ropivacaine, bupivacaine, and mepivacaine during sciatic and femoral nerve blockade. Anesth Analg 1998; 87: 597–600
Dixon WJ, Massey FJ. Introduction to statistical analysis. 4th ed. New York: McGraw-Hill, 1983: 428–39
Greengrass RA, Klein SM, D’Ercole FJ, et al. Lumbar plexus and sciatic nerve block for knee arthroplasty: comparison of ropivacaine and bupivacaine. Can J Anaesth 1998; 45: 1094–6
Raeder JC, Drosdahl S, Klaastad O, et al. Axillary brachial plexus block with ropivacaine 7.5 mg/ml: a comparative study with bupivacaine 5 mg/ml. Acta Anaesthesiol Scand 1999; 43: 794–8
Bertini L, Tagariello V, Mancini S, et al. 0.75% and 0.5% ropivacaine for axillary brachial plexus block: a clinical comparison with 0.5% bupivacaine. Reg Anesth Pain Med 1999; 24: 514–8
Rawal N, Allvin R, Axelsson K, et al. Patient-controlled regional analgesia (PCRA) at home: controlled comparison between bupivacaine and ropivacaine brachial plexus analgesia. Anesthesiology 2002; 96: 1290–6
Vaghadia H, Chan V, Ganapathy S, et al. A multicentre trial of ropivacaine 7.5mg × ml(-1) vs bupivacaine 5mg × ml(-1) for supra clavicular brachial plexus anesthesia. Can J Anaesth 1999; 46: 946–51
Hickey R, Blanchard J, Hoffman J, et al. Plasma concentrations of ropivacaine given with or without epinephrine for brachial plexus block. Can J Anaesth 1990; 37: 878–82
Salama H, Farr AK, Guyton DL. Anesthetic myotoxicity as a cause of restrictive strabismus after scleral buckling surgery. Retina 2000; 20: 478–82
Zink W, Graf BM, Sinner B, et al. Differential effects of bupivacaine on intracellular Ca2+ regulation: potential mechanisms of its myotoxicity. Anesthesiology 2002; 97: 710–6
Zink W, Kunst G, Martin E, et al. Differential effects of S(−)- ropivacaine and bupivacaine on intracellular Ca2+ homeostasis in mammalian skeletal muscle fibers [abstract]. Anesthesiology 2002; 96: A–972
Gioia L, Prandi E, Codenotti M, et al. Peribulbar anesthesia with either 0.75% ropivacaine or a 2% lidocaine and 0.5% bupivacaine mixture for vitreoretinal surgery: a double-blinded study. Anesth Analg 1999; 89: 739–42
Huha T, Ala-Kokko TI, Salomaki T, et al. Clinical efficacy and pharmacokinetics of 1% ropivacaine and 0.75% bupivacaine in peribulbar anaesthesia for cataract surgery. Anaesthesia 1999; 54: 137–41
Nociti JR, Serzedo PS, Zuccolotto EB, et al. Ropivacaine in peribulbar block: a comparative study with bupivacaine. Acta Anaesthesiol Scand 1999; 43: 799–802
Nociti JR, Serzedo PS, Zuccolotto EB, et al. Intraocular pressure and ropivacaine in peribulbar block: a comparative study with bupivacaine. Acta Anaesthesiol Scand 2001; 45: 600–2
Feldman HS, Covino BG. Comparative motor-blocking effects of bupivacaine and ropivacaine, a new amino amide local anesthetic, in the rat and dog. Anesth Analg 1988; 67: 1047–52
Malinovsky JM, Charles F, Baudrimont M, et al. Intrathecal ropivacaine in rabbits: pharmacodynamic and neurotoxicologic study. Anesthesiology 2002; 97: 429–35
van Kleef JW, Veering BT, Burm AG. Spinal anesthesia with ropivacaine: a double-blind study on the efficacy and safety of 0.5% and 0.75% solutions in patients undergoing minor lower limb surgery. Anesth Analg 1994; 78: 1125–30
Wahedi W, Nolte H, Klein P. Ropivacaine for spinal anesthesia: a dose-finding study [in German]. Anaesthesist 1996; 45: 737–44
Gautier PE, De Kock M, Van Steenberge A, et al. Intrathecal ropivacaine for ambulatory surgery. Anesthesiology 1999; 91: 1239–45
Gautier PE. Intrathecal ropivacaine. Acta Anaesthesiol Belg 2000; 51: 127–9
Whiteside JB, Burke D, Wildsmith JA. Spinal anaesthesia with ropivacaine 5mg ml(-1) in glucose 10mg ml(-1) or 50mg ml(-1). Br J Anaesth 2001; 86: 241–4
Khaw KS, Ngan Kee WD, Wong EL, et al. Spinal ropivacaine for cesarean section: a dose-finding study. Anesthesiology 2001; 95: 1346–50
Khaw KS, Ngan Kee WD, Wong M, et al. Spinal ropivacaine for cesarean delivery: a comparison of hyperbaric and plain solutions. Anesth Analg 2002; 94: 680–5
Soni AK, Miller CG, Pratt SD, et al. Low dose intrathecal ropivacaine with or without sufentanil provides effective analgesia and does not impair motor strength during labour: a pilot study. Can J Anaesth 2001; 48: 677–80
Chung CJ, Choi SR, Yeo KH, et al. Hyperbaric spinal ropivacaine for cesarean delivery: a comparison to hyperbaric bupivacaine. Anesth Analg 2001; 93: 157–61
Malinovsky JM, Charles F, Kick O, et al. Intrathecal anesthesia: ropivacaine versus bupivacaine. Anesth Analg 2000; 91: 1457–60
McNamee DA, Parks L, McClelland AM, et al. Intrathecal ropivacaine for total hip arthroplasty: double-blind comparative study with isobaric 7.5mg ml(-1) and 10mg ml(-1). Br J Anaesth 2001; 87: 743–7
Beilin Y, Galea M, Zahn J, et al. Epidural ropivacaine for the initiation of labor epidural analgesia: a dose finding study. Anesth Analg 1999; 88: 1340–5
Cascio MG, Gaiser RR, Camann WR, et al. Comparative evaluation of four different infusion rates of ropivacaine (2 mg/ml) for epidural labor analgesia. Reg Anesth Pain Med 1998; 23: 548–53
Benhamou D, Hamza J, Eledjam JJ, et al. Continuous extradural infusion of ropivacaine 2mg ml-1 for pain relief during labour. Br J Anaesth 1997; 78: 748–50
Sia AT, Chong JL. Epidural 0.2% ropivacaine for labour analgesia: parturient-controlled or continuous infusion? Anaesth Intensive Care 1999; 27: 154–8
Sia AT, Ruban P, Chong JL, et al. Motor blockade is reduced with ropivacaine 0.125% for parturient-controlled epidural analgesia during labour. Can J Anaesth 1999; 46: 1019–23
Meister GC, D’Angelo R, Owen M, et al. A comparison of epidural analgesia with 0.125% ropivacaine with fentanyl versus 0.125% bupivacaine with fentanyl during labor. Anesth Analg 2000; 90: 632–7
Gaiser RR, Venkateswaren P, Cheek TG, et al. Comparison of 0.25% ropivacaine and bupivacaine for epidural analgesia for labor and vaginal delivery. J Clin Anesth 1997; 9: 564–8
Muir HA, Writer D, Douglas J, et al. Double-blind comparison of epidural ropivacaine 0.25% and bupivacaine 0.25%, for the relief of childbirth pain. Can J Anaesth 1997; 44: 599–604
Stienstra R, Jonker TA, Bourdrez P, et al. Ropivacaine 0.25% versus bupivacaine 0.25% for continuous epidural analgesia in labor: a double-blind comparison. Anesth Analg 1995; 80: 285–9
Fischer C, Blanie P, Jaouen E, et al. Ropivacaine, 0.1%, plus sufentanil, 0.5 microg/ml, versus bupivacaine, 0.1%, plus sufentanil, 0.5 microg/ml, using patient-controlled epidural analgesia for labor: a double-blind comparison. Anesthesiology 2000; 92: 1588–93
Owen MD, D’Angelo R, Gerancher JC, et al. 0.125% ropivacaine is similar to 0.125% bupivacaine for labor analgesia using patient-controlled epidural infusion. Anesth Analg 1998; 86: 527–31
Owen MD, Dean LS. Ropivacaine. Expert Opin Pharmacother 2000; 1: 325–36
Campbell DC, Zwack RM, Crone LA, et al. Ambulatory labor epidural analgesia: bupivacaine versus ropivacaine. Anesth Analg 2000; 90: 1384–9
Lee BB, Ngan Kee WD, Lau WM, et al. Epidural infusions for labor analgesia: a comparison of 0.2% ropivacaine, 0.1% ropivacaine, and 0.1% ropivacaine with fentanyl. Reg Anesth Pain Med 2002; 27: 31–6
Lee BB, Ngan Kee WD, Wong EL, et al. Dose-response study of epidural ropivacaine for labor analgesia. Anesthesiology 2001; 94: 767–72
Writer WD, Stienstra R, Eddleston JM, et al. Neonatal outcome and mode of delivery after epidural analgesia for labour with ropivacaine and bupivacaine: a prospective meta-analysis. Br J Anaesth 1998; 81: 713–7
Owen MD, Thomas JA, Smith T, et al. Ropivacaine 0.075% and bupivacaine 0.075% with fentanyl 2 microg/mL are equivalent for labor epidural analgesia. Anesth Analg 2002; 94: 179–83
Hofmann-Kiefer K, Saran K, Brederode A, et al. Ropivacaine 2 mg/mL vs bupivacaine 1.25 mg/mL with sufentanil using patient-controlled epidural analgesia in labour. Acta Anaesthesiol Scand 2002; 46: 316–21
Clement HJ, Caruso L, Lopez F, et al. Epidural analgesia with 0.15% ropivacaine plus sufentanil 0.5 microgram ml-1 versus 0.10% bupivacaine plus sufentanil 0.5 microgram ml-1: a double blind comparison during labour. Br J Anaesth 2002; 88: 809–13
Landau R, Schiffer E, Morales M, et al. The dose-sparing effect of clonidine added to ropivacaine for labor epidural analgesia. Anesth Analg 2002; 95: 728–34
Aveline C, El Metaoua S, Masmoudi A, et al. The effect of clonidine on the minimum local analgesic concentration of epidural ropivacaine during labor. Anesth Analg 2002; 95: 735–40
Concepcion M, Arthur GR, Steele SM, et al. A new local anesthetic, ropivacaine: its epidural effects in humans. Anesth Analg 1990; 70: 80–5
Niesel HC, Eilingsfeld T, Kaiser H, et al. Ropivacaine for peridural anesthesia: studies on the dose-response relationship in orthopedic surgery [in German]. Reg Anaesth 1990; 13: 73–7
Whitehead E, Arrigoni B, Bannister J. An open study of ropivacaine in extradural anaesthesia. Br J Anaesth 1990; 64: 67–71
Kerkkamp HE, Gielen MJ, Edstrom HH. Comparison of 0.75% ropivacaine with epinephrine and 0.75% bupivacaine with epinephrine in lumbar epidural anesthesia. Reg Anesth 1990; 15: 204–7
Wood MB, Rubin AP. A comparison of epidural 1% ropivacaine and 0.75% bupivacaine for lower abdominal gynecologic surgery. Anesth Analg 1993; 76: 1274–8
Katz JA, Knarr D, Bridenbaugh PO. A double-blind comparison of 0.5% bupivacaine and 0.75% ropivacaine administered epidurally in humans. Reg Anesth 1990; 15: 250–2
Finucane BT, Sandler AN, McKenna J, et al. A double-blind comparison of ropivacaine 0.5%, 0.75%, 1.0% and bupivacaine 0.5%, injected epidurally, in patients undergoing abdominal. Can J Anaesth 1996; 43(5 Pt 1): 442–9
Wolff AP, Hasselstrom L, Kerkkamp HE, et al. Extradural ropivacaine and bupivacaine in hip surgery. Br J Anaesth 1995; 74: 458–60
Morrison LM, Emanuelsson BM, McClure JH, et al. Efficacy and kinetics of extradural ropivacaine: comparison with bupivacaine. Br J Anaesth 1994; 72: 164–9
Griffin RP, Reynolds F. Extradural anaesthesia for caesarean section: a double-blind comparison of 0.5% ropivacaine with 0.5% bupivacaine. Br J Anaesth 1995; 74: 512–6
Crosby E, Sandler A, Finucane B, et al. Comparison of epidural anaesthesia with ropivacaine 0.5% and bupivacaine 0.5% for caesarean section. Can J Anaesth 1998; 45: 1066–71
Datta S, Camann W, Bader A, et al. Clinical effects and maternal and fetal plasma concentrations of epidural ropivacaine versus bupivacaine for cesarean section. Anesthesiology 1995; 82: 1346–52
Muldoon T, Milligan K, Quinn P, et al. Comparison between extradural infusion of ropivacaine or bupivacaine for the prevention of postoperative pain after total knee arthroplasty. Br J Anaesth 1998; 80: 680–1
Badner NH, Reid D, Sullivan P, et al. Continuous epidural infusion of ropivacaine for the prevention of postoperative pain after major orthopaedic surgery: a dose-finding study. Can J Anaesth 1996; 43: 17–22
Schug SA, Scott DA, Payne J, et al. Postoperative analgesia by continuous extradural infusion of ropivacaine after upper abdominal surgery. Br J Anaesth 1996; 76: 487–91
Scott DA, Chamley DM, Mooney PH, et al. Epidural ropivacaine infusion for postoperative analgesia after major lower abdominal surgery: a dose finding study. Anesth Analg 1995; 81: 982–6
Turner G, Blake D, Buckland M, et al. Continuous extradural infusion of ropivacaine for prevention of postoperative pain after major orthopaedic surgery. Br J Anaesth 1996; 76: 606–10
Etches RC, Writer WD, Ansley D, et al. Continuous epidural ropivacaine 0.2% for analgesia after lower abdominal surgery. Anesth Analg 1997; 84: 784–90
Bertini L, Mancini S, Di-Benedetto P, et al. Postoperative analgesia by combined continuous infusion and patient-controlled epidural analgesia (PCEA) following hip replacement: ropivacaine versus bupivacaine. Acta Anaesthesiol Scand 2001; 45: 782–5
Scott DA, Blake D, Buckland M, et al. A comparison of epidural ropivacaine infusion alone and in combination with 1, 2, and 4 microg/mL fentanyl for seventy-two hours of postoperative analgesia after major abdominal surgery. Anesth Analg 1999; 88: 857–64
Kampe S, Weigand C, Kaufmann J, et al. Postoperative analgesia with no motor block by continuous epidural infusion of ropivacaine 0.1% and sufentanil after total hip replacement. Anesth Analg 1999; 89: 395–8
Lorenzini C, Moreira LB, Ferreira MB. Efficacy of ropivacaine compared with ropivacaine plus sufentanil for postoperative analgesia after major knee surgery. Anaesthesia 2002; 57: 424–8
Brodner G, Mertes N, Van Aken H, et al. What concentration of sufentanil should be combined with ropivacaine 0.2% wt/vol for postoperative patient-controlled epidural analgesia? Anesth Analg 2000; 90: 649–57
Finucane BT, Ganapathy S, Carli F, et al. Prolonged epidural infusions of ropivacaine (2 mg/ml) after colonic surgery: the impact of adding fentanyl. Anesth Analg 2001; 92: 1276–85
Berti M, Fanelli G, Casati A, et al. Patient supplemented epidural analgesia after major abdominal surgery with bupivacaine/fentanyl or ropivacaine/fentanyl. Can J Anaesth 2000; 47: 27–32
Senard M, Joris JL, Ledoux D, et al. A comparison of 0.1% and 0.2% ropivacaine and bupivacaine combined with morphine for postoperative patient-controlled epidural analgesia after major abdominal surgery. Anesth Analg 2002; 95: 444–9
Brodner G, Mertes N, Van Aken H, et al. Epidural analgesia with local anesthetics after abdominal surgery: earlier motor recovery with 0.2% ropivacaine than 0.175% bupivacaine. Anesth Analg 1999; 88: 128–33
Hubler M, Litz RJ, Sengebusch KH, et al. A comparison of five solutions of local anaesthetics and/or sufentanil for continuous, postoperative epidural analgesia after major urological surgery. Eur J Anaesthesiol 2001; 18: 450–7
Pouzeratte Y, Delay JM, Brunat G, et al. Patient-controlled epidural analgesia after abdominal surgery: ropivacaine versus bupivacaine. Anesth Analg 2001; 93: 1587–92
Jayr C, Beaussier M, Gustafsson U, et al. Continuous epidural infusion of ropivacaine for postoperative analgesia after major abdominal surgery: comparative study with i.v. PCA morphine. Br J Anaesth 1998; 81: 887–92
Wulf H, Worthmann F, Behnke H, et al. Pharmacokinetics and pharmacodynamics of ropivacaine 2 mg/ml, 5 mg/ml, or 7.5 mg/mL after ilioinguinal blockade for inguinal hernia repair in adults. Anesth Analg 1999; 89: 1471–4
Kampe S, Randebrock G, Kiencke P, et al. Comparison of continuous epidural infusion of ropivacaine and sufentanil with intravenous patient-controlled analgesia after total hip replacement. Anaesthesia 2001; 56: 1189–93
Ivani G, De Negri P, Conio A, et al. Ropivacaine-clonidine combination for caudal blockade in children. Acta Anaesthesiol Scand 2000; 44: 446–9
Ivani G, Lampugnani E, Torre M, et al. Comparison of ropivacaine with bupivacaine for paediatric caudal block. Br J Anaesth 1998; 81: 247–8
Ivani G, Mazzarello G, Lampugnani E, et al. Ropivacaine for central blocks in children. Anaesthesia 1998; 53Suppl. 2: 74–6
Khalil S, Campos C, Farag AM, et al. Caudal block in children: ropivacaine compared with bupivacaine. Anesthesiology 1999; 91: 1279–84
Da Conceicao MJ, Coelho L, Khalil M. Ropivacaine 0.25% compared with bupivacaine 0.25% by the caudal route. Paediatr Anaesth 1999; 9: 229–33
Koinig H, Krenn CG, Glaser C, et al. The dose-response of caudal ropivacaine in children. Anesthesiology 1999; 90: 1339–44
Luz G, Innerhofer P, Haussler B, et al. Comparison of ropivacaine 0.1% and 0.2% with bupivacaine 0.2% for single-shot caudal anaesthesia in children. Paediatr Anaesth 2000; 10: 499–504
Bosenberg A, Thomas J, Lopez T, et al. The efficacy of caudal ropivacaine 1, 2 and 3mg x l(-1) for postoperative analgesia in children. Paediatr Anaesth 2002; 12: 53–8
De Negri P, Ivani G, Visconti C, et al. The dose-response relationship for clonidine added to a postoperative continuous epidural infusion of ropivacaine in children. Anesth Analg 2001; 93: 71–6
Lee HM, Sanders GM. Caudal ropivacaine and ketamine for postoperative analgesia in children. Anaesthesia 2000; 55: 806–10
De Negri P, Ivani G, Visconti C, et al. How to prolong postoperative analgesia after caudal anaesthesia with ropivacaine in children: S-ketamine versus clonidine. Paediatr Anaesth 2001; 11: 679–83
Kokki H, Ruuskanen A, Karvinen M. Comparison of epidural pain treatment with sufentanil-ropivacaine infusion with and without epinephrine in children. Acta Anaesthesiol Scand 2002; 46: 647–53
Capogna G. Ropivacaine and bupivacaine in obstetric analgesia. Eur J Anaesthesiol 2002; 19: 237–9
Lyons G, Columb M, Wilson RC, et al. Epidural pain relief in labour: potencies of levobupivacaine and racemic bupivacaine. Br J Anaesth 1998; 81: 899–901
Lacassie HJ, Columb MO, Lacassie HP, et al. The relative motor blocking potencies of epidural bupivacaine and ropivacaine in labor. Anesth Analg 2002; 95: 204–8
McClellan KJ, Faulds D. Ropivacaine: an update of its use in regional anaesthesia. Drugs 2000; 60: 1065–93
D’Angelo R, James RL. Is ropivacaine less potent than bupivacaine? Anesthesiology 1999; 90: 941–3
Stienstra R. A closer look at the new local anesthetics. Acta Anaesthesiol Belg 1999; 50: 211–6
Wildsmith JA. New local anaesthetics: how much is improved safety worth? Acta Anaesthesiol Scand 2001; 45: 652–3
Pasqualucci A, Contardo R, Da Broi U, et al. The effects of intraperitoneal local anesthetic on analgesic requirements and endocrine response after laparoscopic cholecystectomy: a randomized double-blind controlled study. J Laparoendosc Surg 1994; 4: 405–12
Chundrigar T, Hedges A, Morris R, et al. Intraperitoneal bupivacaine for effective pain relief after laparoscopic cholecystectomy. Ann R Coll Surg Engl 1993; 75: 473–39
Bisgaard T, Klarskov B, Kristiansen VB, et al. Multi-regional local anesthetic infiltration during laparoscopic cholecystectomy in patients receiving prophylactic multi-modal analgesia: a randomized, double-blinded, placebo-controlled study. Anesth Analg 1999; 89: 1017–24
Dreher JK, Nemeth D, Limb R. Pain relief following day case laparoscopic tubal ligation with intra-peritoneal ropivacaine: a randomised double blind control study. Aust N Z J Obstet Gynaecol 2000; 40(4): 434–7
Goldstein A, Grimault P, Henique A, et al. Preventing postoperative pain by local anesthetic instillation after laparoscopic gynecologic surgery: a placebo-controlled comparison of bupivacaine and ropivacaine. Anesth Analg 2000; 91: 403–7
Labaille T, Mazoit JX, Paqueron X, et al. The clinical efficacy and pharmacokinetics of intraperitoneal ropivacaine for laparoscopic cholecystectomy. Anesth Analg 2002; 94: 100–5
Gupta A, Thorn SE, Axelsson K, et al. Postoperative pain relief using intermittent injections of 0.5% ropivacaine through a catheter after laparoscopic cholecystectomy. Anesth Analg 2002; 95: 450–6
Rautoma P, Santanen U, Avela R, et al. Diclofenac premedication but not intra-articular ropivacaine alleviates pain following day-case knee arthroscopy. Can J Anaesth 2000; 47: 220–4
Muller M, Burkhardt J, Borchardt E, et al. Postoperative analgesic effect after intra-articular morphine or ropivacaine following knee arthroscopy: a prospective randomized, doubleblinded study [in German]. Schmerz 2001; 15: 3–9
Klein SM, Nielsen KC, Martin A, et al. Interscalene brachial plexus block with continuous intraarticular infusion of ropivacaine. Anesth Analg 2001; 93: 601–5
Scott D, Lee A, Fagan D, et al. Acute toxicity of ropivacaine compared with that of bupivacaine. Anesth Analg 1989; 69: 563–9
Knudsen K, Beckman M, Blomberg S. Central nervous and cardiovascular effects during intravenous infusions of ropivacaine, bupivacaine and placebo in volunteers. Br J Anaesth 1997; 78: 507–14
Voulgaropoulos D, Johnson M, Covino B. Local Anesthetic Toxicity. Semin in Anesth 1990; 9: 8–15
Rowlingson JC. Toxicity of local anesthetic additives. Reg Anesth 1993; 18: 453–60
McCaughey W. Adverse effects of local anaesthetics. Drug Saf 1992; 7: 178–89
Reiz S, Nath S. Cardiotoxicity of local anaesthetic agents. Br J Anaesth 1986; 58: 736–46
Vladimirov M, Nau C, Mok W, et al. Potency of bupivacaine stereoisomers tested in vitro and in vivo: biochemical, electrophysiological, and neurobehavioral studies. Anesthesiology 2000; 93: 744–55
Graf BM, Abraham I, Eberbach N, et al. Differences in cardiotoxicity of bupivacaine and ropivacaine are the result of physicochemical and stereoselective properties. Anesthesiology 2002; 96: 1427–34
Reiz S, Haggmark S, Johansson G, et al. Cardiotoxicity of ropivacaine: a new amide local anaesthetic agent. Acta Anaesthesiol Scand 1989; 33: 93–8
Brun A. Effect of procaine, carbocaine and xylocaine on cutaneous muscle in rabbits and mice. Acta Anaesthesiol Scand 1959; 3: 59–73
Foster AH, Carlson BM. Myotoxicity of local anesthetics and regeneration of the damaged muscle fibers. Anesth Analg 1980; 59: 727–36
Hogan Q, Dotson R, Erickson S, et al. Local anesthetic myotoxicity: a case and review. Anesthesiology 1994; 80: 942–7
Sadeh M, Czyewski K, Stern LZ. Chronic myopathy induced by repeated bupivacaine injections. J Neurol Sci 1985; 67: 229–38
Parris WC, Dettbarn WD. Muscle atrophy following nerve block therapy [letter]. Anesthesiology 1988; 69: 289
Parris WCV, Dettbarn WD. Muscle atrophy following bupivacaine trigger point injection. Anesthesiol Rev 1989; 16: 50–3
Komorowski TE, Shepard B, Okland S, et al. An electron microscopic study of local anesthetic-induced skeletal muscle fiber degeneration and regeneration in the monkey. J Orthop Res 1990; 8: 495–503
Carlson BM, Shepard B, Komorowski TE. A histological study of local anesthetic-induced muscle degeneration and regeneration in the monkey. J Orthop Res 1990; 8: 485–94
Hall-Craggs EC. Early ultrastructural changes in skeletal muscle exposed to the local anaesthetic bupivacaine (Marcaine). Br J Exp Pathol 1980; 61: 139–49
Benoit PW, Belt WD. Destruction and regeneration of skeletal muscle after treatment with a local anaesthetic, bupivacaine (Marcaine). J Anat 1970; 107: 547–56
Benoit PW. Reversible skeletal muscle damage after administration of local anesthetics with and without epinephrine. J Oral Surg 1978; 36: 198–201
Pere P, Watanabe H, Pitkanen M, et al. Local myotoxicity of bupivacaine in rabbits after continuous supraclavicular brachial plexus block. Reg Anesth 1993; 18: 304–7
Kytta J, Heinonen E, Rosenberg PH, et al. Effects of repeated bupivacaine administration on sciatic nerve and surrounding muscle tissue in rats. Acta Anaesthesiol Scand 1986; 30: 625–9
Benoit PW, Yagiela A, Fort NF. Pharmacologic correlation between local anesthetic-induced myotoxicity and disturbances of intracellular calcium distribution. Toxicol Appl Pharmacol 1980; 52: 187–98
Brodner G, Mertes N, Buerkle H, et al. Acute pain management: analysis, implications and consequences after prospective experience with 6349 surgical patients. Eur J Anaesthesiol 2000; 17: 566–75
Macaire P, Gaertner E, Capdevila X. Continuous post-operative regional analgesia at home. Minerva Anestesiol 2001; 67: 109–16
Acknowledgements
We gratefully acknowledge Professor Dr Eike Martin, F.A.N.Z.C.A. (Ruprechts-Karl-University, Heidelberg, Germany) for his support. No sources of funding were used to assist in the preparation of this review. The authors have no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zink, W., Graf, B.M. Benefit-Risk Assessment of Ropivacaine in the Management of Postoperative Pain. Drug-Safety 27, 1093–1114 (2004). https://doi.org/10.2165/00002018-200427140-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-200427140-00003