Abstract
The reliability and relevance of any analytical toxicology result is determined in the first instance by the nature and integrity of the specimen(s) submitted for analysis. This article provides guidelines for sample collection, labelling, transport and storage, especially regarding specimens obtained during a postmortem examination. Blood (5mL) should be taken from two distinct peripheral sites, preferably left and right femoral veins, taking care not to draw blood from more central vessels. Urine (if available), vitreous humour (separate samples from each eye), a representative portion of stomach contents, and liver (10–20g, right lobe) are amongst other important specimens. A preservative (sodium fluoride, 0.5–2% weight by volume (w/v) should be added to a portion of the blood sample/the sample from one vein, and to urine. Leave a small ( 10–20% headspace) in tubes containing liquids if they are likely to be frozen. Precautions to minimise the possibility of cross-contamination of biological specimens must be taken, especially if volatile poison(s) may be involved. If death occurred in hospital, any residual antemortem samples should be sought as a matter of urgency. Hair/nail collection should be considered if chronic exposure is suspected, for example, in deaths possibly related to drug abuse. A lock of hair the width of a pen tied at the root end is required for a comprehensive drug screen. The value of providing as full a clinical/occupational/circumstantial history as possible together with a copy of the postmortem report (when available) and of implementing chain-of-custody procedures when submitting samples for analysis cannot be over-emphasised.
Similar content being viewed by others
1. Background
These guidelines aim to assist in the collection, labelling, storage and transport of specimens of body fluids and tissues for toxicological analysis, particularly when taken postmortem (table I and table II). There is rarely an opportunity to collect further specimens once a postmortem examination has been concluded and in clinical cases the situation often changes with time, possibly rendering later samples less useful. Many analytical toxicology procedures require collection of blood, urine, stomach contents and ‘scene residues’. Samples of other appropriate fluids and tissues should also be collected as detailed in the points below, but may not be required for analysis unless special investigations are required or decomposition is advanced.[1,2] However, all samples should be retained (at 4°C or -20°C) in case they are needed. Hair and nail samples should be stored at room temperature.
In order to maximise the reliability of measurements performed in postmortem blood, it is recommended that:
-
1.
The interval between death and the postmortem examination is minimised.
-
2.
The body/samples are stored at a maximum of 4°C before the examination and after collection, respectively.
-
3.
That blood is collected from peripheral site(s), usually the femoral vein(s), that have been suitably isolated.
-
4.
A preservative (sodium fluoride) is added to a portion of the blood sample or the sample from one vein, and to urine and vitreous humour.
These general recommendations are discussed in more detail in section 2. Special care is required in the collection and storage of specimens for the analysis of volatile or unstable compounds. It is usually advisable to contact the laboratory by telephone in advance to discuss urgent or complicated cases.
The value of providing as full a clinical/occupational/circumstantial history as possible together with a copy of the postmortem report (when available) when submitting samples for analysis cannot be over-emphasised. Not only might this help target the analysis to likely poisons, but also interpretation of any analytical results may be greatly simplified.[3]
2. Sample Collection and Preservation
Samples should be labelled with the full name of the deceased, sample type and site of collection, and date and time of collection. A postmortem (reference) number may also be appropriate. In the case of blood specimens, the specific site of sampling should always be stated. All organs/tissue samples should be placed in separate containers to remove any chance of cross-contamination.
Some laboratories provide appropriate specimen containers for the collection of postmortem blood and urine specimens. Suitable packaging for sending specimens by post may also be supplied. The use of disposable hard plastic or glass tubes is recommended. If these are not available, use containers with secure closures appropriate to the specimen volumes. The use of blood tubes containing gel separators may lead to contamination of the sample with plasticisers and volatiles, and analytes may be lost by diffusion into the gel. Do not use lithium heparin tubes if lithium poisoning is a possibility. Do not use citrated tubes as these will dilute the blood and may render some analytical methods inaccurate.
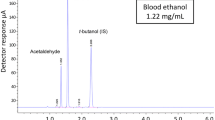
No preservative other than sodium fluoride/oxalate should be used. Ideally sodium fluoride up to a concentration of 2% weight by volume (w/v) should be added, i.e. 20 mg/mL; note that this is substantially more than that contained in a fluoride/oxalate tube of the type used for blood glucose measurement. Fluoride-containing tubes specifically designed for forensic work are available in the UK and in some other countries, but have to be ordered specially. Addition of fluoride helps minimise fermentation, hence production of ethanol in vitro and helps protect other labile drugs such as clonazepam, cocaine and nitrazepam from degradation. However, the retention, if possible, of an additional unpreserved blood sample is advisable.
All specimens should be stored at a maximum of 4°C before transport to the laboratory. Each specimen bottle should be securely sealed to prevent leakage, and individually packaged in separate plastic bags. Particular attention should be paid to the packaging of samples to be transported by post or courier in order to comply with health and safety regulations. Leave a small (10–20%) head-space in tubes containing liquids if they are likely to be frozen. Use waterproof labelling.
Sample volumes/amounts smaller than those indicated in table II are often sufficient to complete the analyses required. Submission of very small samples may, however, result in reduced sensitivity and scope of the analyses undertaken, but nevertheless such samples should always be forwarded to the laboratory. Any residual specimen should be kept at the laboratory and stored at or below -20°C until investigation of the incident is concluded.
If death occurred in hospital, residual antemortem specimens of blood, plasma/serum, or urine should be obtained as a matter of urgency from the hospital pathology laboratory and submitted for toxicological analysis in addition to postmortem specimens. It may be important to note if urine was obtained by use of a catheter lubricated with lidocaine (lignocaine) gel and to record any drugs administered during emergency or investigational procedures.
More detailed guidelines for use when performing postmortem examinations on victims of transport or other accidents are available.[4] When investigating incidents in which several people have died, it is especially important to carefully identify and label accordingly all specimens as they are collected. If a specimen cannot be attributed to a specific individual, this must be recorded.
Collection of specimens for toxicological investigation does not override the need to perform histological or biochemical investigations concurrently in certain circumstances. Histological examination of the myocardium is necessary in order to exclude myocarditis due to chronic exposure to clozapine or cocaine, for example, as a cause of death.
2.1 Blood
2.1.1 Blood (for Quantitative Work)
Blood (at least 5mL) should be taken by aspiration using a hypodermic needle and syringe from two distinct peripheral sites, preferably left and right femoral veins, taking care not to draw blood from more central vessels. This is best achieved by tying or cutting the vessel proximally to the point of sampling. Massaging of tissue around the vessel (‘milking’) during sampling should be minimised and, if possible, avoided — it is better to dissect out the vein beforehand if blood cannot otherwise be obtained. The precise sampling site must be recorded on the sample tube. If sufficient sample is obtained, this should be divided between unpreserved and preserved (fluoride) tubes, otherwise the entire sample should be preserved unless there is a possibility of poisoning with fluoride or compounds giving rise to fluoride in vivo such as fluoroacetate. If only heart or cavity blood is available, this should be clearly stated.
2.1.2 Blood (for Qualitative Analysis)
Blood (approximately 10–30mL) should be taken from the heart (preferably right atrium), inferior vena cava, or another convenient large vessel. The precise sampling site must be recorded on the sample tube.
2.2 Urine
If possible, 2 x 25mL urine samples should be submitted in sterile plastic container(s), one unpreserved and one with preservative (fluoride). If only a small amount is available, all should be preserved (but see note on fluoride poisoning above) in a 5mL glass tube that either has fluoride as an integral preservative or to which suitable fluoride preparations are added. Boric acid or thiomersal containers should NOT be used. Urine specimens collected postmortem are valuable in screening for an unknown drug or poison, particularly illicit drugs and steroids. Urine specimens are also used in the quantitative analysis of alcohol if there may be uncertainty over the reliability of a blood result.
2.3 Stomach Contents
One representative portion (approximately 50mL) without preservative should be submitted. This sample is especially useful if poisons such as drugs or cyanide salts have been taken orally as the amounts present may be many times higher than in other fluids. The sample should be clearly labelled to indicate that it is only a portion of the contents.
The entire stomach contents should be retained. If distinct tablets or capsules are observed, these should be placed in individual hard plastic or glass containers. Identification of such material by reference to a computerised database of pharmaceutical products can sometimes be useful.[5] It can also be helpful to measure the amount of drug present in the stomach if the blood concentration is difficult to interpret, hence it is important to record the total amount of stomach contents. Note that great care is needed if cyanide salts or phosphides such as aluminium phosphide have been ingested, especially on an empty stomach, since highly toxic hydrogen cyanide or phosphine gas will be released because of a reaction with stomach acid. Also, the presence of these and other volatile materials can lead to cross-contamination of other biological specimens unless due precautions are taken.
2.4 Vitreous Humour
Vitreous humour, which occurs behind the lens of the eye, can sometimes be obtained even if a corpse has been extensively burnt or damaged, if putrefaction is beginning to occur, or if samples such as urine are not available. This specimen may be especially useful when investigating deaths related to diabetes mellitus or insulin, and for the analysis of alcohols, digoxin, lithium and many psychotropic drugs. Vitreous humour is essentially a salt solution with very little protein, hence drugs present can be extracted as though they were solutions in a buffer. Samples should be collected from each eye separately, and sodium fluoride preservative (2% w/v) added. Care must be taken during sampling because use of excessive suction can cause a significant change in the concentration of several analytes.[1,6] The possibility of concurrent vitreous disease must also be considered.[7]
2.5 Liver
Liver is easily collected and can be readily homogenised. It may contain large amounts of drugs and metabolites, and may be the primary specimen submitted for analysis if blood is not available. Unfixed, wet tissue (10–20g) should be collected. If possible, the sample should be taken from the right lobe as this should not be contaminated with bile and diffusion of poison from the stomach is less likely than in the left lobe.[8,9] The sample should be clearly labelled to indicate the lobe of origin. An analysis may in some cases help establish whether acute or chronic exposure has occurred, but sometimes the analysis can do little more than establish exposure in the absence of reliable information to aid in the interpretation of quantitative results.
2.6 Bile
Bile (approximately 10mL) should be collected from the gall bladder and sodium fluoride preservative (2% w/v) added. This fluid may contain high concentrations of many dugs and metabolites, hence it is important to minimise the risk of cross-contamination. Also, fermentation may occur after sample collection, hence storage at -20°C or below is recommended even if fluoride has been added.
2.7 Other Tissues
Other tissue samples may be useful when investigating deaths where volatile substances such as solvents or gases are implicated. Brain, subcutaneous fat, lung (apex) and kidney are the most useful; 10–20g wet unfixed tissue should be collected into separate glass containers. The specimen should be placed in a glass specimen jar or nylon bag (volatile substance abuse-related deaths) and deep-frozen prior to transport to the laboratory. Measurement of brain concentrations of certain drugs and poisons, especially volatiles, may also be useful in certain circumstances. Measurement of brain cocaine concentrations has been said to be useful when investigating possible cocaine-related deaths, but there is no clear rationale for this. On the other hand, striated muscle, notably muscle obtained in close proximity to the femoral vessel, can be useful if decomposition is advanced and may allow limited interpretation of quantitative data with drugs such as morphine. Muscle from both legs should be obtained to minimise the risk of a sample being taken close to an injection site.
2.8 Hair and Nail
Drugs and other poisons sequestered in hair and nail are not metabolised further. These samples may be useful: (i) if long-term or episodic exposure to toxic metals, such as arsenic or lead is suspected; (ii) in deaths related to drug abuse (particularly opiates and methadone) where establishing prior drug use may be very important; and (iii) for poisons that may have been eliminated from other commonly sampled fluids/tissues before death. Even lidocaine, a common adulterant in illicit heroin and cocaine, can be monitored in hair.[10] Hair analysis can sometimes help distinguish between episodic or continuous exposure. Head hair (approximate rate of growth 1 cm/month) can give information on exposure weeks to months prior to collection, whereas specimens such as blood and urine will only provide evidence of short-term exposure (to, at most, a few days beforehand). Acidic/neutral drugs/metabolites such as cannabis are generally more difficult to detect than basic drugs. Hair colour can affect the reliability of results.[11] White/grey (grizzled) hair has poor drug incorporation and retention characteristics. In addition, chemical treatment (colouring, perming, dying) may result in significant loss of analyte; any available information on such treatment should be provided to the laboratory.
Head hair should be plucked by the root, and laid aligned in aluminium foil. Pubic hair may be substituted if no head hair remains, or if the head hair has been excessively bleached or permed. If hair specimens are cut from the head, the proximal end should be clearly identified, e.g. by tying with a piece of thread. A lock of hair approximately equivalent to the width of a pen is required for a complete drug screen and this should be obtained prior to the skull being opened.
Whole nails should be lifted from the fingers or toes. This provides an even longer potential window for detecting exposure than hair. However, relatively little is known about the mechanisms of uptake and retention of drugs and metabolites in nail, so interpretation is more difficult.[12]
Hair analysis has its drawbacks. Interpretation of results is based on knowledge of: (i) the anatomy, physiology and biochemistry of growing hair; (ii) of the pharmacokinetics and metabolism of the compound in question; and (iii) of the factors influencing the incorporation, storage, and removal of drugs and other poisons from hair. Surface contamination is likely, although deliberate adulteration of the specimen is unlikely.[13,14] Analytical procedures can minimise the risk of surface contamination whilst the presence of metabolites (notably cocaethylene) can be used to establish that a positive finding is the result of systemic exposure. On the other hand, sample preparation is currently labour-intensive and no adequate control material is available.[6]
There are differences in hair growth rate depending on anatomical region, age, sex, ethnicity and inter-individual variability, hence interpretation of parent drug or/and metabolite concentrations in hair is not straightforward.[15] An exact value for a dose of a particular poison or an exact time of exposure is impossible. Cosmetic treatment, natural and artificial hair colour, differences in hair structure, and the selectivity of the analytical methods used may all influence the results obtained (table III).
2.9 Bone and Bone Marrow
Bone may be useful if chronic poisoning by arsenic or lead, for example, is suspected. Bone marrow may be useful in poison identification in cases where all soft tissue has degenerated. For nortriptyline, a bone marrow : blood ratio of 30 has been demonstrated experimentally after 5 days of nortriptyline treatment.[16]
2.10 Nasal Swabs
Intranasal samples using cotton-tipped swabs are sometimes collected in an attempt to detect drug administration by this route, but normally have no particular value.
2.11 Injection Sites
Possible injection sites should be packed individually and labelled with the site of origin. Appropriate ‘control’ material (i.e. from a site thought to not be an injection site) of similar composition should be supplied separately. It is important that muscle tissue around the site is collected, and not just the skin and fatty layer beneath the skin.
2.12 ‘Scene Residues’
All items (e.g. tablets, powders, syringes and infusion fluids) should be labelled and packed with care. These samples must be kept entirely separate from any biological specimens at all times. The danger of cross-contamination is of course greatest with solvents and other volatile materials. Scene residues may be particularly valuable in deaths involving medical, dental, veterinary or nursing personnel who may have access to agents that are difficult to detect once they have entered the body. Investigation of deaths occurring during or shortly after anaesthesia should include the analysis of the anaesthetic(s) used, including inhalational anaesthetics, in order to exclude an administration error. Needles must be packaged within a suitable shield to minimise the risk of injury to laboratory staff.
3. Transport of Specimens
Each specimen must be individually packaged and placed into a polyethylene bag with a tamper-evident seal. Heat sealing can also be used for this purpose. Glass containers should be used with caution (do not overfill) if the specimen is to be stored at -20°C.
Specimens must be individually labelled with the contents, decedent’s name, and pathologist/autopsy number and date of collection. Indelible felt-tipped pens are very useful for this purpose. Care must be taken to avoid contamination of the specimens with solvents, alcohol, disinfectants or deodorants. Formalin, embalming fluids, etc., cause interference with toxicological analyses and should be avoided.
Most specimens, particularly blood and urine, may be sent by post if securely packaged in compliance with post office regulations. However, if legal action is likely to be taken on the basis of the results, it is important to be able to guarantee the identity and integrity of the specimen from collection through to reporting results. Thus, such samples should be protected during transport by the use of tamper-evident seals and should ideally be submitted in person to the laboratory by the coroner’s officer or other investigating personnel.
4. Documentation
Information provided with the samples and designed to help the laboratory in planning the analysis and reporting the result should include:
-
Name, address and telephone number of clinician/pathologist and/or coroner’s officer, and address to which the report and invoice are to be sent. A postmortem (reference) number may also be appropriate.
-
Circumstances of incident and details of drugs thought to be implicated.
-
Past medical history, including current or recent prescription medication, and details of whether the patient experienced any serious potentially infectious disease such as hepatitis, tuberculosis or human immunodeficiency virus.
-
Information on the likely cause and estimated time of ingestion/death and the nature and quantity of any substance(s) implicated.
-
If death occurred in hospital, a summary of the relevant hospital notes should be supplied to include details of emergency treatment and drugs given, including drugs given incidentally during investigative procedures.
-
A copy of any preliminary pathology report, if available.
An example of a form designed to accompany specimens to the laboratory is provided in figure 1. This form should be completed and submitted to the laboratory together with the samples for analysis. A copy of the postmortem report should be submitted as soon as it is available and a copy of any police sudden death report may also be useful. The information requested on this form is ESSENTIAL for the proper conduct of the analysis, and could save valuable time and expense. The circumstances leading to the incident and any additional relevant information should be recorded on a separate sheet. Further examples of such forms are available.[17–19]
‘Chain of custody’ is a term used to refer to the process used to maintain and document the history of the specimen. The chain-of-custody documents should include:
-
the name of the individual collecting the specimen;
-
each person or entity subsequently having custody of it;
-
the date the specimen was collected or transferred;
-
employer or agency;
-
specimen number;
-
the name of the deceased;
-
a brief description of the specimen.
Samples collected for clinical purposes (or even for the coroner) are often not of ‘evidential’ quality, but such samples may be all that is available. If appropriate, DNA testing may be used to establish the origin of samples where there is concern over sample identity.
5. Conclusions
Great advances that have been made regarding the methodology for analytical toxicology, laboratory accreditation, the training and certification of analytical toxicology laboratory staff, and in the knowledge of factors influencing the interpretation of analytical results. Nevertheless, sample collection, especially postmortem sample collection, often remains problematic. The laboratory can do nothing unless the clinician, pathologist, or other person suspects poisoning and collects specimens for analysis. Thereafter, even the most careful analytical work can be negated if sample collection, labelling, transport or storage has been inappropriate. Adequate written procedures must be in place and appropriate training provided to ensure that these pre-analytical phases of the investigation of suspected poisoning are performed to the required standard.
References
Forrest ARW. Obtaining samples at post-mortem examination for toxicological and biochemical analysis. J Clin Pathol 1993; 46: 292–6
Drummer OH, Odell M. Specimens and specimen collection procedures. In: The forensic pharmacology of drugs of abuse. London: Arnold, 2001: 9–16
Flanagan RJ, Connally G. Interpretation of analytical toxicology results in life and at postmortem. Toxicol Rev 2005; 24: 51–62
Office of the Armed Forces Medical Examiner, Armed Forces Institute of Pathology. Guidelines for the collection and shipment of specimens for toxicological analysis, December 2004 [online]. Available from URL: http://www.afip.org/Departments/oafme/tox/contents.html [Accessed 2005 May 19]
Ramsey JD. Solid dosage form identification. In: Moffat AC, Osselton MD, Widdop B, editors. Clarke’s isolation and identification of drugs. 3rd ed. London: Pharmaceutical Press, 2004: 249–58
Richardson T. Pitfalls in forensic toxicology. Ann Clin Biochem 2000; 37: 20–44
Parsons MA, Start RD, Forrest AR. Concurrent vitreous disease may produce abnormal vitreous humour biochemistry and toxicology [letter]. J Clin Pathol 2003; 56: 720
Pounder DJ, Adams E, Fuke C, et al. Site to site variability of postmortem drug concentrations in liver and lung. J Forensic Sci 1996; 41: 927–32
Pounder DJ, Fuke C, Cox DE, et al. Postmortem diffusion of drugs from gastric residue: an experimental study. Am J Forensic Med Pathol 1996; 17: 1–7
Sporkert F, Pragst F. Determination of lidocaine in hair of drug fatalities by headspace solid-phase microextraction. J Anal Toxicol 2000; 24: 316–22
Kelly RC, Mieczkowski T, Sweeney SA, et al. Hair analysis for drugs of abuse: hair color and race differentials or systematic differences in drug preferences? Forensic Sci Int 2000; 107: 63–86
Drummer OH, Gerostamoulos J. Postmortem drug analysis: analytical and toxicological aspects. Ther Drug Monit 2002; 24: 199–209
Baumgartner WA, Hill VA, Blahd WH. Hair analysis for drugs of abuse. J Forensic Sci 1989; 34: 1433–53
Harkey MR, Henderson GC, Zhou C. Simultaneous quantitation of cocaine and its major metabolites in human hair by gas Chromatography/chemical ionization mass spectrometry. J Anal Toxicol 1991; 15: 260–5
Wennig R. Potential problems with the interpretation of hair analysis results. Forensic Sci Int 2000; 107: 5–12
Winek CL, Morris EM, Wahba WW. The use of bone marrow in the study of postmortem redistribution of nortriptyline. J Anal Toxicol 1993; 17: 93–8
Jones G. Postmortem toxicology. In: Moffat AC, Osselton MD, Widdop B, editors. Clarke’s isolation and identification of drugs. 3rd ed. London: Pharmaceutical Press, 2004: 94–108
Moffat AC, Osselton MD, Widdop B. Forensic toxicology. In: Moffat AC, Osselton MD, Widdop B, editors. Clarke’s isolation and identification of drugs. 3rd ed. London: Pharmaceutical Press, 2004: 80–93
Uges D. Hospital toxicology. In: Moffat AC, Osselton MD, Widdop B, editors. Clarke’s isolation and identification of drugs. 3rd ed. London: Pharmaceutical Press, 2004: 3–36
Acknowledgements
No sources of funding were used to assist in the preparation of this review. The author has no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Flanagan, R.J., Connally, G. & Evans, J.M. Analytical Toxicology. Toxicol Rev 24, 63–71 (2005). https://doi.org/10.2165/00139709-200524010-00005
Published:
Issue Date:
DOI: https://doi.org/10.2165/00139709-200524010-00005