Prescribing Pattern Analysis in Ureteric Calculus at a Tertiary Care Hospital, Erode, Tamil Nadu
Abstract
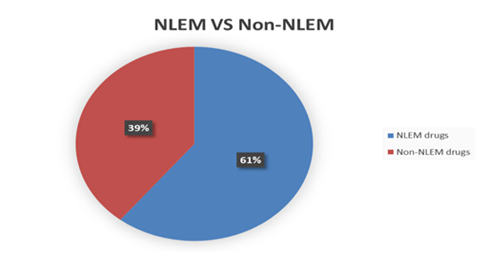
Urolithiasis is one of the most common medical condition of genito-urinary tract which affecting almost 5-15% of the world population and nearly 12 % in India. Nearly 50% of affected patients will have recurrence within 5 years, making it a lifetime disease. Since it is a recurrent condition, the treatment options are not satisfactory for the cure or prevention of ureteric calculus. The present study is mainly evaluating the prescribing pattern of ureteric calculus in a tertiary care center. A retrospective observational study was conducted with 105 prescriptions in the in-patient department of urology in a tertiary care center. The data collected were analyzed by MS Excel sheet & descriptive analysis. It was found that, 72.38% of patients were undergone surgery whereas 21.61% were treated with only drugs. Febuxostat and Hydrochlorothiazide were found to be the mainstay treatment options for the non-surgery patients. Acetaminophen + Diclofenac (375mg) was the most commonly used analgesic (65.71%) in all types of patients. Inj.Amikacin (1g) was the highly prescribed (24.04%) antibiotic during hospitalization and it switched over to T.Trimethoprim+ Sulfamethoxazole (960mg) (26.33%) during discharge. Out of 28 prescribed medicines, 17 were prescribed as per NLEM 2021. The study concluded that, the patients were treated rationally, but there should be a proper intervention on the drugs which are not in the list of NLEM for their use. The use of parentral antibiotics was high, so knowledge among the physicians should be improved by following the updated guidelines and continuous education on urology cases.
Full text article
References
S R Khan. Nephrocalcinosis in animal models with and without stones. Urological Research, 38(6):429–467, 2010.
V Romero, H Akpinar, and D G Assimos. Kidney stones: A global picture of prevalence, incidence, and associated risk factors. Reviews in urology, 12:86–96, 2010.
S N Thornton, Re, D Charles, Alexandria C Scales, Janet M Smith, Christopher S Hanley, and Saigal. Urologic Diseases in america project. prevalence of kidney stones in the United States. European Urology, 62(1):160– 165, 2012.
G Harika and K Srinivas. Renal Calculus A Brief Review. Research and review Journal and medical and health Science, 5(3):2–7, 2016.
B H Eisner and D S Goldfarb. A nomogram for the prediction of Kidney Stone recurrence. Journal of the American Society of Nephrology, 25(12):2685–2692, 2014.
O W Moe. Kidney Stones: Pathophysiol- ogy and medical management. The Lancet, 367(9507):333–377, 2006.
R G Singh, T B Singh, R Kumar, U S Dwivedi, K N Moorthy, and N Kumar. A comparative pilot study of litholytic properties of Celosia Argental (sitivaraka) versus potassium citrate in renal calculus disease. The Journal of Alternative and Complementary Medicine, 18(5):427– 435, 2012.
M López and B Hoppe. History, epidemiology and regional diversities of urolithiasis. Pediatric Nephrology, 25(1):49–59, 2010.
D M Coll, M J Varanelli, and R C Smith. Relation- ship of spontaneous passage of ureteral calculi to stone size and location as revealed by unenhanced helical CT. American Journal of Roentgenology, 178(1):101–104, 2002.
R Rathod, S Gutta, and P Bansal. A giant ureteric calculus. Indian Journal of Urology, 29(3):263–263, 2013.
D W Song, T Y Jeong, S I Lee, and D J Kim. Predicting factors for spontaneous passage of ureteral calculi based on unenhanced helical CT findings. Korean Journal of Urology, 49(12):1094–1094, 2008.
D Prezioso. Laboratory assessment. Urologia Internationalis, 79:20–25, 2007.
N Çiftçioglu, M Björklund, K Kuorikoski, K Bergström, and E O Kajander. Nanobacteria: An infectious cause for Kidney Stone Formation. Kidney International, 56(5):1893–1901, 1999.
H J Kramer, H K Choi, K Atkinson, M Stampfer, and G C Curhan. The association between gout and nephrolithiasis in men: The health professionals’ follow-up study. Kidney International, 64(3):1022–1028, 2003.
D N Baldwin, J L Spencer, and C A Jeffries-Stokes. Carbohydrate intolerance and kidney stones in children in the Goldfields. Journal of Paediatrics and Child Health, 39(5):381–386, 2003.
Mattix Kramer. Menopause and post-menopausal hormone use and risk of incident kidney stones. Journal of the American Society of Nephrology, 14(5):1272–1279, 2003.
C S Biyani and A D Joyce. Urolithiasis in pregnancy. I: Pathophysiology, fetal considerations and diagnosis. BJU International, 89(8):811– 819, 2002.
B G Parulkar, T B Hopkins, M R Wollin, P J Howard, and A Lal. Renal colic during pregnancy: A case for conservative treatment. Journal of Urology, 159(2):365–373, 1998.
A Mutgi. Renal colic. utility of the plain abdominal roentgenogram. Archives of Internal Medicine, 151(8):1589–92, 1991.
M S Parmar. Kidney stones. BMJ, 328(7453):1420–1424, 2004.
T Alelign and B Petros. Kidney Stone Disease: An update on current concepts. Advances in Urology, 2018:1–12, 2018.
A Alevizopoulos, D Zosimas, L Piha, M Hanna, and K Charitopoulos. Managing small ureteral stones: A retrospective study on follow-up, clinical outcomes and cost-effectiveness of conservative management vs. early surgery. Current Urology, 9(1):36–43, 2016.
A Fazlioglu, Y Salman, Z Tandogdu, F O Kurtulus, S Bas, and M Cek. The effect of smoking on spontaneous passage of distal ureteral stones. BMC Urology, 14(1):1–4, 2014.
W H Cordell, T A Larson, J E Lingeman, D R Nelson, J R Woods, L B Burns, and L W Klee. Indomethacin suppositories versus intravenous titrated morphine for the treatment of ureteral colic. Ann. Emerg. Med, 23:262–269, 1994.
E Laerum, O E Omundsen, J E Gronseth, A Christianson, and H E Fagertun. Oral diclofenac in the prophylactic treatment of recurrent renal colic: A double blind comparison with placebo. European urology, 28:108– 111, 1995.
E Laerum and Larsen. Thiazide prophylaxis of urolithiasis. A double-blind study in general practice. Acta Medica Scandinavica, 215(4):383–392, 1984.
J T Cooper, G M Stack, and T P Cooper. Intensive Medical Management of ureteral calculi. Urology, 56(4):575–583, 2000.
M Dellabella, G Milanese, and G Muzzonigro. Efficacy of tamsulosin in the medical management of Juxtavesical ureteral stones. Journal of Urology, 170(6):2202–2207, 2003.
B Resorlu, O F Bozkurt, C Senocak, and A Unsal. Effectiveness Of doxazosin in the management of lower ureteral stones in Male and female patients. International Urology and Nephrology, 43:645–654, 2011.
P Huovinen. Increases in rates of resistance to trimethoprim. Clinical Infectious Diseases, 24(Supplement_1):63–69, 1997.
L P Kotra, J Haddad, and S Mobashery. Aminoglycosides: Perspectives on mechanisms of action and resistance and strategies to counter resistance. Antimicrobial Agents and Chemotherapy, 44(12):3249–56, 2000.
D Landman, E Babu, N Shah, P Kelly, M Backer, and S Bratu. Activity of a novel aminoglycoside, ACHN-490, against clinical isolates of escherichia coli and Klebsiella pneumoniae from New York City. Journal of Antimicrobial Chemotherapy, 65(10):2123–2130, 2010.
H S Sader, C G Carvalhaes, and J M Streit. Antimicrobial activity of cefoperazone sulbactam tested against gram Negative organisms from Europe, Asia-Pacific, and Latin America. Int J Infect Dis, 91:32–37, 2020.
W C Hellinger and N S Brewer. Carbapenems and monobactams: Imipenem, meropenem, and aztreonam. Mayo Clinic Proceedings, 74(4):420–454, 1999.
Authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.