Postpartum Hemorrhage; Incidence and Prognosis
Article Information
Zelmat SA*, Bouabida D, Boucherit DE, Boucherit E, Mazour F
Department of Medicine, University of Oran, Algeria
*Corresponding Author: Zelmat SA, Department of Medicine, University of Oran, Algeria
Received: 30 March 2022; Accepted: 08 April 2022; Published: 27 April 2022
Citation: Zelmat SA, Bouabida D, Boucherit DE, Boucherit E, Mazour F. Postpartum Hemorrhage; Incidence and Prognosis. Anesthesia and Critical Care 4 (2022): 98-103.
View / Download Pdf Share at FacebookAbstract
During the study period a total of 1000 deliveries; 74 parturients presented with PPH, an incidence of 7.4% [95% CI 6.3-6.5] with that of severe PPH at 2.7% [95% CI 1.6-1.8]. maternal age varied between 30 and 42 years. The average age in our sample was: 34.33 ± 6.030 years. Mean term: 38.69 ± 1.25 weeks gestation mean was 3.8 ± 1.6. The oldest parity was 3.2 ± 2 with extremes of 1 and 8. 73.7% were multiparous (2 deliveries and more). RBC transfusion was done in 97.5%. Oxytocics were administered in 95.8%. Uterine inertia following a placentation anomaly (accreta, increta and percreta) remains the most frequent etiology in 79.8%, and coagulation disorders 15.2% (congenital or acquired) and 5% of entangled causes (ATCD from Covid19, death in utero, help ). As for the mode of delivery, the upper route is the most frequent with 70% of cases RBC transfusion was done in 97.5%. Oxytocics were administered in 95.8%. Uterine revision was performed in 80.6%. , artificial delivery was done in 26.4%. Vascular ligation was done in 20.8%. Hemostatic hysterectomy was required in 19.4%. Hospitalization in the maternal intensive care unit was necessary in 70.9% with an average duration of 3.5 days. There were 73% cases of disseminated intravascular coagulation (DIC), 50% renal failure (IR) of which two were hemodialysis. The death rate was 18%. Three risk factors associated with a poor maternal prognosis: severe hypovolaemia (p = 0.0001), disseminated intravascular coagulation abnormalities (p = 0.006) and organic renal failure (p = 0.0013).
Keywords
Bleeding, Hypovolaemia, Pathology of coagulation Hysterectomy-Death
Bleeding articles; Hypovolaemia articles; Pathology of coagulation Hysterectomy-Death articles
Bleeding articles Bleeding Research articles Bleeding review articles Bleeding PubMed articles Bleeding PubMed Central articles Bleeding 2023 articles Bleeding 2024 articles Bleeding Scopus articles Bleeding impact factor journals Bleeding Scopus journals Bleeding PubMed journals Bleeding medical journals Bleeding free journals Bleeding best journals Bleeding top journals Bleeding free medical journals Bleeding famous journals Bleeding Google Scholar indexed journals Hypovolaemia articles Hypovolaemia Research articles Hypovolaemia review articles Hypovolaemia PubMed articles Hypovolaemia PubMed Central articles Hypovolaemia 2023 articles Hypovolaemia 2024 articles Hypovolaemia Scopus articles Hypovolaemia impact factor journals Hypovolaemia Scopus journals Hypovolaemia PubMed journals Hypovolaemia medical journals Hypovolaemia free journals Hypovolaemia best journals Hypovolaemia top journals Hypovolaemia free medical journals Hypovolaemia famous journals Hypovolaemia Google Scholar indexed journals Pathology of coagulation Hysterectomy-Death articles Pathology of coagulation Hysterectomy-Death Research articles Pathology of coagulation Hysterectomy-Death review articles Pathology of coagulation Hysterectomy-Death PubMed articles Pathology of coagulation Hysterectomy-Death PubMed Central articles Pathology of coagulation Hysterectomy-Death 2023 articles Pathology of coagulation Hysterectomy-Death 2024 articles Pathology of coagulation Hysterectomy-Death Scopus articles Pathology of coagulation Hysterectomy-Death impact factor journals Pathology of coagulation Hysterectomy-Death Scopus journals Pathology of coagulation Hysterectomy-Death PubMed journals Pathology of coagulation Hysterectomy-Death medical journals Pathology of coagulation Hysterectomy-Death free journals Pathology of coagulation Hysterectomy-Death best journals Pathology of coagulation Hysterectomy-Death top journals Pathology of coagulation Hysterectomy-Death free medical journals Pathology of coagulation Hysterectomy-Death famous journals Pathology of coagulation Hysterectomy-Death Google Scholar indexed journals Postpartum hemorrhage articles Postpartum hemorrhage Research articles Postpartum hemorrhage review articles Postpartum hemorrhage PubMed articles Postpartum hemorrhage PubMed Central articles Postpartum hemorrhage 2023 articles Postpartum hemorrhage 2024 articles Postpartum hemorrhage Scopus articles Postpartum hemorrhage impact factor journals Postpartum hemorrhage Scopus journals Postpartum hemorrhage PubMed journals Postpartum hemorrhage medical journals Postpartum hemorrhage free journals Postpartum hemorrhage best journals Postpartum hemorrhage top journals Postpartum hemorrhage free medical journals Postpartum hemorrhage famous journals Postpartum hemorrhage Google Scholar indexed journals renal failure articles renal failure Research articles renal failure review articles renal failure PubMed articles renal failure PubMed Central articles renal failure 2023 articles renal failure 2024 articles renal failure Scopus articles renal failure impact factor journals renal failure Scopus journals renal failure PubMed journals renal failure medical journals renal failure free journals renal failure best journals renal failure top journals renal failure free medical journals renal failure famous journals renal failure Google Scholar indexed journals disseminated intravascular coagulation articles disseminated intravascular coagulation Research articles disseminated intravascular coagulation review articles disseminated intravascular coagulation PubMed articles disseminated intravascular coagulation PubMed Central articles disseminated intravascular coagulation 2023 articles disseminated intravascular coagulation 2024 articles disseminated intravascular coagulation Scopus articles disseminated intravascular coagulation impact factor journals disseminated intravascular coagulation Scopus journals disseminated intravascular coagulation PubMed journals disseminated intravascular coagulation medical journals disseminated intravascular coagulation free journals disseminated intravascular coagulation best journals disseminated intravascular coagulation top journals disseminated intravascular coagulation free medical journals disseminated intravascular coagulation famous journals disseminated intravascular coagulation Google Scholar indexed journals intensive care unit articles intensive care unit Research articles intensive care unit review articles intensive care unit PubMed articles intensive care unit PubMed Central articles intensive care unit 2023 articles intensive care unit 2024 articles intensive care unit Scopus articles intensive care unit impact factor journals intensive care unit Scopus journals intensive care unit PubMed journals intensive care unit medical journals intensive care unit free journals intensive care unit best journals intensive care unit top journals intensive care unit free medical journals intensive care unit famous journals intensive care unit Google Scholar indexed journals
Article Details
1. Introduction
Postpartum hemorrhage (PPH) remains the leading cause of direct obstetric maternal mortality in Algeria, unlike most other developed countries [1]. It is also the first cause of severe morbidity [2]. Moreover, it appears that, all over the world, this maternal complication is the one for which the management is the most insufficient and for which much progress can and must be made [2]. Indeed, 60 to 90% of maternal deaths due to PPH are potentially avoidable [3]. The key point of this management is a well-functioning multidisciplinary approach within each maternity hospital, based on national and international recommendations as well as on a good knowledge of the physiopathology, etiologies and available treatments. Its incidence is particularly frequent in type III centers and leads to significant maternal morbidity and mortality and the implementation of second-line treatments. PPH is defined as a blood loss greater than 1000mL, or a peripartum hemoglobin loss greater than 2g/dL. PPH is said to be severe if blood loss is greater than 1000 ml. It is defined by the presence of at least one of the following criteria: hemoglobin loss greater than or equal to 4g/dL, embolization, conservative surgery, hysterectomy, transfusion, transfer to intensive care, or death. PPH is an obstetrical emergency, which is life-threatening for the mother. The incidence of severe PPH is around 2%. Uterine atony is the main cause of PPH. Genital tract wounds are responsible for approximately 1 in 5 cases of PPH. This hemorrhage represents the first cause of maternal mortality and is responsible for 25% of preventable maternal deaths.
Objective
This work is to determine the incidence of severe PPH in the university hospital of Oran.
2. Patients and Methods
It is a descriptive, prospective study. Mono centric, which took place at the EHUD'Oran over a period from 15/03/2020 to 15/03/2021. All patients with severe PPH were included. Maternal characteristics: age, gesity, parity, medical and obstetrical history, existence of uterine atony or coagulopathy, mode of delivery, management modalities, transfers to the intensive care unit, as well as maternal complications were collected on survey forms prepared for the study. The data were analyzed using SPSS 20 software.
3. Results
During the study period a total of 1000 deliveries 74 parturient presented with PPH, an incidence of 7.4% [95% CI 6.3-6.5] with that of severe PPH was 2.7% [95% CI 1.6-1.8]. Maternal age ranged from 30 to 42 years. The average age in our sample was: 34.33±6.03 years. The mean term was 38.69±1.25 years, the mean gestation was 3.8±1.6 years, the mean parity was 3.2±2 with extremes of 1 and 8. 73.7% were multiparous (2 or more deliveries). Uterine inertia due to placental anomaly (accreta, increta and percreta) was the most frequent etiology in 79.8%, and coagulation disorders in 15.2% (congenital or acquired) and 5% of interrelated causes (history of Covid19, death in utero, help.)
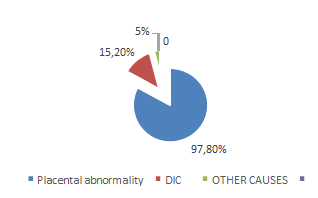
Figure 1: Distribution of patients by etiology of the HPP
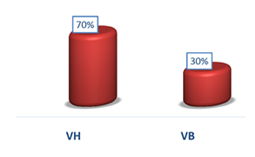
Figure 2: Distribution of parturients according to delivery route
VB low way
VA high way
Red blood cells were transfused in 97.5% of patients. Oxytocics were administered in 95.8%. Uterine revision was performed in 80.6%. Artificial delivery was performed in 26.4%. Vascular ligation was performed in 20.8%. Hemostasis hysterectomy was necessary in 19.4%. (Figure 3) Hospitalization in the maternal intensive care unit was necessary in 70.9% of cases, with an average duration of 3.5 days (Table 1).
|
Hospitalization Kindergarten |
In Reanimation |
In unit of groseese a hut risk |
|
Number percentage |
125(22,7%) |
426(77,3%) |
|
22(6,5%) |
316(93,5%) |
|
|
Average length of hospital stay days |
3,5 |
7,8 |
Table 1: Frequency of patients hospitalized in intensive care and length of hospitalization
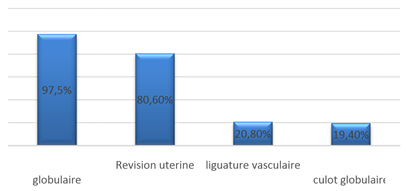
Figure 3: Distribution of parturients according to treatment
Disseminated intravascular coagulation (DIC) was reported in 73% of cases, renal failure (RF) in 50% of cases, two of which required hemodialysis. The death rate was 18% (Figure 4). Three risk factors associated with poor maternal prognosis: severe hypovolemia (p = 0.0001), disseminated intravascular coagulation abnormalities (p = 0.006) and organic renal failure (p = 0.0013).
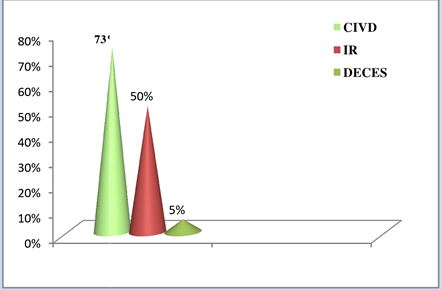
Figure 4: Distribution of partruients according to severe complications
4. Discussion
During the study period the incidence of PPH was 7.4% [95% CI 6.3-6.5] and that of severe PPH was 2.7% [95% CI 1.6-1.8].Our results are consistent with the literature[4,5]. Dupont C in 2014 and in 2009,in France finds an incidence of PPHthat varies from 1.5 to 22% depending on the maternity hospital[5]. This suggests an implication of the adequacy of postpartum surveillance at our level. In our study, regarding the incidence of PPH is much more frequent after caesarean section than in vaginal delivery our results are similar to those found in literature [6]. The incidence of placental anomalies has been steadily increasing over the last twenty years and reached 1/533 in 2002 [7,8]. The implication of placental anomalies in the occurrence of severe, even cataclysmic, PPH justifies a collegial reflection on its management. Indeed, according to studies, patients with an adherent placenta (accreta, increta and percreta) have an increased risk of haemostasis hysterectomy by 43. (OR= 43, 95% CI: 19- 98) [53,8]. This result confirms that obtained prospectively in 117 parturients [14,9]. Other etiologies are represented by uterine inversion (rare <1/1000 and iatrogenic) and coagulation disorders (congenital or acquired) which can be both cause and consequence of PPH, this coagulation disorder is consistent with our study. Mortality rates in developed countries are around 1/100,000 for the United Kingdom, 8.9/100,000 for the United States and can reach 1% in our series. The death rate is similar to that of developing countries [1, 9-12] [10-13]. Delivery hemorrhage is an obstetrical emergency that constitutes the first cause of maternal mortality. Uterine atony remains the main etiology; it often seems avoidable because most patients at risk can be identified before or during labor. In this respect, obstetrical management of delivery is essential; it allows for the necessary prevention and treatment measures to be taken. Once the hemorrhage has set in, any delay or hesitation in the multidisciplinary management is detrimental because it favors the appearance of coagulation disorders and the installation of a vicious circle.
5. Conclusion
PPH is a complex situation because it represents an obstetrical emergency that can jeopardize the maternal vital prognosis. In this respect, preventive measures, early multidisciplinary management by codified protocols well adapted to each health structure are the only guarantee of a good prognosis. The objective here is to update the content, focusing mainly on the place of pro-hemostatic treatments and on the management of placenta accreta.
Declaration of interest
The authors declare that they have no ties of interest.
References
- 3rd report of the National Expert Committee on Maternal Mortality (CNEMM) Inserm Unit 953, (period 2001-2006). InVs, Institut de Veille Sanitaire (2010).
- Bouvier-Colle MH, Ould El Joud D, Varnoux N, et al. Evaluation of the quality of care for severe obstetrical haemorrhage in three French regions. BJOG 108 (2001): 898-903.
- Walfish M, Neuman A, and Wlody D, Maternal haemorrhage. Br J Anaesth 103 (2009): 47-56.
- Dupont C, Douzet S, Colin C. et al. Incidence and management of postpartum haemorrhage following the dissemination of guidelines in a network of 16 maternity units in France. International Journal of Obstetric Anesthesia 18 (2009): 320-327.
- Dupont C, Rudigoz RC, Cortet M, et al. Frequency, causes and risk factors of postpartum haemorrhage: a population-based study in 106 French maternity units. J Gynecol Obstet Biol Reprod 43 (2014): 244-253.
- Vendittelli F, Barasinski C, Pereira B, et al. Incidence of immediate postpartum hemorrhages in French maternity units: a prospective observational study (HERA study). BMC Pregnancy Childbirth 16 (2016): 242.
- Wu S, Kocherginsky M, Hibbard JU. Abnormal placentation: twenty-year analysis. Am J Obstet Gynecol 192 (2005): 1458-1461.
- O' Brien D, Babiker E, O'Sullivan O, et al. Prediction of peripartum hysterectomy and end organ dysfunction in major obstetric haemorrhage. European Journal of Obstetrics & Gynecology and Reproductive Biology 153 (2010): 165-169.
- Bodelon C, Bernabe-Ortiz A, Schiff MA, et al. Factors associated with peripartum hysterectomy. Obstet Gynecol 114 (2009): 115-123.
- World Health Organization- Maternal Mortality (2018).
- World Health Organization- WHO Recommendations for the Prevention and Treatment of Postpartum Hemorrhage (2014).
- American College of Obstetricians and Gynecologists. ACOG Practice Bulletin: Clinical Management Guidelines for Obstetrician- Gynecologists Number 183, October 2017: postpartum haemorrhage. Obstet Gynecol 130 (2017): e138-816.
- Mavrides E, Allard S, Chandraharan E, et al. On behalf of the Royal College of Obstetricians and Gynaecologists. Prevention and management of postpartum haemorrhage. BJOG 124 (2016): e106-e149.

 Impact Factor: * 2.1
Impact Factor: * 2.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 