Summary
The pharmacokinetics of different cardiac glycosides are altered by renal dysfunction in different ways, depending on their basic pharmacokinetic properties.
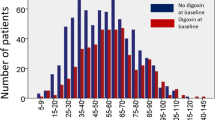
Digoxin: The linearity of digoxin pharmacokinetics is unchanged by renal dysfunction, as is the bioavailability. Protein binding may be slightly reduced, but the change is of no clinical significance. The apparent volume of distribution is reduced by one-third to one-half, the change being roughly proportional to the degree of renal impairment. The significance of this change in terms of adjustment of the loading dose is controversial. I believe that the initial oral loading dose should be reduced from 15 μg/kg to 10 μg/kg in renal dysfunction, and supplemented only if there is evidence of a lack of response and no evidence of toxicity.
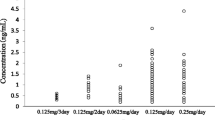
The renal clearance of digoxin is reduced in renal dysfunction and becomes very closely related to the measured creatinine clearance at values of creatinine clearance below 30 ml/min. As a result, the renal elimination rate constant, and therefore the fraction of the total body load lost per day via the kidneys, falls in renal dysfunction. In contrast, the non-renal clearance of digoxin is probably unaffected. However, because of the fall in apparent volume of distribution the non-renal elimination rate constant rises slightly, accounting for the slight increase in faecally excreted digoxin in renal dysfunction. This rise in the non-renal fractional daily loss is not sufficient to counteract the fall in renal fractional daily loss and digoxin maintenance dosages at steady-state need to be reduced. For this purpose the creatinine clearance acts as an initial guide to the extent of the expected reduction in dose, but doses altered on this basis should be regarded as first approximations to the correct dose, and the dose subsequently readjusted according to the patient’s clinical response, using the plasma digoxin concentration as a guide, it must be remembered, however, that because of technical problems with digoxin radioimmunoassay in renal dysfunction, and because of the difficulty in interpretation of the result, the plasma digoxin concentration in renal dysfunction is of less value than it is in normal renal function. The overall half-life of digoxin is prolonged in renal dysfunction and it therefore takes longer for a steady-state to be reached during maintenance dose therapy without a loading dose, and longer for toxicity, when it occurs, to resolve.
Negligible amounts of digoxin are removed from the body by dialysis procedures. A transplanted kidney retains its ability to handle digoxin, and after transplantation the pharmacokinetics of digoxin return towards normal, depending on the overall improvement in renal function achieved.
Digitoxin: There are technical problems with the measurement of digitoxin because of the need to separate digitoxin and its metabolites chromatographically before using the measurement techniques commonly applied. Such separation has not always been carried out, and this makes the interpretation of the available data more difficult.
The bioavailability of digitoxin is unaffected by renal dysfunction. Protein binding is probably significantly reduced but the clinical significance of this effect is unclear since the apparent volume of distribution and total body clearance of digitoxin appear to be unchanged. In the nephrotic syndrome, which must be considered separately from the other forms of renal dysfunction, there is impaired protein binding but also probably loss of protein bound drug via the renal glomerulus. This leads to a proportionately large increase in total body and renal clearances, a shortening of the half-life and a fall in the steady-state plasma digitoxin concentrations. In other forms of renal dysfunction there is probably no change in half-life or in steady-state plasma digitoxin concentrations. There does seem to be a decrease in digitoxin renal clearance but this may be compensated for by increases in nonrenal clearance, both by non-renal excretion of unchanged digitoxin and by metabolic clearance, with increased formation of the active hydroxylated and hydrolysed metabolites, as well as of the relatively inactive reduced metabolites. Overall, the changes seem to contribute little of clinical importance. Little digitoxin is removed from the body by dialysis procedures.
Lanatoside C, deslanoside, and the acylated digoxins: Since these glycosides are largely metabolised to digoxin, one would expect changes in their pharmacokinetics similar to those of digoxin. However, there is only enough information to conclude that this is probably so in the case of β-methyldigoxin. The protein binding of β-methyldigoxin is reduced, as is its apparent volume of distribution, and total body clearance. The reduction in total body clearance is mostly attributable to a reduction in renal clearance, which falls in parallel with creatinine clearance, although always remaining lower than creatinine clearance. Non-renal clearance falls little or not at all. As a result of these changes the overall half-life of β-methyldigoxin is prolonged and the fractional daily loss at steady-state is decreased. Dosages of β-methyldigoxin therefore need to be reduced in renal dysfunction. Little β-methyldigoxin is removed by haemodialysis.
For α-acetyldigoxin, renal clearance is reduced in proportion to renal function, and the half-life is prolonged. Little is removed by haemodialysis.
Other glycosides: Little information is available about other cardiac glycosides. What little information there is, however, suggests that, as one would expect, the half-life is prolonged and renal clearance reduced for those glycosides which are mostly eliminated via the urine, while little or no change occurs for those glycosides which are mostly metabolised. Thus, for ouabain (g-strophanthin), and k-strophanthin, the half-life is prolonged and renal excretion decreased, while for proscillaridin, methylproscillaridin, and peruvoside there is no change. None of these glycosides is much affected by haemodialysis.
Despite the changes in pharmacokinetics of digoxin compared with digitoxin, there is little to choose between the two drugs for use in patients with renal dysfunction. Arguments in favour of one or other can be marshalled but there is no good evidence that one is preferable to the other.
Similar content being viewed by others
References
Ackerman, G.L.; Doherty, J.E. and Flanigan, W.J.: Peritoneal dialysis and hemodialysis of tritiated digoxin. Annals of Internal Medicine 67: 718–723 (1967).
Angelino, P.F.; Matta, F.; Bartolozzi, S.; Ladetto, P. and Rotunno, M.: Cinetica della betametil-digossina nei diversi gradi di funzionalitá renale. Bolletino della Societa Italiana Cardiologica 22: 773–778 (1977).
Aronson, J.K.: Monitoring digoxin therapy: III. How useful are the nomograms?. British Journal of Clinical Pharmacology 5: 55–64 (1978).
Aronson, J.K. and Grahame-Smith, D.G.: Digoxin therapy: Textbooks, theory and practice. British Journal of Clinical Pharmacology 3: 639–648 (1976a).
Aronson, J.K. and Grahame-Smith, D.G.: Altered distribution of digoxin in renal failure — a cause of digoxin toxicity?. British Journal of Clinical Pharmacology 3: 1045–1051 (1976b).
Aronson, J.K. and Grahame-Smith, D.G.: Monitoring digoxin therapy: II. Determinants of the apparent volume of distribution. British Journal of Clinical Pharmacology 4: 223–227 (1977).
Aronson, J.K.; Grahame-Smith, D.G. and Wigley, F.M.: Monitoring digoxin therapy. The use of plasma digoxin concentration measurements in the diagnosis of digoxin toxicity. Quarterly Journal of Medicine NS 47: 111–122 (1978).
Beckmann, H.; Belz, G.G. and Quellhorst, E.: Die Eliminationsgeschwindigkeit von Meproscillarin nach Wiederholter Applikation bei Patienten mit eingeschränkter Nierenfunktion. Arzneimittel-Forschung 28: 565–567 (1978).
Beckmann, H.; Belz, G.G. and Quellhorst, E.: Meproscillarin bei gleichzeitiger Nieren- und Herzinsuffizienz. Medizinische Klinik 74: 1761–1766 (1979).
Belz, G.G. and Brech, W.J.: Plasmaspiegel und Kumulationsverhalten von Proscillaridin bei Niereninsuffizienz. Klinische Wochenschrift 52: 650–644 (1974).
Belz, G.G.; Nübling, H.; Schmidt-Wiederkehr, P. and Franz, H.E.: Plasmakonzentrationen und Elimination von Methylproscillaridin bei Niereninsuffizienz. Klinische Wochenschrift 52: 1078–1081 (1974).
Belpaire, F.M.; Bogaert, M.G. and de Broe, M.E.: Radioimmunoassay of digoxin in renal failure: a comparison of different commercial kits. Clinica Chimica Acta 62: 255–261 (1975).
Belpaire, F.M.; Bogaert, M.G. and Mussche, M.M.: Influence of acute renal failure on the protein binding of drugs in animals and in man. European Journal of Clinical Pharmacology 11: 27–32 (1977).
Bloom, P.M.; Nelp, W.B. and Tuell, S.H.: Relationship of the excretion of tritiated digoxin to renal function. American Journal of the Medical Sciences 251: 133–144 (1966).
Boden, G. and von Unruh, E.: Enhanced transformation of digitoxin to dihydrodigitoxin in humans with renal failure. Journal of Clinical Pharmacology 19: 195–199 (1979).
Brass, H.: Zur Therapie mit Herzglykosiden bei Patienten mit Niereninsuffizienz. Deutsche Medizinische Wochenschrift 95: 754–758 (1970).
Brass, H. and Phillips, H.: Die Elimination von α-Acetyldigoxin und k-Strophanthin bei Niereninsuffizienz. Klinische Wochenschrift 48: 972–978 (1970).
Cusack, B.; Kelly, J.; O’Malley, K.; Noel, J.; Lavan, J. and Horgan, J.: Digoxin in the elderly: Pharmacokinetic consequences of old age. Clinical Pharmacology and Therapeutics 25: 772–776 (1979).
Dengler, H.J.; Bodem, G. and Wirth, K.: Pharmacokinetic and metabolic studies with lanatoside C, α- and β-acetyldigoxin and digoxin in man. Proceedings of the 5th International Congress of Pharmacology, pp.112–126 (Karger, Basel 1973).
Doherty, J.E.; Flanigan, W.J.; Dalrymple, G.V.; Gammill, J. and Sherwood, J.: Tritiated digoxin. XVII. Excretion and turnover times in normal donors before and after nephrectomy and in the paired recipient of the kidney after transplantation. American Journal of Cardiology 29: 470–474 (1972).
Doherty, J.E.; Flanigan, W.J.; Patterson, R.M. and Dalrymple, G.V.: The excretion of tritiated digoxin in normal human volunteers before and after unilateral nephrectomy. Circulation 40: 555–561 (1969).
Doherty, J.E.; Flanigan, W.J. and Perkins, W.H.: Tritiated digoxin excretion of patients following renal transplantation. Circulation 37: 865–869 (1968).
Doherty, J.E.; Flanigan, W.J.; Perkins, W.H. and Ackerman, G.L.: Studies with tritiated digoxin in anephric human subjects. Circulation 35: 298–303 (1967).
Ewy, G.A.; Kapadia, G.G.; Yao, L.; Lullin, M. and Marcus, F.I.: Digoxin metabolism in the elderly. Circulation 319: 449–453 (1969).
Finkelstein, F.O.; Goffinet, J.A.; Hendler, E.D. and Lindenbaum, J.: Pharmacokinetics of digoxin and digitoxin in patients undergoing hemodialysis. American Journal of Medicine 58: 525–531 (1975).
Gault, M.H.; Churchill, D.N. and Kalra, J.: Loading dose of digoxin in renal failure. British Journal of Clinical Pharmacology 9: 593–597 (1980).
Gault, M.H.; Jeffrey, J.R.; Chirito, E. and Ward, L.L.: Studies of digoxin dosage, kinetics and serum concentrations in renal failure and review of the literature. Nephron 17: 161–187 (1976).
Gault, M.H.; Sugden, D.; Maloney, G; Ahmed, M. and Tweed-dale, M.: Biotransformation and elimination of digoxin with normal and minimal renal function. Clinical Pharmacology and Therapeutics 25: 499–513 (1979).
Garrett, E,R. and Hinderung, P.H.: Pharmacokinetics of β-methyldigoxin in healthy humans. IV: Comparisons of radioimmunoassays, total radioactivity, and specific assays of β-methyldigoxin and digoxin in plasma. Journal of Pharmaceutical Sciences 66: 806–810 (1977).
Gibson, T.P. and Nelson, H.A.: The question of cumulation of digoxin metabolites in renal failure. Clinical Pharmacology and Therapeutics 27: 219–223 (1980).
Gobbi, A.; Tabacchi, G.C.; Giangrande, A. and Crespi, G.: Valutazione radioimmunologica della digitalemia in cordo di terapia con beta-metil-digoxin in pazienti con diverso grado di funzionalita renale. Minerva Cardioangiologica 28: 445–451 (1980).
Grabensee, B.; Peters, U.; Risler, T. and Grosse-Brockhoff, F.: Digitoxin and digoxin in patients with chronic renal failure and on haemodialysis; in Bodem and Dengler (Eds) Cardiac Glycosides, pp.317–323 (Springer-Verlag, Berlin/Heidelberg 1978).
Halkin, H; Sheiner, L.B.; Peck, C.C. and Melmon, K.L.: Determinants of the renal clearance of digoxin. Clinical Pharmacology and Therapeutics 17: 385–394 (1975).
Hinderling, P.H.; Garrett, E.R. and Wester, R.C.: Pharmacokinetics of β—methyldigoxin in healthy humans. I: Intravenous studies. Journal of Pharmaceutical Sciences 66: 242–253 (1977).
lisalo, E. and Forsstróm, J.: Elimination of digoxin during maintenance haemodialysis. Annals of Clinical Research 6: 203–206 (1974).
Jelliffe, R.W.: A chemical determination of urinary digitoxin and digoxin in man. Journal of Clinical Investigation 67: 694–708 (1966).
Jelliffe, R.W.: A mathematical analysis of digitalis kinetics in patients with normal and reduced renal function. Mathematical Biosciences 1: 305–326 (1967).
Jelliffe, R.W.; Buell, J.; Kalaba, R.; Sridhar, R. and Rockwell, R.: A mathematical study of the metabolic conversion of digitoxin in man. Mathematical Biosciences 6: 387–403 (1970).
Jusko, W.J.; Szefler, S.J. and Goldfarb, A.L.: Pharmacokinetic design of digoxin dosage regimens in relation to renal function. Journal of Clinical Pharmacology 14: 525–535 (1974).
Jusko, W.J. and Weintraub, M.: Myocardial distribution of digoxin and renal function. Clinical Pharmacology and Therapeutics 16: 449–454 (1974).
Kaufmann, B.; Olcay, A.; Schaumann, W.; Teufel, W. and Weib, W.: Pharmacokinetics of metildigoxin and digoxin in geriatric patients with normal and elevated serum creatinine levels. Clinical Pharmacokinetics 6: 463–468 (1981).
Keller, F.; Blumenthal, H.P.; Märtin, K. and Rietbrock, N.: Overall pharmacokinetics during prolonged treatment of healthy volunteers with digoxin and β-methyldigoxin. European Journal of Clinical Pharmacology 12: 387–392 (1977).
Keller, F.; Molzahn, M. and Ingerowski, R.: Digoxin dosage in renal insufficiency: Impracticality of basing it on the creatinine clearance, body weight and volume of distribution. European Journal of Clinical Pharmacology 18: 433–441 (1980).
Klehr, H.U.; Otten, H.; von Unruh, G. and Bodem, G.: Digitoxinstoffwechsel bei niereninsuffizienten Patienten. Verhandlung Deutsches Gesell für Inner Med 83: 1656–1659 (1977).
Koup, J.R.; Greenblatt, D.J.; Jusko, W.J.; Smith, T.W. and Koch-Weser, J.: Pharmacokinetics of digoxin in normal subjects after intravenous bolus and infusion doses. Journal of Pharmacokinetics and Biopharmaceutics 3: 181–192 (1975a).
Koup, J.R.: Jusko, W.J.; Elwood, C.M. and Kohli, R.K.: Digoxin pharmacokinetics: Role of renal failure in dosage regimen design. Clinical Pharmacology and Therapeutics 18: 9–21 (1975b).
Kramer, P.; Korenkamp, J.; Willins, B. and Scheler, F.: Das Kumulationsverhalten verschiedener Herzglykoside bei Anurie. Deutsche Medizinische Wochenschrift 95: 444–453 (1970a).
Kramer, P.; Horenkamp, J.; Quellhorst, E. and Scheler, F.: Comparative studies on dialysance and renal clearance of various cardiac glycosides. Proceedings of the European Dialysis and Transplant Association 7: 212–216 (1970b).
Kramer, P.; Köthe, E.; Saul, J. and Scheler, F.: Uraemic and normal plasma protein binding of various cardiac glycosides under “in vivo” conditions. European Journal of Clinical Investigation 4: 53–58 (1974a).
Kramer, W.G.; Leis, R.P.; Cobb, T.C.; Forester, W.F.; Visconti, J.A.; Wanke, L.A.; Boxenbaum, H.G. and Reuning, R.H.: Pharmacokinetics of digoxin: Comparison of a two-and a three-compartment model in man. Journal of Pharmacokinetics and Biopharmaceutics 2: 299–312 (1974b).
Kramer, P.; Quellhorst, E.; Horenkamp, J. and Scheler, F.: Dialysance und prozentuale Elimination verschiedener Herzglykoside Während der Hämo- und Peritonealdialyse. Klinische Wochenschrift 50: 609–613 (1972).
Kramer, P.; Stroh, E.; Matthei, D.; Teiwes, F. and Scheler, F.: Increased digitalis tolerance in uremic patients; in Bodem and Dengler (Eds) Cardiac Glycosides, pp. 304–313 (Springer-Verlag, Berlin/Heidelberg 1978).
Lahrtz, H.; Reinold, H.M. and van Zwieten, P.A.: Serumkonzentration and Ausscheidung von 3H-Digitoxin beim Menschen unter normal und pathologischen Bendingungen. Klinische Wochenschrift 47: 695–700 (1969a).
Lahrtz, H.; Reinold, H.M. and van Zwieten, P.A.: Serum concentration and urinary excretion of 3H-ouabain in patients suffering from liver or kidney diseases. Pharmacologia Clinica 1: 114–118 (1969b).
Larbig, D. and Haasis, R.: Plasma-tissue distribution of different cardiac glycosides; in Bodem and Dengler (Eds) Cardiac Glycosides, pp. 126–133 (Springer-Verlag, Berlin/Heidelberg 1978).
Levitt, B.; Cagin, N.; Kleid, J.; Somberg, J. and Gillis, R.: Role of the nervous system in the genesis of cardiac rhythm disorders. American Journal of Cardiology 37: 1111–1113 (1976).
Lukas, D.S.: Some aspects of the distribution and disposition of digitoxin in man. Annals of the New York Academy of Sciences 179: 338–361 (1971).
Lukas, D.S. and Peterson, R.E.: Determination of digitoxin in plasma by double isotope dilution derivative assay. Journal of Clinical Investigation 43: 1242 (1964).
Lukas, D.S. and Peterson, R.E.: Double isotope dilution derivative assay of digitoxin in plasma, urine, and stool of patients maintained on the drug. Journal of Clinical Investigation 45: 782–795 (1966).
Marzo, A.; Ghirardi, P.; Maggi, G.C.; Piscitello, F.; Gobetti, F. and Marchetti, G.: Livelli plasmatici ed eliminazione urinaria del k-strofantoside somministrato per veno in pazienti affetli da insufficienza renale. Bolletino della Societa Italiana Biologica Sperimentale 50: 1594–1597 (1974).
Nyberg, L.; Anderson, K.-E. and Bertler, A.: Bioavailability of digoxin from tablets. II. Radioimmunoassay and disposition pharmacokinetics of digoxin after intravenous administration. Acta Pharmaceutica Suecica 11: 459–470 (1974).
Ohnhaus, E.E.: Bioavailability of digoxin in renal insufficiency and heart failure; in Bodem and Dengler (Eds) Cardiac Glycosides, pp.181–185 (Springer-Verlag, Berlin/Heidelberg 1978).
Ohnhaus, E.E.; Lenzinger, H.R. and Galeazzi, R.L.: Comparison of two different loading doses of digoxin in severe renal impairment. European Journal of Clinical Pharmacology 18: 467–472 (1980).
Ohnhaus, E.E.; Spring, P. and Dettli L.: Eliminationskinetik und Dosierung von Digoxin bei Patienten mit Niereninsuffizienz. Deutsche Medizinische Wochenschrift 99: 1797–1803 (1974).
Ohnhaus, E.E.; Vozeh, S. and Nüesch, E.: Absolute bioavailability of digoxin in chronic renal failure. Clinical Nephrology 11: 302–306 (1979).
Okada, R.D.; Hager, W.D.; Graves, P.E.; Mayersohn, M.; Perrier, D.G. and Marcus, F.I.: Relationship between plasma concentration and dose of digoxin in patients with and without renal impairment. Circulation 58: 1196–1203 (1978a).
Okada, R.D.; Hager, W.D.; Marcus, F.I.; Perrier, D. and Graves, P.: Predicting digoxin dosage from creatinine clearance. Annals of Internal Medicine 88: 133 (1978b).
Pancorbo, S. and Comty, C.: Digoxin pharmacokinetics in continuous peritoneal dialysis. Annals of Internal Medicine 93: 639 (1980).
Paulson, M.F. and Welling, P.G.: Calculation of serum digoxin levels in patients with normal and impaired renal function. Journal of Clinical Pharmacology 16: 660–665 (1976).
Peters, U.; Grabensee, B.; Hausamen, T.-U.; Fritsch, W.-P. and Grosse-Brockhoff, F.: Pharmacokinetik von Digitoxin bei chronischer Niereninsuffizienz. Deutsche Medizinisches Wochenschrift 102: 109–115 (1977).
Rabkin, S.W. and Grupp, G.: A two compartment open model for digoxin pharmacokinetics in patients receiving a wide range of digoxin doses. Acta Cardiologica (Bruxelles) 30: 343–351 (1975).
Rasmussen, K.; Jervell, J. and Storstein, O.: Clinical use of a bioassay of serum digitoxin activity. European Journal of Clinical Pharmacology 3: 236–242 (1971).
Rasmussen, K.; Jervell, J.; Storstein, L. and Gjerdrum, K.: Digitoxin kinetics in patients with impaired renal function. Clinical Pharmacology and Therapeutics 13: 6–14 (1972).
Reuning, R.H.; Sams, R.A. and Notari, R.E.: Role of pharmacokinetics in drug dosage adjustment. I. Pharmacologic effect kinetics and apparent volume of distribution of digoxin. Journal of Clinical Pharmacology 13: 127–141 (1973).
Rietbrock, N.; Rennekamp, C.; Rennekamp, H.; von Bergman, K. and Abshagen, U.: Demethylation and cleavage of glycosidic bonds of 4111-methyldigoxin in man. Naunyn-Schmiedeberg’s Archives of Pharmacology 272: 450–453 (1972).
Seiden, L.; Margolies, M.N. and Smith. T.W.: Renal and gastrointestinal excretion of ouabain in dog and man. Journal of Pharmacology and Experimental Therapeutics 188: 615–623 (1974).
Seiden, R. and Haynie, G.: Ouabain plasma level kinetics and removal by dialysis in chronic renal failure. Annals of Internal Medicine 83: 15–19 (1975).
Shoeman, D.W. and Azarnoff, D.L.: The alteration of plasma proteins in uraemia as reflected in their ability to bind digitoxin and diphenylhydantoin. Pharmacology 7: 169–177 (1972).
Steiness, E.: Renal excretion of digoxin; in Storstein et al. (Eds) Symposium on Digitalis, pp. 178–183 (Glydendal Norsk For1ag 1973).
Stall, R.G.; Christensen, M.S.; Sakmar, E.; Blair, D. and Wagner, J.G.: Determination of bioavailability of digitoxin using the radioimmunoassay procedure. Journal of Pharmaceutical Sciences 62: 1615–1620 (1973).
Storstein, L.: The influence of renal function on the pharmacokinetics of digitoxin; in Storstein et al. (Eds) Symposium on Digitalis, pp.158–168 (Gyldendal Norsk Forlag 1973).
Storstein, L.: Studies on digitalis. I. Renal excretion of digitoxin and its metabolites. Clinical Pharmacology and Therapeutics 16: 14–24 (1974a).
Storstein, L.: Studies on digitalis. II. The influence of impaired renal function on the renal excretion of digitoxin and its cardioactive metabolites. Clinical Pharmacology and Therapeutics 16: 25–34 (1974b).
Storstein, L.: Studies on digitalis. III. Biliary excretion and enterohepatic circulation of digitoxin and its cardioactive metabolites. Clinical Pharmacology and Therapeutics 17: 313–320 (1975).
Storstein, L.: Studies on digitalis, V. The influence of impaired renal function and drug interaction on serum protein binding of digitoxin and digoxin. Clinical Pharmacology and Therapeutics 20: 6–14 (1976a).
Storstein, L.: Studies on digitalis. VII. Influence of nephrotic syndrome on protein binding, pharmacokinetics, and renal excretion of digitoxin and cardioactive metabolites. Clinical Pharmacology and Therapeutics 20: 158–166 (1976b).
Storstein, L. and Janssen, H.: Studies on digitalis. VI. The effect of heparin on serum protein binding of digitoxin and digoxin. Clinical Pharmacology and Therapeutics 20: 15–23 (1976).
Sumner, D.J.; Russell, A.J. and Whiting, B.: Digoxin pharmacokinetics: Multicompartmental analysis and its clinical implications. British Journal of Clinical Pharmacology 3: 221–229 (1976).
Szefler, S.J. and Jusko, W.J.: Decreased volume of distribution of digoxin in a patient with renal failure. Research Communications in Chemical Pathology and Pharmacology 6: 1095–1098 (1973).
Tsujimoto, G.; Sasaki, T.; Ishizaki, T.; Suganuma, T. and Hirayama, H.: Re-examination of digoxin dosage regimen: Comparison of the proposed nomograms or formulae in elderly patients. British Journal of Clinical Pharmacology 13: 493–500 (1982).
Twittenhoff, W.D.; Strauch, M.; Kütemeyer, M.; Koch, K. and Schaumann, W.: Extrarenal clearance, distribution volume, and elimination rate of digoxin and metildigoxin in anuric patients. International Journal of Clinical Pharmacology, Therapy and Toxicology 19: 405–408 (1981).
van der Vijgh, W.J.F. and Oe, P.L.: Pharmacokinetic aspects of digoxin in patients with terminal renal failure. I. Off dialysis. II. On haemodialysis. III. Effect of heparin. International Journal of Clinical Pharmacology and Biopharmacy 15: 249–254, 255-259, 560-562 (1977).
Vöhringer, H.F. and Rietbrock, N.: Metabolism and excretion of digitoxin in man. Clinical Pharmacology and Therapeutics 16: 796–806 (1974).
Vöhringer, H.F.; Rietbrock, N.; Spurny, P.; Kuhlmann, J.; Hampl, H. and Baethke, R.: Disposition of digitoxin in renal failure. Clinical Pharmacology and Therapeutics 19: 387–395 (1976).
Wagner, J.G.: Loading and maintenance doses of digoxin in patients with normal renal function and those with severely impaired renal function. Journal of Clinical Pharmacology 14: 329–338 (1974).
Wirth, K.E.; Frölich, J.C.; Hollifield, J.W.; Falkner, F.C.; Sweetman, B.S. and Oates, J.A.: Metabolism of digitoxin in man and its modification by spironolactone. European Journal of Clinical Pharmacology 9: 345–354 (1976).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Aronson, J.K. Clinical Pharmacokinetics of Cardiac Glycosides in Patients with Renal Dysfunction. Clin Pharmacokinet 8, 155–178 (1983). https://doi.org/10.2165/00003088-198308020-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003088-198308020-00003