A Case Report On Intraocular Cystocercosis and the Occurrence of A Live Free Floating Cyst in the Anterior Chamber of the Eye
Article Information
Juna Musa1, Loran Rakovica2, Luela Hallunovaj3, Edlira Horjeti4, Erisa Kola5, Ali Guy6, Ermal Simaku3, Blina Abdullahu7, Fiolla Hyseni8, Alketa Tandili3*
1Postdoctoral Research Fellow, Department of Surgery, Mayo Clinic, Rochester, Minnesota, USA
2Faculty of Medicine, University of Prishtina, Kosovo
3Ophthalmologist, Eye Clinic, UHC ?Mother Teresa?, Tirane, Albania
4Family Doctor, Department of Family Medicine, Tirane, Albania
5Pathologist, Department of Pathology, Albania
6Department of Physical Medicine and Rehabilitation, New York University, School of Medicine, NYU Medical Center, New York, USA
7Medical Doctor, University of Medicine of Tirana, Albania
8Research Fellow, Department of Urology, NYU, NY, USA
*Corresponding Author: Dr. Alkeda Tandili, Ophthalmologist, Eye Clinic, UHC ?Mother Teresa?, Tirane, Albania
Received: 14 July 2020; Accepted: 22 July 2020; Published: 08 September 2020
Citation: Juna Musa, Loran Rakovica, Alketa Tandili, Luela Hallunovaj, Edlira Horjeti, Ali Guy, Ermal Simaku, Erisa Kola. A Case Report On Intraocular Cystocercosis and the Occurrence of A Live Free Floating Cyst in the Anterior Chamber of the Eye. Archives of Clinical and Medical Case Reports 4 (2020): 774-778.
View / Download Pdf Share at FacebookAbstract
Ocular cysticercosis is a parasitic infestation caused by Cysticercus cellulosae, known as the larval form of Taenia solium. It occurs through consumption of fecally contaminated food or by intestinal autoinfection. Ocular cysticercosis can involve the ocular adnexa, the subconjunctival space, and the anterior and posterior segments of the eye. Anterior chamber cysticercosis is unusual. It has a worldwide distribution, most commonly found in developing countries with poor sanitation like East Asia, sub-Saharan Africa and some parts of Latin America. Due to its varied presentation, cysticercosis may pose a diagnostic challenge to health professionals. Early diagnosis and management can prevent vision loss and optimize visual outcomes.
Below we report a rare case of an 11-year-old female presenting with blurriness and conjunctival injection to her left eye after visiting the countryside. Initial BCVA was noted to be 0.4. Histopathological findings showed scolex in the left anterior chamber and membranous cyst wall suggestive of cysticercus cellulosae. Management with viscoexpression, fixation of cyst along with topical and systemic medication showed satisfactory improvement with a post-operative BCVA of 1.0.
Keywords
Ocular cysticercosis; Taenia solium; Cysticercus cellulosae; Viscoexpression
Ocular cysticercosis articles, Taenia solium articles, Cysticercus cellulosae articles, Viscoexpression articles
Article Details
1. Introduction
Cysticercosis is parasitic infection in which the human tissue is invaded by the cystic form of the larvae of the Taenia solium, ingested via the feces of a human with a tapeworm (human-to-human fecal-oral transmission) leading to variable clinical manifestations [1]. These larval cysts are a major cause of adult onset seizures in most low income countries. Owing to increased migration of people, cysticercosis has gained global significance and has become a major health problem worldwide [2]. While the adult tapeworm in the human intestine (taeniasis) does not have a major health impact, humans can also develop cysticercosis with tapeworm larvae (cysticerci) in the muscles, subcutaneous tissues, central nervous system and eyes [3]. Ocular cysticercosis, though rare, can be extraocular (subconjunctival, in orbital tissues) or intraocular (vitreous, subretinal space, or anterior chamber). Ocular manifestations usually occur as a part of a systemic infection and can lead to partial or complete visual impairment over a 3-5-year period. CNS involvement also poses a major threat; therefore, a prompt and accurate diagnosis along with the right treatment options are tremendously important.
2. Case Report
An 11-year old girl presented with the chief complaint of progressive blurry vision and painless conjunctivitis to the left eye. Otherwise rather healthy; no history of double vision or a decrease in visual activity prior to a current peak of her vision acuity was noted. The patient claims that approximately 5 months ago she visited her cousins in the countryside. She sometimes helped them in the stall feeding the cattle where sanitation was minimal. Patient denies consuming any undercooked pork, trauma to the eyes, fever or any previous seizure attacks. Afterwards, a Slit Lamp examination was performed, which is a simple procedure helping to contribute to the diagnosis of intraocular Cysticercosis of the left eye. This examination revealed a mobile crystal lucid larva with scolex in the left anterior chamber without perforation or attachment of the cyst to nearby structures like the iris, cornea or lens. Right eye examination was intact.
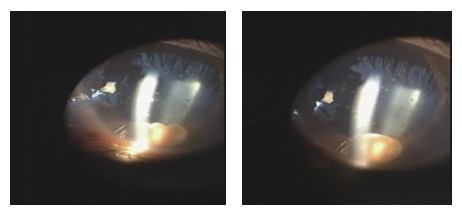
Figure 1: Slit-lamp examination.
Fundus oculi examination displayed no retinopathy and oculomotor movements were within normal limits for both eyes, respectively. Moreover, a stool microbiology test resulted positive for cysticerci parasites helping us to furthermore confirm the diagnosis and move forward with the management of our 11-year-old patient. MRI examination showed a hyperintense scolex image; and the cyst with a lesser intensity, similar to that of CSF. MRI of the brain revealed no lesions in the brain parenchyma. The neurologic system was intact, thus explaining normal MRI findings; as patient has never had history of seizures before. On histopathological H & E stain, a translucent flexible larva measured 1.8x1.5mm, with a scolex and membranous cyst wall suggestive of cysticercus cellulosae. Pre-treatment BCVA resulted a 0.4 with mild vision loss. Extraction and fixation of the mobile translucent cyst with visceoexpression method was executed with local anesthesia. Along with topical eyedrops and an anthelmintic systemic medication; post-operative BCVA showed satisfactory visual improvement of 1.0.
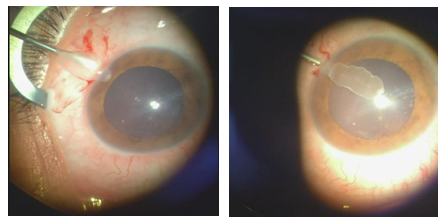
Figure 2: Extraction of cyst.
Close monitoring was crucial for our patient after this mini invasive procedure. A course of Albendazole and other steroids were given for possible parasitic recurrence. Other investigations were also performed to prevent potential complications.
3. Discussion
Cysticercosis is a parasitic tissue infection caused by larval cysts of the tapeworm Taenia solium, cysticercus cellulosae. Human beings are definitive hosts that harbor the adult parasite in the intestine and pigs are the intermediate hosts harboring the larvae. After ingestion, the eggs of Taenia solium hatch into larvae, which can pierce the gut to reach the bloodstream and enter various tissues (particularly the central nervous system, eyes and striated muscle) where they develop into cysts producing the clinical syndrome of cysticercosis [5]. Both the taeniasis (tapeworm intestinal infection) and cysticercosis (involving muscles, subcutaneous tissues, CNS and eyes) occur globally, but the highest rates of infection are found in developing countries with inadequate sanitation [6]. Ocular dissemination of cysticercus cellulose is a rare condition, although it is acknowledged. These manifestations usually involve intraocular structures (anterior and posterior segment) and extraocular tissues (extraocular muscles, orbit, subconjunctival space, eyelids, optic nerve and lacrimal gland). Intraocular cysticercosis is associated with a mediocre prognosis for vision.
The clinical signs depend on the location, size, involved structures, stage of the cyst, the number of lesions and host immune response. Anterior chamber cysticercosis is an unusual presentation; the occurrence of a live free-floating cyst in the anterior chamber is highly unlikely, with very few sporadic case reports of intracameral cysticercosis in literature. The route entry of the cyst in the anterior chamber is debatable. It can enter the anterior chamber from the posterior segment through the pupil in aphakia, through vessels supplying the ciliary body or through the anterior chamber angle. Ocular cysticercosis commonly occurs in children ages 10-20, with no definite gender predilection. The cyst may be adherent to the adjacent structures like the iris, anterior lens capsule or corneal endothelium by a stalk, or rarely remains freely floating in the anterior chamber as was described in our patient. The patient remains asymptomatic if the cyst is small or may present with complaints of diminution of vision, floater or leukocoria. Intraocular cysticercosis is diagnosed through Slit Lamp examination; as the cysts can be easily detected.
The presence of a scolex in a cystic lesion usually is suggestive in diagnosing cysticercosis. Imaging studies are the most beneficial in establishing the diagnosis. High resolution ultrasonography (USG), computed tomography (CT) and magnetic resonance imaging (MRI) help in detection of the orbital cyst. CT and MRI imaging are important not only to confirm the diagnosis, but also to rule out the involvement of the CNS (neurocysticercosis) [7, 8].
Stool examination for the adult worm may be performed in cases of suspected cysticercosis as was obtained in our patient. A high index of suspicion along with characteristic features on imaging helps us diagnose and initiate appropriate treatment depending upon the site of involvement. Differential diagnosis to be highly considered are: hydatid cysts, orbital pseudotumor or idiopathic myositis9. Medical therapy is the recommended treatment for the extraocular muscle form and retro-orbital cysticercosis. Surgical removal is advocated for subconjunctival and eyelid cysticercosis. In the case of intraocular cysticercosis; initial treatment is indicated with surgical removal of the cyst to avoid a severe intraocular reaction caused by killing the living parasite. After surgical intervention, medical antiparasitic treatment has proven to be effective [11, 12].
4. Conclusions
Cysticercosis is an avoidable and irradicable cause of blindness, related to inappropriate self-hygiene. Diagnosis of cysticercosis is based mainly on orbital imaging because of its specific appearance. Despite resolution of cysticercosis with medical therapy or surgery such as sub conjunctival and eyelid cysticercosis, however the vast majority of patients may have long-term functional deficits due to the induced inflammation. Appropriate sanitation and personal hygiene are important in control of fecal contamination of water and food.
References
- Schantz PM. Taenia solium cysticercosis: an overview of global distribution and transmission. Chapter in Taenia Solium cysticercosis. From basic to clinical science. CABI Publishing (2002): 63-74.
- CDC - Centers for Disease Control. Prevention. Cdc – cysticercosis (2019).
- Garcia HH. Neurocysticercosis. Neurol Clin 36 (2018): 851-864.
- Chowdhurys, Sinha P, Naeveen AK, et al. Cysticercosis: An emerging parasitic disease. American Family Physician 76 (2007): 91-96.
- Atul Kumar, Kumar Hem, Mallika T, et al. Socio-demographic trends in ocular cysticercosis. Acta Ophthalmologica Scandinavica 73 (1995): 438-441.
- Del Brutto OH, Rajshekhar V, White AC, et al. Tsang Diagnostic criteria for neurocysticercosis, Neurology 57 (2001): 177-183.
- Reddy DS, Volkmer R. Neurocysticercosis as an infectious acquired epilepsy worldwide. Seizure 52 (2017): 176-181.
- Dhiman R, Devi S, Duraipandi K, et al. Cysticercosis of the eye. Int J Ophthalmol 10 (2017): 1319-1324.
- Wandra T, Ito A, Yamasaki H, et al. Taenia solium cysticercosis, Irian Jaya, Indonesia. Emerg Infect Dis (2003).
- Lorenzo Z, Marianne S, Filippo B, et al. Epidemiology and Management of Cysticercosis and Taenia solium Taeniasis in Europe, Systematic Review 1990-2011. PLoS One 8 (2013): e69537.
- Javier B, Silvia R, Juan J, et al. Detection of Taenia solium Taeniasis Coproantigen Is an Early Indicator of Treatment Failure for Taeniasis. Clinical and vaccine immunology 19 (2012): 570-573.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
