Abstract
Thiazolidinediones (TZDs), including pioglitazone and rosiglitazone, have been prescribed for a number of years as monotherapy or combination therapy for glycemic control of type 2 diabetes mellitus. It has been hypothesized that the clinical advantages offered by TZDs compared with other commonly used oral hypoglycemic agents (OHAs) [i.e. improved glycemic control, improved lipid profiles, and low rates of hypoglycemic events] should lead to improvements in long-term outcomes, such as decreased incidence of micro- and macrovascular disease, leading in turn to improvements in life expectancy and quality-adjusted life expectancy. While the acquisition costs of TZDs are generally higher than other alternatives, such as metformin or sulfonylureas, it has been postulated that the higher initial acquisition costs of the medications should be offset by decreased costs of treating complications. As such, TZDs could represent an efficient form of treatment for type 2 diabetes.
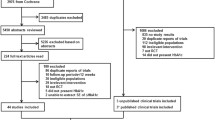
In order to provide an overview of studies performed to date, we have reviewed the available literature on the cost effectiveness of TZDs as a treatment in type 2 diabetes. An extensive literature search of major databases of indexed studies and proceedings of diabetes and health economics-related international conferences was performed to identify studies reporting health-economic outcomes for pioglitazone or rosiglitazone. Very few health-economics studies of TZDs have been published in peer-reviewed journals to date. A total of 16 studies (3 peer-reviewed international journal publications, 13 abstracts) were identified. These studies used various economic-simulation models to estimate the cost effectiveness of rosiglitazone or pioglitazone compared with other commonly prescribed OHAs, such as metformin, sulfonylureas, or acarbose, used either as monotherapy or in combination therapy for the treatment of type 2 diabetes. The studies demonstrated that the short-term clinical advantages of using TZDs translated into decreased incidence and progression of micro- and macrovascular complications, leading to improvements in life expectancy and quality-adjusted life expectancy. The short-term increase in costs due to the higher acquisition prices of the TZDs were partially offset by the long-term avoidance of complication costs. In Japan, pioglitazone was shown to lead to overall cost savings compared with other commonly used OHAs. While bearing in mind the issues of publication bias and other limitations outlined, the cost-effectiveness analyses identified and discussed in this paper lend support to the hypothesis that TZDs can be cost-effective therapies when compared with other commonly prescribed OHAs. Future clinical and health-economics studies must make direct head-to-head comparisons between pioglitazone and rosiglitazone to identify which TZD offers the best value for money. Furthermore, the more recently discovered renoprotective properties of TZDs must be factored into future analyses and are likely to have an important impact on their long-term cost effectiveness.





Similar content being viewed by others
References
Zimmet P, McCarty D. The NIDDM epidemic: global estimates and projections. International Diabetes Federation bulletin 1995; 40: 8–16
King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2025: prevalence, numerical estimates, and projections. Diabetes Care 1998; 21: 1414–31
Powers A. Diabetes mellitus. In: Braunwald E, Anthony SF, Kasper D, et al., editors. Harrison’s principles of internal medicine. 15th ed. New York: McGraw-Hill, 2003: 2109–143
Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med 2003; 348: 383–93
Ovalle F, Ovalle-Berúmen JF. Thiazolidinediones: a review of their benefits and risks [abstract]. South Med J 2002 Oct; 95(10): 1188
Europe approves Actos (Pioglitazone HCI) monotherapy for treatment of type 2 diabetes. DG News. 2003 Sep 5
Detsky AS. Using cost-effectiveness analysis for formulary decision making: from theory into practice. Pharmacoeconomics 1994; 6: 281–8
Weinstein MC, O’Brien B, Hornberger J, et al. Principles of good practice for decision analytic modeling in health-care evaluation: report of the ISPOR Task Force on Good Research Practices. Modeling studies. Value Health 2003; 6: 9–17
Weinstein MC, Siegel JE, Gold MR, et al. Recommendations of the panel on costeffectiveness in health and medicine. JAMA 1996; 276: 1253–8
Canadian Coordinating Office for Health Technology Assessment. Guidelines for economic evaluations of pharmaceuticals: Ottawa (ON): CCOHTA, 1997
National Institute for Clinical Excellence. Guide to the technology appraisal process [online]. Available from URL: http://www.nice.org.uk [Accessed 2004 Sep 1]
Pharmaceutical Benefits Advisory Committee. Guidelines for the pharmaceutical industry on preparation of submissions to the PBAC [online]. Available from URL: http://www.health.gov.au [Accessed 2004 Oct 14]
Palmer AJ, Weiss C, Sendi PP, et al. The cost-effectiveness of different management strategies for type I diabetes: a Swiss perspective. Diabetologia 1999; 43: 13–26
Palmer AJ, Brandt A, Gozzoli V, et al. Outline of a diabetes disease management model: principles and applications. Diabetes Res Clin Pract 2000; 50 Suppl. 3: S47–56
Coyle D, Palmer AJ, Tam R. Economic evaluation of pioglitazone hydrochloride in the management of type 2 diabetes mellitus in Canada. Pharmacoeconomics 2003; 20: 31–42
Henriksson F. Applications of economic models in healthcare: the introduction of pioglitazone in Sweden. Pharmacoeconomics 2002; 20 Suppl. 1: 43–53
Maniadakis N, Kielhorn A, Thomander L, et al. The impact and outcomes of a new oral diabetes drug pioglitazone (Actos®, Takeda) in the management of type-2 diabetes in Sweden [abstract]. Value Health 2003; 4: 504
Maniadakis N, Kielhorn A, Jansen R, et al. The impact and outcomes of a new oral diabetes drug pioglitazone (Actos®, Takeda) in the management of type 2 diabetes in Norway [abstract]. Value Health 2003; 4: 506
Maniadakis N, Kielhorn A, Heikkinen K, et al. The outcomes of long-term treatment of a new oral diabetes drug pioglitazone (Actos®, Takeda) in the management of type 2 diabetes [abstract]. Value Health 2001; 4: 502
Palmer AJ, Weiss C, Roze S, et al. Cost-effectiveness of pioglitazone versus acarbose, metformin, and sulphonylureas in the United Kingdom [abstract]. Diabetes Res Clin Pract 2000; 50: S193
Palmer AJ, Weiss C, Roze S, et al. Cost-effectiveness of adding either pioglitazone or acarbose to metformin in the United Kingdom. Diabetes Res Clin Pract 2000; 50: S193
Maniadakis N, Sacristan J, Reviriego J, et al. An economic evaluation of combination therapy with pioglitazone (Actos®, Takeda) in type 2 diabetes mellitus from a Spanish health-care perspective [abstract]. Value Health 2001; 4: 503
Jansen R, Clausen JO, Maniadakis N, et al. An assessment of the cost-effectiveness of pioglitazone (Actos®, Takeda) in type 2 diabetes mellitus in Denmark. Value Health 2003; 4: 507–8
Ikeda S, Kobayashi M. Development of a simulation model for clinical and economic consequences of Type II diabetes in Japan [abstract]. Diabetologia 2003; 46: 1332
Beale S, Bagust A, Richter A, et al. A cost-effectiveness evaluation of adding rosiglitazone versus sulphonylurea to metformin in a US obese Type 2 diabetes population [abstract]. Diabetologia 2003; 46: A444
Bagust A, Shearer A, Schoeffski O, et al. Cost-effectiveness in Germany of rosiglitazone-metformin combination in Type 2 diabetes [abstract]. Diabetologia 2003; 46: A444
Richter A, Thieda P, Bagust A, et al. The cost-effectiveness of adding rosiglitazone versus sulfonylurea to metformin in a us obese type 2 diabetes population [abstract]. Diabetes 2003; 52: A254
Nicklasson L, Palmer AJ, Roze S. Simulating the long term cost-effectiveness of a comibnation regimen of repaglinide plug rosiglitazone vs. rosiglitazone monotherapy over a 30-year period [abstract]. Value Health 2003; 6: 334
Pi O, Lg S. Cost-effectiveness and cardiovascular risk: an analysis of rosiglitazone compared with other oral hypoglycemic agents in the treatment of type two diabetes mellitus [abstract]. Value Health 2003; 4: 111
Ramsdell JW, Braunstein SN, Stephens JM, et al. Economic model of first-line drug strategies to achieve recommended glycaemic control in newly diagnosed type 2 diabetes mellitus. Pharmacoeconomics 2003; 21: 819–37
Bagust A, Hopkinson PK, Maier W, et al. An economic model of the long-term health care burden of Type II diabetes. Diabetologia 2001; 44: 2140–55
Palmer AJ, Roze S, Foos V, et al. The CORE diabetes model: projecting long term clinical outcomes, costs and cost-effectiveness of interventions in diabetes mellitus (types 1 and 2) to support clinical and reimbursement decision making. Curr Med Res Opin 2004; 20 Suppl. 1: s5–s26
Palmer AJ, Roze S, Foos V, et al. Validation of the CORE Diabetes Model. Curr Med Res Opin 2004; 20 Suppl. 1: s27–40
Valentine W, Lammert M, Lurati F, et al. Overview of the CORE Diabetes Model [abstract]. Diabetologia 2003; 46: A275–6
Friedberg M, Saffran B, Stinson TJ, et al. Evaluation of conflict of interest in economic analyses of new drugs used in oncology. JAMA 1999; 282: 1453–7
Sacristan JA, Bolanos E, Hernandez JM, et al. Publication bias in health economic studies. Pharmacoeconomics 1997; 11: 289–92
Rakatansky H. Sources of bias in the economic analysis of new drugs [letter]. JAMA 2000; 283: 1424
Prendergast MM. Sources of bias in the economic analysis of new drugs [letter]. JAMA 2000; 283: 1424
Le Pen C. Sources of bias in the economic analysis of new drugs. JAMA 2000; 283: 1423–4
Gagnon JP. Sources of bias in the economic analysis of new drugs. Health Outcomes Committee Pharmaceutical Research and Manufacturers of America, Washington, DC [letter]. JAMA 2000; 283: 1423
Krimsky S. Conflict of interest and cost-effectiveness analysis. JAMA 1999; 282: 1474–5
Caro JJ, Klittich WS, Raggio G, et al. Economic assessment of troglitazone as an adjunct to sulfonylurea therapy in the treatment of type 2 diabetes. Clin Ther 2000; 22: 116–27
Coyle D, Lee KM, O’Brien BJ. The role of models within economic analysis: focus on type 2 diabetes mellitus. Pharmacoeconomics 2002; 20 Suppl. 1: 11–9
Eddy DM, Schlessinger L. Archimedes: a trial-validated model of diabetes. Diabetes Care 2003; 26: 3093–101
CDC Diabetes Cost-effectiveness Group. Cost-effectiveness of intensive glycemic control, intensified hypertension control, and serum cholesterol level reduction for type 2 diabetes. JAMA 2002; 287: 2542–51
Caro JJ, Klittich WS, Raggio G, et al. Economic assessment of troglitazone as an adjunct to sulfonylurea therapy in the treatment of type 2 diabetes. Clin Ther 2000; 22: 116–27
Brown JB, Russell A, Chan W, et al. The global diabetes model: user friendly version 3.0. Diabetes Res Clin Pract 2000; 50 Suppl. 3: S15–46
Buchanan TA, Meehan WP, Jeng YY, et al. Blood pressure lowering by pioglitazone: evidence for a direct vascular effect. J Clin Invest 1995; 96: 354–60
Kaufman LN, Peterson MM, DeGrange LM. Pioglitazone attenuates diet-induced hypertension in rats. Metabolism 1995; 44: 1105–9
Buckingham RE, Al Barazanji KA, Toseland CD, et al. Peroxisome proliferatoractivated receptor-gamma agonist, rosiglitazone, protects against nephropathy and pancreatic islet abnormalities in Zucker fatty rats. Diabetes 1998; 47: 1326–34
Nakamura T, Ushiyama C, Osada S, et al. Pioglitazone reduces urinary podocyte excretion in type 2 diabetes patients with microalbuminuria. Metabolism 2001; 50: 1193–6
Bakris G, Viberti G, Weston WM, et al. Rosiglitazone reduces urinary albumin excretion in type II diabetes. J Hum Hypertens 2003; 17: 7–12
Rodby RA, Firth LM, Lewis EJ. An economic analysis of Captopril in the treatment of diabetic nephropathy. The Collaborative Study Group. Diabetes Care 1996; 19: 1051–61
Rodby RA, Chiou CF, Borenstein J, et al. The cost-effectiveness of irbesartan in the treatment of hypertensive patients with type 2 diabetic nephropathy. Clin Ther 2003; 25: 2103–19
Palmer AJ, Annemans L, Roze S, et al. An economic evaluation of irbesartan in the treatment of patients with type 2 diabetes, hypertension and nephropathy; costeffectiveness of Irbesartan in Diabetic Nephropathy Trial (IDNT) in the Belgian, and French settings. Nephral Dial Transplant 2003; 18: 2059–66
Data on file, CORE, Palmer AJ, 2004
Acknowledgments
The authors have not received any funding for the preparation of this manuscript. All the authors are employed by CORE Center for Outcomes Research, which has received unrestricted research funding from Eli Lilly, Novo Nordisk, and Merck-Santé.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Palmer, A.J., Valentine, W.J. & Ray, J.A. Thiazolidinediones for Diabetes Mellitus. Dis-Manage-Health-Outcomes 12, 363–375 (2004). https://doi.org/10.2165/00115677-200412060-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00115677-200412060-00003