Abstract
Background: Armodafinil (Nuvigil®, Cephalon, Inc., Frazer, PA, USA), the longer-lasting isomer of racemic modafinil, is a nonamphetamine, wakefulnesspromoting medication. In patients with excessive sleepiness associated with shift work disorder, treated obstructive sleep apnoea, or narcolepsy, armodafinil has been found to improve wakefulness throughout the shift or day. In addition, while not approved for this indication, armodafinil has been found to improve excessive sleepiness associated with jet-lag disorder.
Objective: This study evaluated systemic exposure to armodafinil and its two major circulating metabolites, R-modafinil acid and modafinil sulfone, and assessed the tolerability profile of armodafinil in elderly and young subjects.
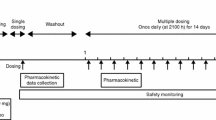
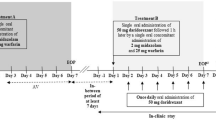
Methods: The pharmacokinetics and tolerability of armodafinil were assessed in an open-label, multiple-dose, parallel-group study in two groups (n = 25 in each group) of healthy men (elderly group aged ≥65 years and young group aged 18–45 years) who received armodafinil 50 mg on day 1, 100 mg on day 2 and 150 mg once daily on days 3 through 7. Plasma concentrations of armodafinil and its metabolites were quantified over 72 hours following the last dose on day 7. Pharmacokinetic parameters, including area under the plasma drug concentration-versus-time curve during a dosing interval (AUCτ) and maximum observed plasma drug concentration (Cmax), and tolerability were assessed.
Results: All 50 subjects enrolled in the study were evaluable for tolerability and 49 were included in the pharmacokinetic analysis. One elderly subject was excluded from the pharmacokinetic analyses because of apparent noncompliance with armodafinil dosing. Systemic exposure following administration of armodafinil, as measured by steady-state AUCτ and Cmax values, was approximately 15% greater in elderly subjects compared with young subjects. Geometric mean ratios for AUCτ and Cmax in the two groups were 1.14 (95% CI 1.03, 1.25; p = 0.0086) and 1.15 (95% CI 1.08, 1.24; p = 0.0002), respectively. When data were analysed for elderly subgroups, systemic exposure in the old-elderly group (age ≥75 years; n = 7) was 27% greater than in young subjects, as compared with 10% greater in the young-elderly group (age 65–74 years; n = 17). Although steady-state exposure to the metabolite R-modafinil acid was also higher in elderly than in young subjects (geometric mean ratios for AUCτ and Cmax were 1.73 and 1.61, respectively; p < 0.0001), there were no significant differences in systemic exposure to modafinil sulfone. Armodafinil was generally well tolerated by both groups. Headache (four subjects in each group), nausea (one in the elderly group and four in the young group), insomnia (two in the elderly group and one in the young group), and dizziness (two in the young group) were the most common adverse events.
Conclusions: Systemic exposure following administration of armodafinil is increased in the elderly in comparison with younger subjects, particularly in those aged ≥75 years. Although the increase in plasma armodafinil concentration in elderly subjects does not appear to result in more adverse events compared with young subjects, consideration should be given to the use of lower dosages of armodafinil for the management of excessive sleepiness in older patients, particularly the very elderly.








Similar content being viewed by others
References
Czeisler CA, Walsh JK, Wesnes KA, et al. Armodafinil for treatment of excessive sleepiness associated with shift work disorder: a randomized controlled study. Mayo Clin Proc 2009 Nov; 84(11): 958–72
Hirshkowitz M, Black JE, Wesnes K, et al. Adjunct armodafinil improves wakefulness and memory in obstructive sleep apnea/hypopnea syndrome. Respir Med 2007 Mar; 101(3): 616–27
Roth T, White D, Schmidt-Nowara W, et al. Effects of armodafinil in the treatment of residual excessive sleepiness associated with obstructive sleep apnea/hypopnea syndrome: a 12-week, multicenter, double-blind, randomized, placebo-controlled study in nCPAP-adherent adults. Clin Ther 2006 May; 28(5): 689–706
Harsh JR, Hayduk R, Rosenberg R, et al. The efficacy and safety of armodafinil as treatment for adults with excessive sleepiness associated with narcolepsy. Curr Med Res Opin 2006 Apr; 22(4): 761–74
Rosenberg R. A phase III, double-blind, randomized, placebo-controlled study of armodafinil for excessive sleepiness associated with jet lag disorder. Mayo Clin Proc 2010 Jul; 85(7): 630–8
Robertson Jr P, Hellriegel ET. Clinical pharmacokinetic profile of modafinil. Clin Pharmacokinet 2003; 42(2): 123–37
Wong YN, Simcoe D, Hartman LN, et al. A double-blind, placebo-controlled, ascending-dose evaluation of the pharmacokinetics and tolerability of modafinil tablets in healthy male volunteers. J Clin Pharmacol 1999 Jan; 39(1): 30–40
Darwish M, Kirby M, Hellriegel ET, et al. Pharmacokinetic profile of armodafinil in healthy subjects: pooled analysis of data from three randomized studies. Clin Drug Investig 2009; 29(2): 87–100
Wong YN, King SP, Simcoe D, et al. Open-label, single-dose pharmacokinetic study of modafinil tablets: influence of age and gender in normal subjects. J Clin Pharmacol 1999 Mar; 39(3): 281–8
Provigil® (modafinil) [US prescribing information]. Frazer (PA): Cephalon Inc., 2008
Darwish M, Kirby M, Hellriegel ET, et al. Armodafinil and modafinil have substantially different pharmacokinetic profiles despite having the same terminal half-lives: analysis of data from three randomized, single-dose, pharmacokinetic studies. Clin Drug Investig 2009; 29(9): 613–23
Darwish M, Kirby M, Hellriegel ET. Comparison of steady-state plasma concentrations of armodafinil and modafinil late in the day following morning administration: post hoc analysis of2 randomized, double-blind, placebo-controlled, multiple-dose studies in healthy male subjects. Clin Drug Investig 2009; 29(9): 601–12
Gooneratne NS, Gehrman PR, Nkwuo E, et al. Consequences of comorbid insomnia symptoms and sleep-related breathing disorder in elderly subject. Arch Intern Med 2006 Sep; 166(16): 1732–8
Johnson KG, Johnson DC. Frequency of sleep apnea in stroke and TIA patients: a meta-analysis. J Clin Sleep Med 2010 Apr; 6(2): 131–7
Luyster FS, Buysse DJ, Strollo Jr PJ. Comorbid insomnia and obstructive sleep apnea: challenges for clinical practice and research. J Clin Sleep Med 2010 Apr; 6(2): 196–204
Wolkove N, Elkholy O, Baltzan M, et al. Sleep and aging 1: sleep disorders commonly found in older people. CMAJ 2007 Apr; 176(9): 1299–304
Durán J, Esnaola S, Rubio R, et al. Obstructive sleep apnea-hypopnea and related clinical features in a population-based sample ofsubjects aged 30 to 70 yr. Am J Respir Crit Care Med 2001 Mar; 163 (3 Pt 1): 685–9
Lichstein KL, Riedel BW, Lester KW, et al. Occult sleep apnea in a recruited sample of older adults with insomnia. J Consult Clin Psychol 1999 Jun; 67(3): 405–10
Ancoli-Israel S, Kripke DF, Klauber MR, et al. Sleep-disordered breathing in community-dwelling elderly. Sleep 1991 Dec; 14(6): 486–95
Chaudhary BA, Husain I. Narcolepsy. J Fam Pract 1993 Feb; 36(2): 207–13
Klotz U. Pharmacokinetics and drug metabolism in the elderly. Drug Metab Rev 2009; 41(2): 67–76
ElDesoky ES. Pharmacokinetic-pharmacodynamic crisis in the elderly. Am J Ther 2007 Sep–Oct; 14(5): 488–98
Darwish M, Kirby M, Robertson Jr P, et al. Interaction profile of armodafinil with medications metabolized by cytochrome P450 enzymes 1A2, 3A4 and 2C19 in healthy subjects. Clin Pharmacokinet 2008; 47(1): 61–74
Nuvigil® (armodafinil) [US prescribing information]. Frazer (PA): Cephalon Inc., 2009
International Conference on Harmonisation (ICH) Expert Working Group. ICH harmonised tripartite guideline: guideline for good clinical practice, E6 (R1). Current step 4 version. 1996 Jun 10 [online]. Available from URL: http://www.ich.org/LOB/media/MEDIA482.pdf [Accessed 2009 Mar 16]
Dinges DF, Arora S, Darwish M, et al. Pharmacodynamic effects on alertness ofsingle doses ofarmodafinil in healthy subjects during a nocturnal period ofacute sleep loss. Curr Med Res Opin 2006 Jan; 22(1): 159–67
Bressler R. Grapefruit juice and drug interactions. Exploring mechanisms of this interaction and potential toxicity for certain drugs. Geriatrics 2006 Nov; 61(11): 12–8
Kinirons MT, O’Mahony MS. Drug metabolism and ageing. Br J Clin Pharmacol 2004 May; 57(5): 540–4
Kuypers DR. Immunotherapy in elderly transplant recipients: a guide to clinically significant drug interactions. Drugs Aging 2009; 26(9): 715–37
Marinac JS, Buchinger CL, Godfrey LA, et al. Herbal products and dietary supplements: a survey of use, attitudes, and knowledge among older adults. J Am Osteopath Assoc 2007 Jan; 107(1): 13–23
Acknowledgements
This study and article were sponsored by Cephalon, Inc., Frazer, PA, USA. All authors are employees of Cephalon, Inc.
The authors wish to acknowledge Virginia Schobel, MSc (formerly of Cephalon, Inc., Frazer, PA) and Trevor Speight (Medicines Information Co., Auckland, New Zealand) for their editorial assistance, which included literature searches, editing and fact checking, graphics support and, at the request of and with guidance from the authors, support for the preparation of the outline and drafting of this manuscript. Additional editorial assistance was provided by the Curry Rockefeller Group, LLC (Tarrytown, NY). The authors would also like to acknowledge the work of the study investigators: Dr Geraldine Bichier (Center for Clinical Trials Research, Gainesville, FL) and Dr Maria Gutierrez (Comprehensive Phase One™, Miramar, FL).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Darwish, M., Kirby, M., Hellriegel, E.T. et al. Systemic Exposure to Armodafinil and Its Tolerability in Healthy Elderly versus Young Men. Drugs Aging 28, 139–150 (2011). https://doi.org/10.2165/11586370-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11586370-000000000-00000