Summary
Synopsis
Lamivudine is a dideoxynucleoside analogue which undergoes intracellular phosphorylation to the putative active metabolite, lamivudine triphosphate. Lamivudine triphosphate prevents HIV replication by competitively inhibiting viral reverse transcriptase. Lamivudine has a unique resistance profile and has the ability to delay resistance to zidovudine and restore zidovudine sensitivity in zidovudine-experienced patients.
Combination antiretroviral drug therapy is now generally considered preferable to monotherapy as first-line treatment for patients with HIV infection. In double-blind trials in antiretroviral drug–experienced or —naive adults, improvements in surrogate markers of disease progression were significantly greater in patients receiving lamivudine plus zidovudine combination therapy than in patients who received either drug as monotherapy. Preliminary results of CAESAR, a large multicentre trial in patients with moderately advanced HIV infection receiving zidovudine-based treatment regimens, show a 54% reduction in the rate of disease progression or death with the addition of lamivudine, compared with the addition of placebo.
Initial virological data from studies of combination regimens including lamivudine and protease inhibitors are also promising, although the longer term efficacy of these regimens remains to be established.
Improvements in surrogate disease markers were also seen in children and adolescents with symptomatic HIV infection who received lamivudine monotherapy. Studies of lamivudine-containing combination therapy in children and adolescents are in progress, but few data have yet been published.
Lamivudine is generally well tolerated as monotherapy or in combination with other antiretroviral agents in HIV- infected adults with CD4+ counts ≥100 cells/µl. Gastrointestinal disturbances were reported as the most common adverse events during lamivudine monotherapy or combination therapy. Lamivudine appears to be less well tolerated in patients with advanced disease (CD4+ cell counts <100 cells/µl ), but more data are required to clarify its tolerability in such patients. Pancreatitis has been reported in children with advanced disease during treatment with the drug, but was not directly attributable to lamivudine therapy.
Thus, lamivudine, administered in combination with zidovudine, is now established as an effective agent for the treatment of antiretroviral drug—experienced or —naive individuals with asymptomatic or symptomatic HIV disease. Moreover, encouraging preliminary data suggest that lamivudine is poised to become an important component of other regimens, in combination with drugs such as the protease inhibitors.
Pharmacodynamic Properties
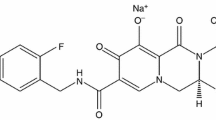
Lamivudine (also known as 3TC) is phosphorylated by intracellular enzymes to form lamivudine triphosphate, the putative active metabolite. Lamivudine triphosphate prevents HIV replication by competitively inhibiting viral reverse transcriptase and terminating proviral DNA chain extension. Its intracellular elimination half-life was between 10.5 and 15.5 hours in HIV-infected cells.
Lamivudine demonstrates good inhibitory activity against HIV-1 and -2 in human peripheral blood lymphocytes (PBLs), monocyte/macrophages, and various tumour cell lines. In addition, synergistic activity against HIV-1 has been observed in vitro with 2-drug combinations of lamivudine with zidovudine, didanosine, stavudine, saquinavir, delavirdine or nevirapine.
Minimal cytotoxicity was observed in PBLs and in a range of cell lines exposed to lamivudine. In addition, there was no evidence of decreased DNA synthesis in PBLs exposed to the drug.
High-level resistance to lamivudine, mediated via a mutation at codon 184 of the HIV pol gene, has emerged rapidly in viral isolates from patients infected with HIV-1 who have received the drug as monotherapy (87% at 12 weeks) or as combination therapy. The lamivudine resistance mutation has led to antagonism of zidovudine resistance and the partial restoration of HIV-1 phenotypic sensitivity to this agent during lamivudine exposure. However, resistance to both lamivudine and zidovudine has occurred in clinical isolates from small numbers of patients who received these agents in combination.
Pharmacokinetic Properties
After oral administration, lamivudine is well absorbed and has good bioavailability (mean absolute bioavailability >80% in adults and 68% in infants and children), although wide interpatient variation in oral bioavailability has been reported.
Lamivudine is distributed into total body fluid and had a mean volume of distribution of 1.3 L/kg in a dose-ranging investigation. It has been shown to distribute into CSF, but the mean CSF: serum ratio was low (0.06) in 6 HIV-infected adults. In children, CSF concentrations of lamivudine increased with increasing oral dosages of the drug. Lamivudine is <36% plasma protein bound. Lamivudine appears to diffuse freely across the placenta from the maternal circulation to the fetal circulation. As yet, data are unavailable on the extent of penetration of the drug into breast milk.
Lamivudine is not significantly metabolised and is eliminated primarily as unchanged drug via the kidneys. In patients with moderate or severe renal impairment, lamivudine area under the serum concentration-time curve (AUC) values increased by 270 and 500%, respectively, compared with values in healthy controls.
Few data are available on interactions between lamivudine and other drugs. However, when lamivudine and cotrimoxazole (trimethoprim-sulfamethoxazole) were coadministered to patients with asymptomatic HIV infection, there was an increase in lamivudine AUC and a decrease in lamivudine renal clearance, probably because of competitive inhibition of lamivudine renal excretion by the trimethoprim component of cotrimoxazole. The pharmacokinetics of cotrimoxazole were unaffected by concomitantly administered lamivudine.
Therapeutic Efficacy
In clinical practice, combination therapy is generally regarded as preferable to monotherapy for the first-line treatment of patients with HIV infection. Beneficial immunological and virological responses were observed in antiretroviral drug-naive and —experienced HIV-infected patients who received lamivudine and zidovudine in combination. Improvements in surrogate markers were greater in recipients of combination therapy than in patients who received either lamivudine or zidovudine as monotherapy.
Preliminary results of a large multicentre trial (the CAESAR trial) have shown that in patients with moderately advanced HIV infection receiving zidovudine-based treatment regimens, the addition of lamivudine produced a 54% lower rate of disease progression or death than the addition of placebo.
Lamivudine has also been investigated in combination with protease inhibitors. In several studies (reported as abstracts), plasma HIV RNA was suppressed to below detectable levels in patients who received the drug in combination with indinavir, ritonavir, nelfinavir or saquinavir.
Early trials with lamivudine monotherapy demonstrated that improvements in surrogate markers of HIV disease (increased CD4+ cell counts and decreased serum HIV RNA and p24 antigen levels) occurred in patients with intermediate or advanced HIV infection. However, there was evidence of declining efficacy over time, which was partly attributed to the emergence of high-level HIV-1 resistance to the drug.
Lamivudine monotherapy (1 to 20 mg/kg/day) improved surrogate disease markers in children and adolescents with HIV infection. Investigations of lamivudine-containing combination regimens in this population are in progress.
Tolerability
Lamivudine is generally well tolerated as monotherapy or combination therapy in HIV-infected adults with CD4+ counts ≥100 cells/µl. Gastrointestinal disturbances were the most common adverse events reported in patients who received the drug as monotherapy or in combination with zidovudine. Neutropenia and anaemia have also been observed in lamivudine recipients, but the incidence of myelosuppression was no greater with lamivudine plus zidovudine combination therapy than with zidovudine monotherapy. Lamivudine was well tolerated by most children and adolescents in a dose-ranging study.
Limited clinical evidence indicates that lamivudine is less well tolerated in patients with advanced HIV infection (CD4+ counts <100 cells/µl), but further data are needed to clarify its tolerability profile in this patient group. Pancreatitis was reported in 14% of children with advanced HIV disease during treatment with the drug but was not directly attributed to lamivudine therapy. All of the children who developed pancreatitis had received prior antiretroviral drug therapy before starting lamivudine treatment.
Dosage and Administration
For adults and adolescents weighing ≥50kg, the recommended dosage of lamivudine is 150mg twice daily. It is recommended that lamivudine is administered in combination with zidovudine. The recommended dosage of the drug for adults weighing <50kg is 2 mg/kg body weight twice daily. Lamivudine clearance decreases with declining renal function and dosage adjustment may be required.
The dosage of lamivudine for infants and children (aged 3 months to 12 years) is 4 mg/kg bodyweight twice daily; this should be reduced to 2 mg/kg twice daily for neonates.
Similar content being viewed by others
References
Soudeyns H, Yao X-J, Gao Q, et al. Anti-human immunodeficiency virus type 1 activity and in vitro toxicity of 2′-deoxy-3′-thiacytidine (BCH-189), a novel heterocyclic nucleoside analog. Antimicrob Agents Chemother 1991 Jul; 35: 1386–90
Chang CN, Skalski V, Zhou JH, et al. Biochemical pharmacology of (+)-2′,3′-dideoxy-3′-thiacytidine and (−)-2′,3′-dideoxy-3′-thiacytidine as antihepatitis B-virus agents. J Biol Chem 1992 Nov 5;267: 22414–20
Shewach DS, Liotta DC, Schinazi RF. Affinity of the antiviral enantiomers of oxathiolane cytosine nucleosides for human 2′-deoxycytidine kinase. Biochem Pharmacol 1993 Apr 6; 45: 1540–3
Cammack N, Rouse P, Marr CLP, et al. Cellular metabolism of (−) enantiomeric 2′-deoxy-3′-thiacytidine. Biochem Pharmacol 1992 May 28; 43: 2059–64
Hart GJ, Orr DC, Penn CR, et al. Effects of (−)-2′-deoxy-3′-thiacytidine (3TC) 5′-triphosphate on human immunodeficiency virus reverse transcriptase and mammalian DNA polymerases alpha, beta, and gamma. Antimicrob Agents Chemother 1992 Aug; 36: 1688–94
Veal GJ, Hoggard PG, Barry MG, et al. Interaction between lamivudine (3TC) and other nucleoside analogues for intra-cellular phosphorylation. AIDS 1996 May; 10: 546–8
Schinazi RF, Chu CK, Peck A, et al. Activities of the four optical isomers of 2′,3′-dideoxy-3′-thiacytidine (BCH-189) against human immunodeficiency virus type 1 in human lymphocytes. Antimicrob Agents Chemother 1992 Mar; 36: 672–6
Coates JAV, Cammack N, Jenkinson HJ, et al. The separated enantiomers of 2′-deoxy-3′-thiacytidine (BCH 189) both inhibit human immunodeficiency virus replication in vitro. Antimicrob Agents Chemother 1992 Jan; 36: 202–5
Coates JAV, Cammack N, Jenkinson HJ, et al. (−)-2′-Deoxy-3′-thiacytidine is a potent, highly selective inhibitor of human immunodeficiency virus type 1 and type 2 replication in vitro. Antimicrob Agents Chemother 1992 Apr; 36: 733–9
Schinazi RF, McMillan A, Cannon D, et al. Selective inhibition of human immunodeficiency viruses by racemates and enantiomers of cis-5-fluoro-l-[2-(hydroxymethyl)-1,3-oxathiolan-5-yl]cytosine. Antimicrob Agents Chemother 1992 Nov; 36: 2423–31
Merrill DP, Moonis M, Chou T-C, et al. Lamivudine or stavudine in two- and three-drug combinations against human immunodeficiency virus type 1 replication in vitro. J Infect Dis 1996 Feb; 173: 355–64
Gao W-Y, Agbaria R, Driscoll JS, et al. Divergent anti-human immunodeficiency virus activity and anabolic phosphorylation of 2′,3′-dideoxynucleoside analogs in resting and activated human cells. J Biol Chem 1994 Apr 29; 269: 12633–8
St Clair-MH, Pennington KN, Rooney J, et al. In vitro comparison of selected triple-drug combinations for suppression of HIV-1 replication: The inter-company collaboration protocol. J Acquired Immune Defic Syndr Hum Retrovirol 1995; 10Suppl. 2: S83–91
Larder BA. Viral resistance and the selection of antiretroviral combinations. J Acquir Immune Defic Syndrom Hum Retrovirol 1995; 10Suppl. 1: S28–33
Johnson VA. Nucleoside reverse transcriptase inhibitors and resistance of human immunodeficiency virus type 1. J Infect Dis 1995; 171Suppl. 2: S140–9
Bridges EG, Dutschman GE, Gullen EA, et al. Favorable interaction of β-L(−) nucleoside analogues with clinically approved anti-HIV nucleoside analogues for the treatment of human immunodeficiency virus. Biochem Pharmacol 1996 Mar 22; 51: 731–6
Mathez D, Schinazi RF, Liotta DC, et al. Infectious amplification of wild-type human immunodeficiency virus from patients’ lymphocytes and modulation by reverse transcriptase inhibitors in vitro. Antimicrob Agents Chemother 1993 Oct; 37: 2206–11
Viner KC, Cammack N, Coates JAV, et al. (−)Enantiomeric 2′-deoxy-3′-thiacytidine in combination with AZT synergistically inhibits clinical isolates of HIV-1 [abstract]. 9th International Conference on AIDS. 1993 Jun 6–11; Berlin, 236
Chong KT, Pagano PJ. Synergistic inhibition of human immunodeficiency type I replication in vitro by two and three-drug combination of delavirdine, lamivudine and zidovudine [abstract]. 11th International Conference on AIDS. 1996 Jul 7–12; Vancouver, 72
Balzarini J, Pelemans H, De Clercq E, et al. Combination of 3TC with non-nucleoside reverse transcriptase inhibitors greatly increases the activity of the inhibitors against human immunodeficiency virus type 1 in cell culture [abstract]. J Acquir Immune Defic Syndrom Hum Retrovirol 1995; 10Suppl. 3: S7–8
Sommadossi JP, Schinazi RF, Chu CK, et al. Comparison of cytotoxicity of the (−)-enantiomer and (+)-enantiomer of 2′,3′-dideoxy-3′-thiacytidine in normal human bone marrow progenitor cells. Biochem Pharmacol 1992 Nov 17; 44: 1921–5
Gray NM, Marr CLP, Penn CR, et al. The intracellular phosphorylation of (−)-2′-deoxy-3′-thiacytidine (3TC) and the incorporation of 3TC 5′-monophosphate into DNA by HIV-1 reverse transcriptase and human DNA polymerase γ. Biochem Pharmacol 1995 Sep 28; 50: 1043–51
Lisignoli G, Facchini A, Cattini L, et al. In vitro toxicity of 2′,3′-dideoxy-3′-thiacytidine (BCH189/3TC), a new synthetic anti-HIV-1 nucleoside. Antiviral Chem Chemother 1992; 3(5): 299–303
Moyle G. Activity and role of lamivudine in the treatment of adults with human immunodeficiency virus type 1 infection: a review. Expert Opin Invest Drug 1996; 5(8): 913–24
Schuurman R, Nijhuis M, van LR, et al. Rapid changes in human immunodeficiency virus type 1 RNA load and appearance of drug-resistant virus populations in persons treated with lamivudine (3TC). J Infect Dis 1995 Jun; 171: 1411–9
Gao Q, Gu Z, Parniak MA, et al. The same mutation that encodes low-level human immunodeficiency virus type 1 resistance to 2′,3′-dideoxyinosine and 2′,3′-dideoxycytidine confers high-level resistance to the (−) enantiomer of 2′,3′-dideoxy-3′-thiacytidine. Antimicrob Agents Chemother 1993 Jun; 37: 1390–2
Schinazi RF, Lloyd RM Jr, Nguyen MH, et al. Characterization of human immunodeficiency viruses resistant to oxathiolanecytosine nucleosides. Antimicrob Agents Chemother 1993 Apr; 37: 875–81
Wainberg MA, Salomon H, Gu Z, et al. Development of HIV-1 resistance to (−)2′-deoxy-3′thiacytidine in patients with AIDS or advanced AIDS-related complex. AIDS 1995 Apr; 9: 351–7
Wainberg MA, Drosopoulos WC, Salomon H, et al. Enhanced fidelity of 3TC-selected mutant HIV-1 reverse transcriptase. Science 1996 Mar 1; 271: 1282–5
Tisdale M, Kemp SD, Parry NR, et al. Rapid in vitro selection of human immunodeficiency virus type 1 resistant to 3′-thiacytidine inhibitors due to a mutation in the YMDD region of reverse transcriptase. Proc Natl Acad Sci USA 1993 Jun 15; 90: 5653–6
Kavlick MF, Shirasaka T, Kojima E, et al. Genotypic and phenotypic characterization of HIV-1 isolated from patients receiving (−)-2′,3′-dideoxy-3′-thiacytidine. Antiviral Res 1995 Oct; 28: 133–46
Harrigan PR, Bloor S, Kinghorn I, et al. Virological response to AZT/3TC combination therapy in AZT-experienced patients (trial NUCB3002) [abstract]. J Acquir Immune Defic Syndrom Hum Retrovirol 1995; 10Suppl. 3: S226–7
Harrigan PR, Kinghorn I, Kohli A, et al. Virological response to AZT/3TC combination therapy in AZT-naive patients (Trial NUCB 3001) [abstract]. J Acquir Immune Defic Syndrom Hum Retrovirol 1995; 10Suppl. 3: S27–28
Kuritzkes DR, Shugarts D, Griffin A, et al. Resistance to lamivudine and zidovudine in a phase II comparative trial of 3TC vs. ZDV vs. 3TC plus ZDV [abstract]. J Acquir Immune Defic Syndrom Hum Retrovirol 1995; 10Suppl. 3: S26
Nijhuis M, de Jong JD, van Leeuwen LR, et al. The rise in HIV-1 RNA load during 3TC/AZT combination therapy is associated with the selection of viruses resistant to both 3TC and AZT [abstract]. J Acquir Immune Defic Syndrom Hum Retrovirol 1995; 10Suppl. 3: 25–6
Staszewski S, Miller V, Rehmet S, et al. Virological and immunological analysis of a triple combination pilot study with loviride, lamivudine and zidovudine in HIV-1-infected patients. AIDS 1996 May; 10: F1–7
Boucher CAB, Schuurman R. Rapid changes in HIV-1 RNA load and appearance of drug-resistant virus populations in persons treated with lamivudine (3TC). Int Antiviral News 1996 Apr; 4: 43–5
Bartlett JA, Benoit SL, Johnson VA, et al. Lamivudine plus zidovudine compared with zalcitabine plus zidovudine in patients with HIV infection. Ann Intern Med 1996; 125(3): 161–72
Staszewski S, Loveday C, Picazo JJ, et al. Safety and efficacy of lamivudine-zidovudine combination therapy in zidovudine-experienced patients: a randomized controlled comparison with zidovudine monotherapy. JAMA 1996 Jul 10; 276: 111–7
Katlama C, Ingrand D, Loveday C, et al. Safety and efficacy of lamivudine-zidovudine combination therapy in antiretroviral-naive patients: a randomized controlled comparison with zidovudine monotherapy. JAMA 1996 Jul 10; 276: 118–25
Eron JJ, Benoit SL, Jemsek J, et al. Treatment with lamivudine, zidovudine, or both in HIV-positive patients with 200 to 500 CD4+ cells per cubic millimeter. N Engl J Med 1995 Dec 21; 333: 1662–9
Moyle GJ. Use of viral resistance patterns to antiretroviral drugs in optimising selection of drug combinations and sequences. Drugs 1996; 52(2): 168–85
Nájera I, Holguín A, Quiñones-Mateu ME, et al. pol Gene quasispecies of human mmunodeficiency virus: mutations associated with drug resistance in virus from patients undergoing no drug therapy. J Virol 1995; 69(1): 23–31
Pluda JM, Cooley TP, Montaner JSG, et al. A phase I/II study of 2′-deoxy-3′-thiacytidine (lamivudine) in patients with advanced human immunodeficiency virus infection. J Infect Dis 1995 Jun; 171: 1438–47
van Leeuwen R, Katlama C, Kitchen V, et al. Evaluation of safety and efficacy of 3TC (lamivudine) in patients with asymptomatic or mildly symptomatic human immunodeficiency virus infection: a phase I/II study. J Infect Dis 1995 May; 171: 1166–71
Dalgleish AG. New drugs for the treatment of HIV infection. Expert Opin Invest Drug 1995; 4(8): 763–9
Goulden MG, Hopewell P, Viner KC, et al. Selection of high-level resistance to both 3TC and AZT [abstract]. J Acquir Immune Defic Syndrom Hum Retrovirol 1995; 10Suppl. 3: S25
Goulden MG, Cammack N, Hopewell PL, et al. Selection in vitro of an HIV-1 variant resistant to both lamivudine (3TC) and zidovudine [letter]. AIDS 1996 Jan; 10: 101–2
Johnson VA, Quinn JB, Benoit SL, et al. Drug resistance and viral load in NUCA 3002: lamivudine (3TC) (high or low dose)/zidovudine (ZDV) combination therapy versus ZDV/dideoxycytidine (DDC) combination therapy in ZDV-experienced (≥ to 24 weeks) patients (CD4 cells 100–300/mm3) [abstract]. 3rd Conference on Retroviruses and Opportunistic Infections. 1996 Jan 28–Feb 3: Washington, DC, 113
Kemp SD, Kohli A, Larder BA. Genotypic characterization of an HIV-1 mutant co-resistant to AZT and 3TC [abstract]. J Acquir Immune Defic Syndrom Hum Retrovirol 1995; 10Suppl. 3: 25
Boucher CAB, Cammack N, Schipper P, et al. High-level resistance to (−)enantiomeric 2′-deoxy-3′-thiacytidine in vitro is due to one amino acid substitution in the catalytic site of human immunodeficiency virus type 1 reverse transcriptase. Antimicrob Agents Chemother 1993 Oct; 37: 2231–4
Larder BA, Kemp SD, Harrigan PR. Potential mechanism for sustained antiretroviral efficacy of AZT-3TC combination therapy. Science 1995 Aug 4; 269: 696–9
Larder BA. The influence of combination therapy on HIV-1 viral load and drug resistance [abstract]. AIDS 1994 Nov; 8Suppl. 4: S4
van Leeuwen R, Lange JM, Hussey EK, et al. The safety and pharmacokinetics of a reverse transcriptase inhibitor, 3TC, in patients with HIV infection: a phase I study. AIDS 1992 Dec; 6: 1471–5
Yuen GJ, Morris DM, Mydlow PK, et al. Pharmacokinetics, absolute bioavailability, and absorption characteristics of lamivudine. J Clin Pharmacol 1995 Dec; 35: 1174–80
Angel JB, Hussey EK, Hall ST, et al. Pharmacokinetics of 3TC (GR109714X) administered with and without food to HIV-infected patients. Drug Invest 1993 Aug; 6: 70–4
Heald AE, Hsyu PH, Yuen GJ, et al. Pharmacokinetics of lamivudine in human immunodeficiency virus-infected patients with renal dysfunction. Antimicrob Agents Chemother 1996 Jun; 40: 1514–9
Moore KHP, Yuen GJ, Raasch RH, et al. Pharmacokinetics of lamivudine administered alone and with trimethoprim-sulfamethoxazole. Clin Pharmacol Ther 1996 May; 59: 550–8
Harker AJ, Evans GL, Hawley AE, et al. High-performance liquid Chromatographic assay for 2′-deoxy- 3′-thiacytidine in human serum. J Chromatogr B Biomed Appl 1994 Jul 1; 657: 227–32
Morris DM, Selinger K. Determination of 2′-deoxy-3′-thiacytidine (3TC) in human urine by liquid chromatography: direct injection with column switching. J Pharm Biomed Anal 1994 Feb; 12: 255–64
Yuen GJ, Benoit S, Rubin M. Population (POP) pharmacokinetics (PK) of lamivudine (3TC) in HIV infected patients: results from two phase III clinical trials [abstract]. Clin Pharmacol Ther 1996 Feb; 59: 144
Johnson MA, Goodwin C, Yuen GJ, et al. The pharmacokinetics of 3TC administered to HIV-1 infected women (pre-partum), during labour and post-partum) and their offspring [abstract]. 11th International Conference on AIDS. 1996 Jul 7–12; Vancouver, 249
Lewis LL, Venzon D, Church J, et al. Lamivudine in children with human immunodeficiency virus infection: a phase I/II study. J Infect Dis 1996 Jul; 174: 16–25
Glaxo Wellcome Inc. Lamivudine Prescribing Information. Research Triangle Park, North Carolina, USA, 1995
Dudley MN, Graham K, Kaul S, et al. Pharmacokinetics of stavudine in patients with AIDS or AIDS-related complex. J Infect Dis 1992; 166: 480–5
Dudley MN. Clinical pharmacokinetics of nucleoside antiretroviral agents. J Infect Dis 1995 Mar; 171Suppl. 2: S99–112
Blaney SM, Daniel MJ, Harker AJ, et al. Pharmacokinetics of lamivudine and BCH-189 in plasma and cerebrospinal fluid of nonhuman primates. Antimicrob Agents Chemother 1995 Dec; 39: 2779–82
Johnson MA, Yuen GI, Daniel MJ, et al. The safety and pharmacokinetics of lamivudine (3TC) in patients with renal impairment, including those on haemodialysis [abstract]. 11th International Conference on AIDS. 1996 Jul 7–12; Vancouver, 111
Rana KZ, Horton CM, Yuen GJ, et al. Effect of lamivudine on zidovudine pharmacokinetics in asymptomatic HIV-infected individuals [abstract]. 34th Int Conf Antimicro Ag Chemother 1994: 83
Horton CM, Yuen G, Mikolich DM, et al. Pharmacokinetics of oral lamivudine administered alone and with oral zidovudine (ZDV) in asymptomatic patients with human immuno-deficiency virus (HIV) infection [abstract]. 95th Annu Meet Am Soc Clin Pharmacol Ther 1994: 198
Phillips AN, Eron JJ, Bartlett JA, et al. HIV-1 RNA levels and the development of clinical disease. AIDS 1996 Jul; 10: 859–65
Lange JMA. Triple combinations: present and future. J Acquir Immune Defic Syndrom Hum Retrovirol 1995; 10Suppl. 1: 77–82
Lange J. Combination antiretroviral therapy; back to the future. Drugs 1995; 49Suppl 1: 32–7 (discussion 38–40)
Vella S. HIV pathogenesis and treatment strategies. J Acquir Immune Defic Syndrom Hum Retrovirol 1995; 10Suppl. 1: S20–3
de Jong MD, Boucher CAB, Galasso GJ, et al. Consensus symposium on combined antiviral therapy. Antiviral Res 1996 Jan; 29: 5–29
Phillips AN, Eron J, Bartlett J, et al. Effect of nucleoside analogue RT inhibitors on plasma HIV RNA and CD4 count as an indicator of clinical effect [abstract]. 11th International Conference on AIDS. 1996 Jul 7–12; Vancouver, 21
Staszewski S, Bartlett I, Eron J, et al. Reductions in HIV-1 disease progression for AZT/3TC relative to control treatments: a meta-analysis [abstract]. AIDS 1996 Nov; 10Suppl. 2
Williams IG, De Cock KM. The XI International Conference on AIDS Vancouver 7–12 July 1996. A review of Clinical Science Track B. Genitourin Med 1996; 72: 365–9
Michelet C, Ruffault A, Arvieux C, et al. 3TC + ZDV in pts with CD4 under 50/mm3: a phase II study [abstract]. 3rd Conference on Retroviruses and Opportunistic Infections. 1996 Jan 28–Feb 3; Washington, DC, 108
Novak RM, Colombo J, Linarez-Diaz J, et al. Comparison of AZT/3TC for the treatment of HIV in persons with CD4 cell counts <300 and prior AZT experience [abstract]. 11th International Conference on AIDS. 1996 July 7–12; Vancouver, 287
Antela A, Casado JL, Pérez-Elías MJ, et al. Efficacy of additive antiretroviral therapy in 135 patients with advanced HIV disease: a 4 year follow-up [abstract]. 11th International Conference on AIDS. 1996 Jul 7–12; Vancouver, 77
Costes O, Lafeuillade A, Pellegrino P, et al. HIV-1 RNA in patients receiving zidovudine + lamivudine after long term zidovudine monotherapy [abstract]. 11th International Conference on AIDS. 1996 Jul 7–12; Vancouver, 75
Jäger H, Virgin G, Pascucci R, et al. Virostatic efficacy of AZT + 3TC in advanced HIV patients with previous exposure to antiretroviral drugs — community based data [abstract]. 11th International Conference on AIDS. 1996 Jul 7–12; Vancouver, 77
Sha BE, Pottage JC Jr, Benson CA, et al. Lamivudine (3TC) therapy for patients with advanced AIDS and <50 CD4 cells [abstract]. 11th International Conference on AIDS. 1996 Jul 7–12; Vancouver, 77
Rouleau D, Conway B, Raboud J, et al. A pilot open label study of the antiviral effect of stavudine (D4T) and lamivudine (3TC) in advanced HIV disease [abstract]. 11th International Conference on AIDS. 1996 July 7–12; Vancouver, 80
Steinhart CR, Jacobsen DGS. Combination antiretroviral therapy with stavudine (D4T) and lamivudine (3TC): a retrospective analysis [abstract]. 11th International Conference on AIDS. 1996 July 7–12; Vancouver, 287
Scott-Lennox J, Burt M. Impact of lamivudine +zidovudine combination therapy on healthy-related quality of life (HRQOL) in people with HIV infection [abstract]. 3rd International Congress on Drug Therapy in HIV infection. 1996 Nov 3–7; Birmingham, P40
Scott-Lennox J, McLaughlin-Miley CJ, Mauskopf JA. Impact of lamivudine and zidovudine therapy on quality of life (QOL) [abstract]. 11th International Conference on AIDS. 1996 Aug 7–12; Vancouver, 286
Saimot AG, Simon F, Landman R, et al. A triple nucleoside analogue combination in four patients with primary HIV-I infections: towards complete virological remissions? [abstract]. 11th International Conference on AIDS. 1996 Jul 7–12; Vancouver, 112
Mathez D, Winter C, Leibowitch I, et al. Triple nucleoside analogue combinations as first or second line treatment against HIV-I in patients with AIDS: preliminary results [abstract]. 11th International Conference on AIDS. 1996 Jul 7–12; Vancouver, 284
Ruiz L, Romeu J, Martínez-Picado J, et al. Efficacy of triple combination therapy with zidovudine (ZDV) plus zalcitabine (ddC) plus lamivudine (3TC) versus double (ZDV+3TC) combination therapy in patients previously treated with ZDV+ddC. AIDS 1996; 10(14): F61–6
Katlama C. Clinical and survival benefit of 3TC in combination with zidovudine -containing regimens in HIV-1 infection: interim results of the CAESAR study [abstract]. 1996 Nov 3–7; Birmingham, S9
Montaner J, Cooper D, Katlama C, et al. CAESAR: Confirmation of the clinical benefit of 3TC (Epivir) in HIV-1 disease: preliminary results. Interscience Conference on Antimicrobial Agents and Chemotherapy. 1996 Sep 15–18; New Orleans, 8
Higgins G. New era of combination therapy for HIV infection. Inpharma 1996 (1048): 3–5
Gulick R, Mellors J, Havlir D, et al. Potent and sustained antiretroviral activity of indinavir (IDV) in combination with zidovudine (ZDV) and lamivudine (3TC) [abstract]. 3rd Conference on Retroviruses and Opportunistic Infections. 1996 Jan 28–Feb 3: 162
Prescott L. Redefining the approach to treating HIV infection. Inpharma 1996 (1052): 13–4
Baruch A, Mastrodonato-Delora P, Schnipper E, et al. Efficacy and safety of triple combination therapy with Invirase (saquinavir/SQV/HIV protease inhibitor), Epivir (3TC/lamivudine) and Retrovir (Rm) (ZDV/zidovudine) in HIV-infected patients [abstract]. 11th International Conference on Aids 1996 Jul 7–12; 18
Hirsch M, Meibohm A, Rawlins S, et al. Indinavir (IDV) in combination with zidovudine (ZDV) and lamivudine (3TC) in ZDV-experienced patients with CD4+ cell counts ≤50 cells/mm3 [abstract]. 4th Conference on Retroviruses amd Opportunistic Infections. 1997 Jan 22–26; Washington, DC
Gulick R, Mellors J, Havlir D, et al. Potent and sustained antiretroviral activity of indinavir (IDV), zidovudine (ZDV) and lamivudine (3TC) [abstract]. 11th International Conference on AIDS. 1996 Jul 7–12; Vancouver
Saget BM, Elbeik T, Guthries J, et al. Dramatic suppression of HIV-I plasma RNA using a combination of zidovudine, didanosine, zalcitabine, epivir, and interferon-alpha in subjects with recent HIV-I infection [abstract]. 11th International Conference on AIDS; 1996 Jul 7–12; Vancouver, 29
Scheibel SF, Saget B, Elbeik T, et al. Extreme suppression of HIV-1 plasma RNA using a combination of zidovudine, didanosine, zalcitabine, epivir, saquinavir, and interferon-alpha in patients with HIV-I infection [abstract]. 11th International Conference on AIDS. 1996 Jul 7–12; Vancouver, 78
Wiewora RJ, Landvay K. Persistence of CD4 lymphocyte increases at 18 months of treatment with lamivudine [abstract]. 11th International Conference on AIDS. 1996 July 7–12; Vancouver, 77
Sölder B, Wintergast U, Gundula N, et al. Effect of combination therapy with ZDV/DDI or ZDV/3TC on plasma HIV-RNA in HIV-infected infants and adolescents [abstract]. 11th International Conference on AIDS. 1996 Jul 7–12; Vancouver, 107
Castelli G, Gibb D, Debré M, et al. Pediatric European Network for treatment of AIDS (Penta) [abstract]. 11th International Conference on AIDS. 1996 Jul 7–12; Vancouver, 318
New drugs for HIV infection. Med Lett Drugs Ther 1996 Apr 12; 38: 35–7
Cupler EJ, Dalakas MC. Exacerbation of peripheral neuropathy by lamivudine. Lancet 1995 Feb 18; 345: 460–1
Styrt BA, Piazza-Hepp TD, Chikami GK. Clinical toxicity of antiretroviral nucleoside analogs. Antiviral Res 1996 Jul; 31: 121–35
Rubin M. New application for lamivudine (EpivirTM) [abstract]. Presented at the FDA Division of Antiviral Drug Products and Antiviral Drugs Advisory Committee Meeting; Nov 6, 1995; Washington, DC
Fong IW. Safety profile of lamivudine (3TC) in patients with advanced HIV-infection [abstract]. 3rd Conference on Retroviruses and Opportunistic Infections. 1996 Jan 28–Feb 3, 77
Centers for Disease Control and Prevention. Case-control study of HIV seroconversion in health-care workers after percutaneous exposure to HIV-infected blood — France, United Kingdom, and United States, Jan 1988–Aug 1994. MMWR 1995; 44: 929–33
Centers for Disease Control and Prevention. Update: Provisional Public Health Service Recommendations for Chemoprophylaxis After Occupational Exposure to HIV. JAMA 1996; 276(2): 90–2
Schinazi RF, Larder BA, Mellors JW, et al. Mutations in retroviral genes associated with drug resistance. Int Antiviral News 1996; 4: 95–107
Carpenter CCJ, Fischl MA, Hammer SM. Antiretroviral therapy for HIV infection in 1996: recommendations of an international panel. JAMA 1996 Jul 10; 276: 146–54
Connor EM, Sperling RS, Gelber R, et al. Reduction of maternal-infant transmission of human immunodeficiency virus type 1 with zidovudine treatment. N Engl J Med 1994; 331: 1173–80
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: D. Back, Department of Pharmacology and Therapeutics, University of Liverpool, Liverpool, England; J.A. Bartlett, Duke University Medical Center, Durham, North Carolina, USA; E. De Clercq, Rega Institute, Katholieke Universiteit Leuven, Leuven, Belgium; M. Floridia, Retrovirus Department, Laboratory of Virology, Istituto Superiore di Sanita, Rome, Italy; A.E. Heald, Division of Infectious Diseases, Duke University Medical Center, Durham, North Carolina, USA; C. Katlama, Service des Maladies Infectieuses et Tropicales, Groupe Hospitalier Pitié-Salpêtrière, Paris, France; L. Naesens, Rega Institute, Katholieke Universiteit Leuven, Leuven, Belgium; R.F. Schinazi, Laboratory of Biochemical Pharmacology, Veterans Affairs Medical Center/Emory University, Decatur, Georgia, USA; S. Vella, Retrovirus Department, Laboratory of Virology, Istituto Superiore di Sanita, Rome, Italy.
Rights and permissions
About this article
Cite this article
Perry, C.M., Faulds, D. Lamivudine. Drugs 53, 657–680 (1997). https://doi.org/10.2165/00003495-199753040-00008
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-199753040-00008