Vitamin D Levels in Chronic Diseases in Primary Care
Article Information
A.Sabic1*, Dz.Sabic2, A.Zejcirovic1, F.Mumic1, S.Bosankic1, S.Hasanovic1
1Department of Family Medicine, Health Center Zivinice, Zivinice, Bosnia and Herzegovina
2Department of Neurology, Health Center Zivinice, Bosnia and Herzegovina
*Corresponding author: Adela Sabic, Department of Family Medicine, Health Center Zivinice, Zivinice, Bosnia and Herzegovina
Received: 21 March 2020; Accepted: 28 March 2020; Published: 16 April 2020
Citation: A.Sabic, Dz.Sabic, A.Zejcirovic, F.Mumic, S.Bosankic, S.Hasanovic. Vitamin D Levels in Chronic Diseases in Primary Care. Archives of Clinical and Biomedical Research 4 (2020): 083-088.
View / Download Pdf Share at FacebookAbstract
The aim of this paper is to highlight the role and level of vitamin D in chronic diseases at the primary level of their treatment.
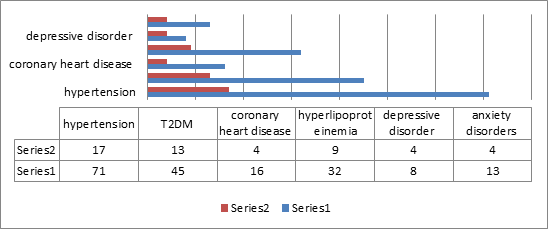
Methods and patients: At Zivinice Health Care Center 81 patients were analyzed between March and September 2019, with 39 men (48.1%) and 42 (51.9%) women. The mean age of the patients was 62 ± 10 years. The youngest patient was 24 years old and the oldest 80 years old. Patients with long-term hypertension (71 patients, 36 women and 35 men), coronary heart disease (16 patients, 8 women and 8 men), type 2 diabetes (T2DM, 45 patients, 22 women and 23 men) were observed, hyperlipoproteinemia (32 patients, 17 women and 15 men), depressive disorder (8 patients, 3 women and 5 men), and anxiety (13 patients, 8 women and 5 men). Vitamin D levels were determined at the University Clinical Center Tuzla, Department of Biochemistry, and 36.8-171.0 mmol / L were taken as reference values. The statistics were analyzed in the SSPS.
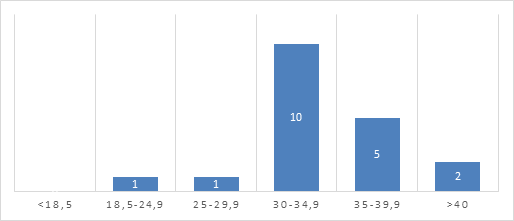
Results: The mean vitamin D level in patients with chronic diseases was 53.3 mmol / L. Standard deviation (SD) ± 20.9. The reference values for vitamin D levels were 62 patients or 76.5% and 19 or 23.5% had decreased vitamin D. In patients with hypertension, 17 had a reduced vitamin D level (p 0.063). Of the 45 diabetic patients, 13 had reduced levels of vitamin D (p 0.202). Patients with ischemic heart disease 4 of them had lowered vitamin D (p 0.873). In patients with hyperlipoproteinemia, 9 of them have lowered vitamin D (p 0,429). There are 4 patients with reduced levels of vitamin D with depressive disorder and 4 with patients with anxiety disorders with reduced levels of vitamin D (p 0,113). One patient had a body mass index (BMI) of less than 18.5, 6 patients had a neat BMI, 30 patients were overweight. 26 patients had grade I thickness, 16 patients had grade II thickness and two BMI patients over 40 m2 / kg.In t
Keywords
Vitamin D; Chronic diseases; Prevention
Vitamin D articles, Chronic diseases articles, Prevention articles
Article Details
Introductıon
The most common chronic diseases in family medicine clinics are hypertension, coronary heart disease, type 2 diabetes mellitus, hyperlipidemia, depressive disorder, anxiety and obesity. Each of these diseases has pharmacological and non-pharmacological treatment measures. In the treatment of hypertension, in addition to medication, it is commonly advised to reduce sodium intake, control of body weight, physical activity, but also intake of vitamin D and minerals, which greatly contribute to better regulation of the disease [1]. Earlier studies on cardiovascular disease showed that severe vitamin D deficiency was associated with an increased risk of acute myocardial infarction [2]. In a meta-analysis of 19 studies of the association between low-level 25-OH D and the incidence of cardiovascular disease in almost 7,000 subjects, a link was found between vitamin D and a higher incidence of coronary heart disease and stroke [3]. Recent large-scale observational studies have demonstrated a strong inverse correlation between plasma levels of 25(OH) D and coronary atherosclerosis [4]. It is shown in coronary arteries that in low concentrations calcitriol inhibits calcification of the tunica media and interna [5]. When we are treating hyperlipoproteinemia, it is necessary to know what type of disease we have in the patient. High blood cholesterol levels occur in disorders of hyperlipoproteinemia, which are elevated blood lipopoprotein levels, and lipoproteins are carriers of blood cholesterol. Low density lipoproteins (LDL) and high density lipopoproteins (HLD) play the most important role in the transmission of cholesterol. As we know, cholesterol is an important component of the human body. It synthesizes D-vitamin and many hormones and is an important constituent of the membrane of every cell in the body. Serotonin is one of the major neurotransmitters of the central nervous system and biochemical imbalances in the brain can lead to depression and anxiety. Earlier studies have shown that Vitamin D regulates serotonin in the brain and thus contributes to better mood in the general population.Vitamin D supplements are currently widely used in the general population, especially in winter [6]. Deficiency of vitamin D in obese subjects is a well-documented finding that is most probably due to volumetric dilution into the greater volumes of fat, serum, liver, and muscle present in obese people [7]. In our research the results show a statistically significant difference was found in the decreased vitamin D in the group of patients with BMI 30-34.9 compared to other groups of patients according to the BMI. No statistically significant difference in vitamin D levels was found between the groups of patients with chronic diseases.
Methods and Patıents
At Zivinice Health Care Center 81 patients were analyzed between March and September 2019, with 39 men (48.1%) and 42 (51.9%) women. The mean age of the patients was 62 ± 10 years. The youngest patient was 24 years old and the oldest 80 years old. Patients with long-term hypertension (71 patients, 36 women and 35 men), coronary heart disease (16 patients, 8 women and 8 men), type 2 diabetes (T2DM, 45 patients, 22 women and 23 men) were observed, hyperlipoproteinemia (32 patients, 17 women and 15 men), depressive disorder (8 patients, 3 women and 5 men), and anxiety (13 patients, 8 women and 5 men). Vitamin D levels were determined at the University Clinical Center Tuzla, Department of Biochemistry, and 36.8-171.0 mmol / L were taken as reference values. The statistics were analyzed in the SSPS.
Results
The mean vitamin D level in patients with chronic diseases was 53.3 mmol / L. Standard deviation (SD) ± 20.9. The reference values for vitamin D levels were 62 patients or 76.5% and 19 or 23.5% had decreased vitamin D. In patients with hypertension, 17 had a reduced vitamin D level (p 0.063). Of the 45 diabetic patients, 13 had reduced levels of vitamin D (p 0.202). Patients with ischemic heart disease 4 of them had lowered vitamin D (p 0.873). In patients with hyperlipoproteinemia, 9 of them have lowered vitamin D (p 0,429). There are 4 patients with reduced levels of vitamin D with depressive disorder and 4 with patients with anxiety disorders with reduced levels of vitamin D (p 0,113) (Figure 1) . One patient had a body mass index (BMI) of less than 18.5, 6 patients had a neat BMI, 30 patients were overweight. The 26 patients had grade I obesity, 16 patients had grade II obesity and two BMI patients over 40 m2 / kg. In the BMI group 30-34.9 there were 10 patients with reduced vitamin D values (p 0.002), which is a statistically significant difference compared to other patient groups according to the BMI.
Discussion
In our study the results show a statistically significant difference was found in the decreased vitamin D in the group of patients with BMI 30-34.9 compared to other groups of patients according to the BMI (p=0.002). No statistically significant difference in vitamin D levels was found between the groups of patients with chronic diseases. Randomized studies have shown that overweight and obese adults found that the addition of 1050 mg calcium with 300 IU of vitamin D daily was associated with a significant reduction in visceral adiposity compared with placebo [8]. Also, earlier research confirm that a lower vitamin D level is a very common condition among obese subjects. Vitamin D was independently related to higher BMI, diastolic blood pressure and insulin serum levels [9]. At the primary care level, it should always be kept in mind that when screening children and young people, we influence the prevention of obesity. Recent studies suggest a relationship between vitamin D levels and overweight in adolescents and increased cardiovascular risk. In their research, they found that severity of obesity was inversely related to vitamin D levels [10]. As studies have shown lower levels of vitamin D in obese people, it is known that the bioavailability of vitamin D is reduced in obese people. The mechanism of action of vitamin D is via the vitamin D receptors which are found in more than 37 body tissues [11]. For example, the study found that individuals with the AA genotype BsmI had significantly lower levels of 25 (OH) D (p = 0.001) compared to other genotypes [12].
Conclusıon
The most common chronic diseases in family medicine clinics are hypertension, coronary heart disease, type 2 diabetes mellitus, hyperlipidemia, depressive disorder, anxiety and obesity and Vitamin D levels were lower in all of the above. In the obese group patients with BMI 30-34.9 there were 10 patients with reduced vitamin D values (p 0.002), which is a statistically significant difference compared to other patient groups according to the BMI. With the fact that chronic diseases are in themselves complex and difficult to treat, we should pay more attention to the level of vitamin D, which by its action can improve the quality of life of patients and contribute to better quality of treatment.
Author’s contribution
Adela Sabic, substantial contribution to conception and design, substantial contribution to acquisition of data, substantial contribution to analysis and interpretation of data, drafting the article. Dzevad Sabic, substantial contribution to conception and design, final approval of the version to be published. Critically revising the article for important intellectual content. Alema Zejcirovic and Fatima Mumic, substantial contribution to conception and design, substantial contribution to acquisition of data, substantial contribution to analysis and interpretation of data, drafting the article. Sedina Bosankic, Sejla Hasanovic, Amra Alibasic drafting the article.
Conflict of interest
None declared.
References
- Rosa MOA, Ana IJO, Jose MPS, Esther CS, et al. Nutritional patterns on prevention and control of hypertension. Nutr Hosp 33 (2016): 53-58.
- Babikir K, Ahmed A, Mohammed O, Sahar A, et al. Vitamin D deficiency and risk of cardiovascular diseases: a narrative review. Clinical Hypertension 24 (2018): 9.
- Darija VB, Zlatko G, Vesna K, Nadica Lž, et al. Smjernice za prevenciju, prepoznavanje i liječenje nedostatka vitamina D u odraslih. Liječ Vjesn 138 (2016): 121–132.
- Christian L, Daniela G, Marcus K, Manfred I and Markus W. Potential beneficial efects of Vitamin D in coronary artery disease. Nutrients 12 (2020): 99.
- Ewelina AD, Sebastian P, Marek D. The effects of vitamin D on severity of coronary artery atherosclerosis and lipid profile of cardiac patients. Arch Med Sci 6 (2016): 1199–1206.
- Maria AC, Tamlin SC, Jill JH, Michelle JH and Lisa AH. Effect of vitamin D supplementation on depressive symptoms and psychological wellbeing in healthy adult women: a double-blind randomised controlled clinical trial. Journal of Nutritional Science 23 (2018):1-10.
- Luka V, Ivana M and Sandra M. Vitamin D Deficiency: Consequence or Cause of Obesity? Medicina 55 (2019): 541.
- Simon V. Vitamin D and obesity. Nutrients 5 (2013): 949-956.
- Roberta Z, Fabio C, Rodolfo S, Luisa L, Carmen DN et all. Hydroxyvitamin D serum levels are negatively associated with platelet number in a cohort of subjects affected by overweight and obesity. Nutrients 12 (2020): 474.
- Aslı OG, Müjgan A, Ethem E, Selmin K, Emre Ç et all. The relationship between cardiometabolic risks and vitamin D levels with the degree of obesity. Turk Pediatri Ars 54 (2019): 256–63.
- Zahra SK, Marzieh K, Parastoo T, Akbar HZ, Mohammad HE. Effect of Vitamin D supplementation on weight loss, glycemic indices, and lipid profile in obese and overweight women: A clinical trial study. International Journal of Preventive Medicine 9 (2018): 63.
- Rayinda R, Nur LZ, Zahurin M, Foong MM, Muhammad YJ. The associations between VDR BsmI polymorphisms and risk of vitamin D deficiency, obesity and insulin resistance in adolescents residing in a tropical country. Plos One 12 (2017): e0178695.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 