- Department of Neurosurgery, Azerbaijan Medical University, Baku, Azerbaijan,
- Department of Neurosurgery, Neurosurgery Teaching Hospital, Baghdad, Iraq,
- Faculty of Medicine, Mansoura University, Mansoura, Egypt,
- University of Sharjah, College of Medicine, Sharjah, United Arab Emirates,
- Department of Neurosurgery, University of Al-Nahrain, College of Medicine, Baghdad, Iraq,
- Department of Neurosurgery, University of Al-Iraqia, College of Medicine, Baghdad, Iraq,
- Department of Neurosurgery, University of Baghdad, College of Medicine, Baghdad, Iraq,
- Department of Neurosurgery, University of Cincinnati, Cincinnati, Ohio, United States.
Correspondence Address:
Alkawthar M. Abdulsada, Department of Neurosurgery, Azerbaijan Medical University, Baku, Azerbaijan.
DOI:10.25259/SNI_962_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Alkawthar M. Abdulsada1, Mustafa Ismail2, Abdelrahman Mohamed Elsayed3, Mohamed R. Emara4, Younus M. Al-Khazaali5, Sama S. Albairmani6, Ahmed Muthana7, Samer S. Hoz8. Stephanion to cranial base penetrating stab wound with outstanding recovery: A case report. 24-Feb-2023;14:72
How to cite this URL: Alkawthar M. Abdulsada1, Mustafa Ismail2, Abdelrahman Mohamed Elsayed3, Mohamed R. Emara4, Younus M. Al-Khazaali5, Sama S. Albairmani6, Ahmed Muthana7, Samer S. Hoz8. Stephanion to cranial base penetrating stab wound with outstanding recovery: A case report. 24-Feb-2023;14:72. Available from: https://surgicalneurologyint.com/surgicalint-articles/12166/
Abstract
Background: Mortality due to head trauma is common in developed countries in all age groups. Nonmissile penetrating skull base injuries (PSBIs) due to foreign bodies are quite rare, accounting for about 0.4%. PSBI carries that a poor prognosis brainstem involvement usually is often fatal. We are reporting the first case of PSBI with a foreign body insertion site through the stephanion with a remarkable outcome.
Case Description: The 38-year-old male patient was referred with a penetrating stab wound to the head through the stephanion caused by a knife after a conflict in the street. He had no focal neurological deficit or cerebrospinal fluid leak, and Glasgow coma scale (GCS) was 15/15 on admission. A preoperative computed tomography scan showed the path of the stab beginning at the stephanion, which is the point where the coronal suture crosses the superior temporal line, heading toward the cranial base. Postoperatively, GCS was 15/15 without any deficit apart from the left wrist drop, possibly due to a left arm stab.
Conclusion: Careful investigations and diagnoses must be made to ensure convenient knowledge of the case due to the variety of injury mechanisms, foreign body characteristics, and individual patients’ characteristics. Reported cases of PSBIs in adults have not reported a stephanion skull base injury. Although brain stem involvement is usually fatal, our patient had a remarkable outcome.
Keywords: Cranial base, Knife stab, Nonmissile, Penetrating traumatic brain injury, Stephanion
INTRODUCTION
Traumatic brain injury is one of the most frequent causes of death in developed countries in all age groups. Approximately 5 million people die annually due to physical head traumas, in which most cases are preventable. Penetrating skull base injuries (PSBIs) due to foreign bodies (FBs) are not common, representing about 0.4% of all head traumas. Although PSBIs are less prevalent than closed-head traumas, they carry a worse prognosis.[
PSBIs are caused mainly by high-velocity tools that lead to dangerous damage with high mortality rates. Others made by nonmissile low-velocity objects are scarce among civilians, with the better outcome due to being more localized primary injuries. Most intracranial FBs can be defined using a cranial computed tomography (CT) scan. Management for PSBIs includes surgical removal of FBs, control of infection, treatment of vascular injuries, and reconstruction of the skull base.
Herein, we report a case of a 38-year-old male with the left stephanion to cranial base penetrating wound injury caused by a knife after a conflict in the street. The patient underwent surgery for knife removal, pre-and postoperative Glasgow coma scale (GCS) was 15/15, and no neurological deficit was observed.
CASE DESCRIPTION
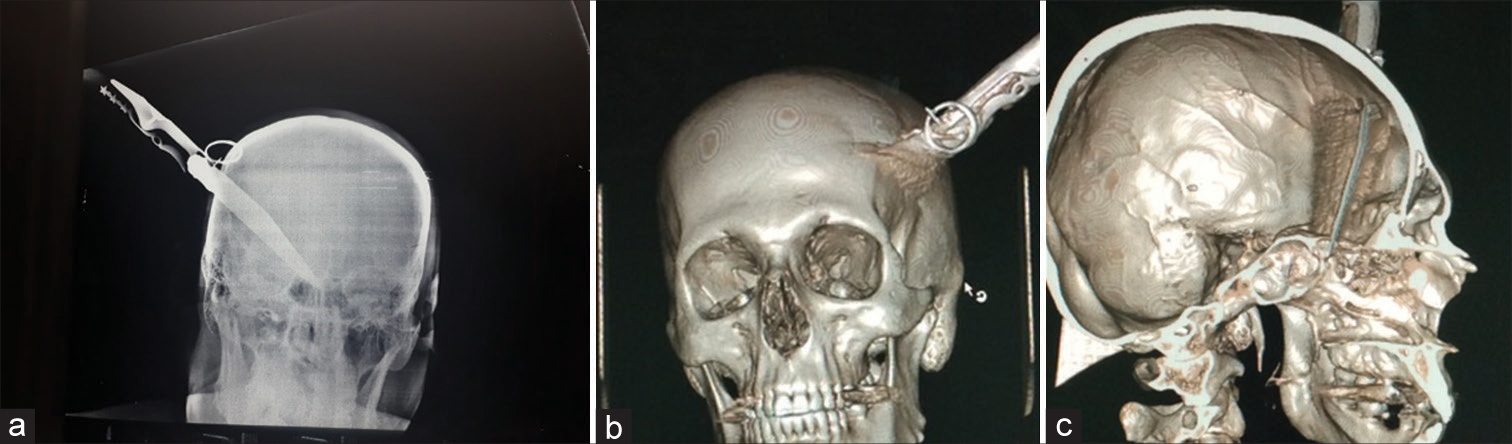
A 38-year-old male patient was referred to the Neurosurgery Teaching hospital with a penetrating stab wound to the head caused by a knife after a conflict in the street [
Figure 2:
(a) Preoperative CT scan, sagittal section, bone window, (b) preoperative CT scan, sagittal section, 3D reconstructed, shows the knife stab penetrating the left Stephanion heading toward the cranial base, (c) preoperative CT scan, coronal section, 3D reconstructed shows the extension of the knife tip to the skull base (posterior ethmoidal sinus). CT: Computed tomography.
DISCUSSION
Mortality due to head trauma is very common among developed countries in all age groups.[
Nonmissile penetrating brain injuries are relatively rare.[
Insertion through the orbital roof is the most common site, followed by temporal squama due to their relative thinness.[
The stephanion provides an important topographic anatomical key point. It can approximate the junction between the inferior frontal sulcus and precentral sulcus.[
We conducted a PubMed Medline database search by the following keywords: (((nonmissile [Title/Abstract]) OR (penetrating injury [Title/Abstract])) AND ((skull base [Title/Abstract]) OR (stephanion))). A total of 33 reported cases of PSBI in adults have been reported. A literature review published in 2017 identified 37 PSBI cases, 29 of which are adult injuries. Other four cases of adult PSBIs were identified after 2017, none describing FB insertion sites through the stephanion.[
CT scans and 3D construction are recommended for PSBI diagnosis to provide a clear image of the case due to the complexity of such cases. CT scan was used to assess anatomical structures surrounding the object and to rule out any slight brain damage since many important structures lie within the skull base. In addition, a 3D-constructed CT scan was obtained, which provided further details to facilitate diagnosis and presurgical planning.[
Such cases should be managed as soon as possible, even if they appear asymptomatic, because they usually deteriorate and have a poor prognosis.[
Complications are common in nonmissile penetrating head injuries, primarily vascular, and infectious complications. Many patients may develop aneurysms and vessel cutoffs. Infections are also common, and the lack of prophylactic antibiotics administration is associated with infectious complications.[
CONCLUSION
Nonmissile PSBIs constitute an essential type of traumatic brain injury. Careful investigations and diagnoses must be made to ensure convenient knowledge of the case due to the variety of injury mechanisms, FB characteristics, and individual patients’ characteristics. Previously reported cases of PSBIs have not reported the stephanion as an FB insertion site. Although brain stem involvement is usually fatal, our patient had a remarkable outcome.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Alafaci C, Caruso G, Caffo M, Adorno AA, Cafarella D, Salpietro FM. Penetrating head injury by a stone: Case report and review of the literature. Clin Neurol Neurosurg. 2010. 112: 813-6
2. Alao T, Waseem M, editors. Penetrating head trauma. StatPearls. Treasure Island, FL: StatPearls Publishing; 2021. p.
3. Aydin S. Intracranial penetrating trauma caused by fishing sinker. World Neurosurg. 2019. 129: 237-40
4. Chaddad-Neto F, Joaquim AF, dos Santos MJ, Linhares PW, de Oliveira E. Microsurgical approach of arteriovenous malformations in the central lobule. Arq Neuropsiquiatr. 2008. 66: 872-5
5. de Holanda LF, Pereira BJ, Holanda RR, Neto JT, de Holanda CV, Filho MG. Neurosurgical management of nonmissile penetrating cranial lesions. World Neurosurg. 2016. 90: 420-9
6. Harrington BM, Gretschel A, Lombard C, Lonser RR, Vlok AJ. Complications, outcomes, and management strategies of non-missile penetrating head injuries. J Neurosurg. 2020. 134: 1658-66
7. Jimenez DF, Barone CM. Early treatment of coronal synostosis with endoscopy-assisted craniectomy and postoperative cranial orthosis therapy: 16-year experience. J Neurosurg Pediatr. 2013. 12: 207-19
8. Lan ZG, Seidu AR, Li J, Yang C. Nonprojectile penetrating iron rod from the oral cavity to the posterior cranial fossa: A case report and review of literature. Int Med Case Rep J. 2018. 11: 41-5
9. Li XS, Yan J, Liu C, Luo Y, Liao XS, Yu L. Nonmissile penetrating head injuries: Surgical management and review of the literature. World Neurosurg. 2017. 98: 873.e9-873.e25
10. Vakil MT, Singh AK. A review of penetrating brain trauma: Epidemiology, pathophysiology, imaging assessment, complications, and treatment. Emerg Radiol. 2017. 24: 301-9
11. Vasella F, Akeret K, Smoll NR, Germans MR, Jehli E, Bozinov O. Improving the aesthetic outcome with burr hole cover placement in chronic subdural hematoma evacuation-a retrospective pilot study. Acta Neurochir (Wien). 2018. 160: 2129-35
12. Yoneoka Y, Aizawa N, Nonomura Y, Ogi M, Seki Y, Akiyama K. Traumatic nonmissile penetrating transnasal anterior skull base fracture and brain injury with cerebrospinal fluid leak: Intraoperative leak detection and an effective reconstruction procedure for a localized skull base defect especially after coronavirus disease 2019 outbreak. World Neurosurg. 2020. 140: 166-72
13. Zhang D, Chen J, Han K, Yu M, Hou L. Management of penetrating skull base injury: A single institutional experience and review of the literature. Biomed Res Int. 2017. 2017: 2838167
14. Zhang M, He Q, Wang Y, Pang S, Wang W, Wang D. Combined penetrating trauma of the head, neck, chest, abdomen and scrotum caused by falling from a high altitude: A case report and literature review. Int Emerg Nurs. 2019. 44: 1-7
15. Zyck S, Toshkezi G, Krishnamurthy S, Carter DA, Siddiqui A, Hazama A. Treatment of penetrating non-missile traumatic brain injury. Case series and review of the literature. World Neurosurg. 2016. 91: 297-307