Imaging in Splenic Pathologies: A Pictorial Review
Article Information
Gurpreet Singh Sandhu1, Lokesh Singh2*, Uma Debi3, Pratyaksha Rana1, Vikas Bhatia3, Sandhu M S4
1Senior resident, Department of Radiodiagnosis and Imaging, PGIMER, Chandigarh, India
2Pool officer, Department of Radiodiagnosis and Imaging, PGIMER, Chandigarh, India
3Associate Professor, Department of Radiodiagnosis and Imaging, PGIMER, Chandigarh, India
4Professor and head, Department of Radiodiagnosis, PGIMER, Chandigarh, India
*Corresponding Author: Dr. Lokesh Singh, Pool officer, Department of Radiodiagnosis and Imaging, PGIMER, Chandigarh, India
Received: 03 November 2020; Accepted: 27 November 2020; Published: 10 December 2020
Citation: Gurpreet Singh Sandhu, Lokesh Singh, Uma Debi, Pratyaksha Rana, Vikas Bhatia, Sandhu M S. Imaging in Splenic Pathologies: A Pictorial Review. Archives of Clinical and Medical Case Reports 4 (2020): 1234-1247.
View / Download Pdf Share at FacebookAbstract
Splenic lesions are uncommon and encountered less commonly than pathologies of other visceral organs. However radiological evaluation and diagnosis of these lesions using ultrasound, Computed tomography and Magnetic resonance imaging has good specificity in differentiating congenital, benign and malignant lesions. The purpose of this pictorial essay is to offer a review of the common and uncommon splenic pathologies and illustrating the typical imaging features of these lesions.
Keywords
Spleen; USG; CT; MRI; Congenital; Benign; Malignant; Miscellaneous
Article Details
1. Introduction
Spleen as an organ is overlooked however careful evaluation while imaging can help us give important clue to diagnosis of different pathologies such as malignancy, hematologic disorders, infection, abdominal trauma, portal hypertension and miscellaneous conditions. The lesions involving spleen can be solitary or multiple [1]. In addition, congenital anomalies of the spleen, anatomical variants and rare anomalies such as asplenia and polysplenia syndrome are important to recognize along with awareness of the associated complex findings [2].
|
Congenital Lesions And Anatomical Variants. |
Cleft, notch, lobulation, Accessory spleen, Wandering spleen, Polysplenia, Asplenia. |
|
Benign Lesions |
Cysts, Echinococcal cyst, Abscess, Tuberculosis, haemangioma, lymphangioma, Hamartoma, pseudocyst, mesenchymal tumours). |
|
Intermediate And Malignant Lesions |
Angioma, haemangiopericytoma, Inflammatory myofibroblastic tumour, Lymphoma), Angiosarcoma, Metastasis and Kaposi sarcoma. |
|
Miscellaneous |
Siderosis, Trauma, Infarction. |
Table 1: Various splenic lesions.
2. Congenital Lesions and Anatomical Variants
2.1 Splenic lobulation, cleft and notches
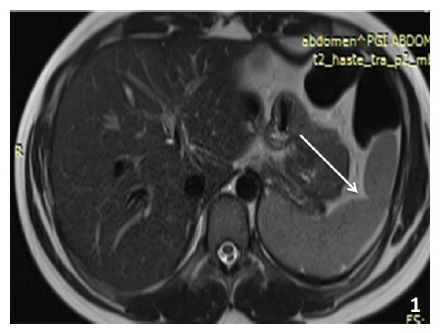
There are lobulations seen in fetal spleen which however normally would disappear before birth [3]. In some cases, it may persist till later age and is a normal variant. These are usually located on the medial part of spleen [4]. On the superior border of adult spleen generally notches or clefts are seen which are remnants of the grooves that separate the fetal lobules. The clefts usually have a well defined margin and can extend 2-3 cm deep within the parenchyma (Figure 1) and may be falsely diagnosed as laceration.
2.2 Accessory spleen
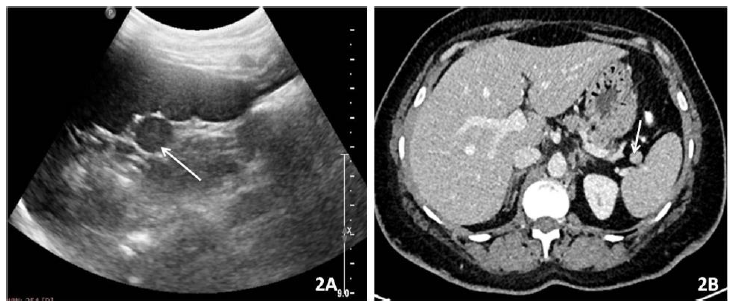
An accessory spleen is a normal splenic tissue which is discrete from the main splenic body which results due to the failure of fusion of splenic anlage [5]. They are asymptomatic, found incidentally and should not be misdiagnosed as lymphadenopathy [6]. Its detection is important in patients with hematologic or autoimmune disorder planned for splenectomy so that all the functional splenic tissue is removed [7-9]. They are usually spherical in shape ranging from few millimeter to centimeter and have well-defined borders (Figure 2A and 2B). Common locations include splenic hilum and tail of pancreas with other uncommon locations being along the splenic vessels, gastrosplenic and splenorenal ligaments. The characteristic of splenunculus is that they enhance homogeneously and show similar density or intensity to that of adjacent splenic parenchyma on CT and MRI respectively [10].
2.3 Wandering spleen
Wandering spleen, also known as ectopic spleen is the presence of spleen at a site different from the usual in left upper quadrant. It can be both congenital and acquired in etiology and results from migration of the spleen caudally in abdomen or pelvis due to laxity or maldevelopment of the supporting splenic ligaments with most common location being the left mid abdomen [11]. The various acquired causes of laxity of ligament include the hormonal effects of pregnancy, and abdominal wall laxity [12-14]. It is usually seen in age group between 20 and 40 years and is more common in women. Acute torsion is the major complication encountered and is a surgical emergency [15]. The diagnostic feature on CT finding would be absent spleen in its normal location with a soft-tissue mass having imaging features of normal spleen, located somewhere in the abdomen or pelvis (Figure 3). In cases of splenic torsion, the twisting of pedicle with splenic vessels and surrounding fat, known as the whirl sign is the
characteristic imaging finding [15].
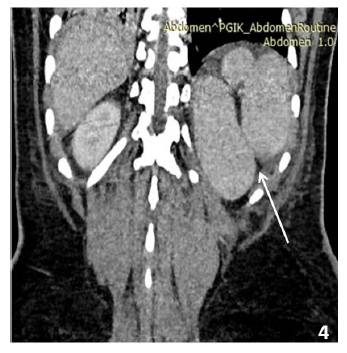
2.4 Polysplenia syndrome
Polysplenia is associated with anatomic abnormalities known as heterotaxia [16, 17] It is a complex congenital anomaly and part of spectrum of partial visceral heterotaxia (situs ambiguous) and concomitant levoisomerism. Severe cardiac anomalies are associated leading to diagnosis in early infancy [18]. Interruption of the inferior vena cava (IVC) with azygos continuation being the most frequent anomalies. There are multiple spleens in abdomen. (Figure 4).
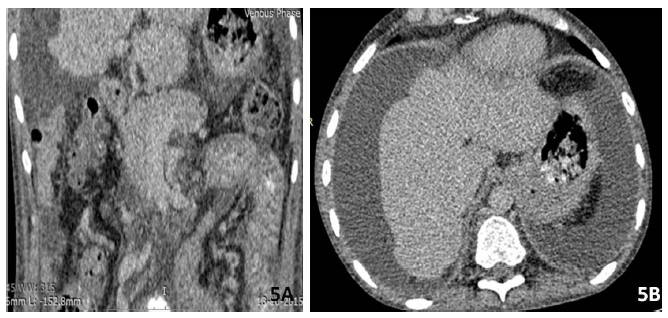
2.5 Asplenia syndrome
Asplenia is characterized by absent splenic tissue along with an abnormal arrangement of the abdominal organs with liver and gallbladder being midline in location. Congenital heart anomalies are commonly associated with it and seen in majority of patients resulting in high mortality in patients during the first year of life (Figure 5A).
3. Benign Lesions
3.1 Splenic cysts
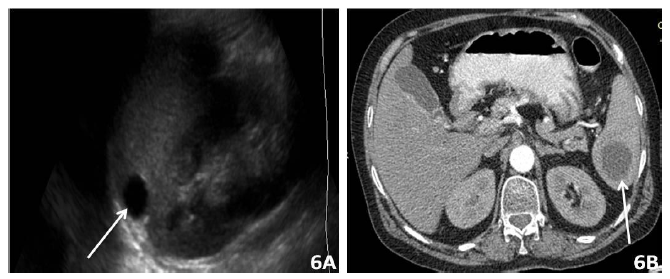
The Cysts are the commonest of the benign lesions of spleen and can be primary or acquired. Primary cysts are always true cysts lined by a epithelium membrane. They are simple, uniloculated or septated and may show punctate calcifications. The acquired cyst have no cellular lining and can be secondary to trauma or sequelae of splenic infarction and abscess. Simple cysts are sharply demarcated lesion as seen as anechoic lesion on USG, and show low density on CT and bright on T2 WI in MRI. No post contrast enhancement is seen [20-22]. (Figure 6A, B, C and D).
3.2 Echinococcal cysts:
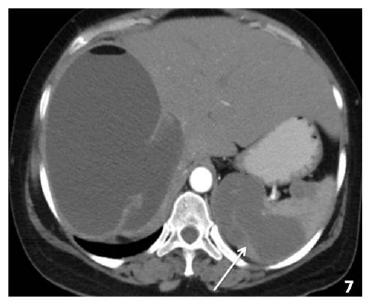
The involvement of spleen by echinococcus granulosa is rare and seen in 1-3 % cases of hydatid disease. The cyst consists of pericyst, derived from the host tissue, ectocyst, which is the acellular laminated membrane and the innermost endocyst which gives rise to daughter cyst. The cysts can be large and unilocular or multilocular in appearance. Typically the daughter cysts are arranged peripherally and are less dense on CT and compared to fluid in the parent cyst (Figure 7). A “snake” sign can be seen due collapsed parasitic membranes within the cyst. In a dead cyst there is complete calcification of the cyst with no enhancement is seen is noted [23].
3.3 Splenic abscess
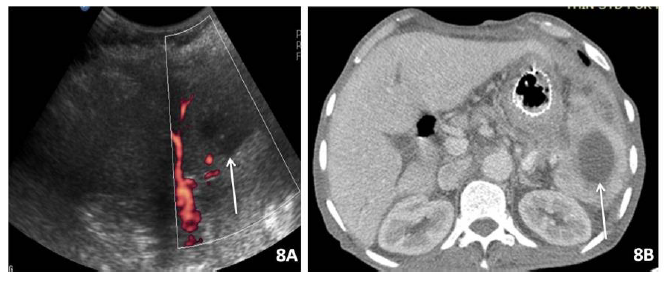
The splenic infection is more common in patients with immunodeficency, post splenic trauma s, and sickle cell disease and presents with left upper quadrant pain, fever, and raised blood counts There can be single or multiple liver abscesses. Splenic abscess may be unilocular and represent bacterial etiology or can be multilocular which may be due to fungal or mycobacterial cause. On USG (Figure 8A) it appears as low echogenicity lesion with complex internal echoes. On CT, it is seen usually as a spherical hypodense (20 to 40HU) lesion with thick shaggy wall and shows peripheral enhancement which however can lack in some cases (Figure 8B). On MRI its is hyperintense on T2 and show restricted diffusion on DWI. Gas or air bubbles may be also seen [24-26]
3.4 Splenic tuberculosis
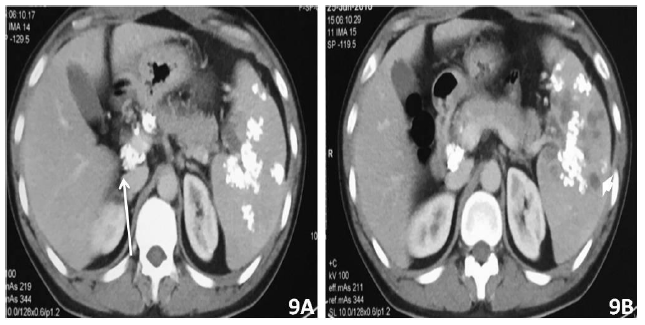
Spleen is commonly affected organ in patients with disseminated miliary tuberculosis [27]. On imaging there may be mild splenomegaly, enlarged abdominal lymph nodes with central necrosis, ascites with peritoneal thickening. There are usually multiple small lesions or can be a single large lesion. On Ultrasound these lesions are generally hypoechoic to anechoic with ill defined margins [28]. On CT they appear as hypodense lesions and chronic/treated cases may show calcification (Figure 9A and 9B).
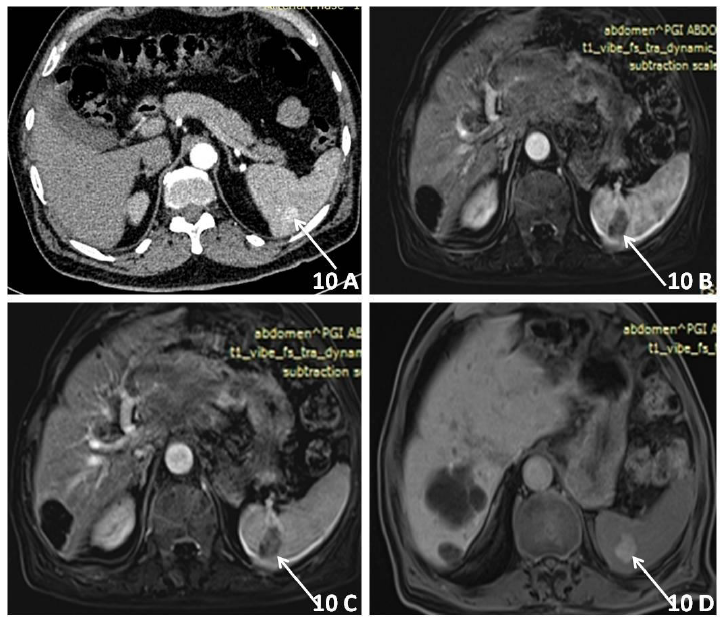
3.5 Splenic haemangioma
Hemangioma is characterized by vascular channels of varying sizes and is the most common benign tumour of spleen. It can be solitary, multiple or can present with diffuse splenic involvement as in kasaback -Merrit syndrome, which is also associated with abnormalities including anemia, thrombocytopenia, and consumptive coagulopathy. They are usually solid or mixed solid cystic lesion and appear hyperechoic on USG and may show scattered or punctate calcification. On Non contrast CT they appear as hypodense and on T2WI MRI appear hyperintense. On post contrast study they show centripetal enhancement with gradual filling on delayed phase. However the classical peripheral nodular discontinuous enhancement is less commonly seen [29-31]. (Figure 10 A, B, C and D).
3.6 Splenic lymphangioma
It is a uncommonly encountered lesion and is generally in younger patients occuring mostly as multiple splenic lesions. Rarely the complete parenchyma may be involved suggestive of lymphangiomatosis. They may be associated with lymphangiomas in other sites such as neck mediastinum and axilla. Various pathologies have been postulated for their development from hamartomatous, neoplastic to congenital defect of lymphatics [32]. On imaging, they appear as well defined, uni or multilocular cystic lesion with thin septations and are commonly encountered in subcapsular location. Calcification can be seen. On MRI the lesion are bright on T2 and may appear bright on T1w images due to proteinaceous fluid or hemorrhage [33].
3.7 Splenic hamartoma
Hamartoma is a mass of malformed splenic red pulp elements with no organized lymphoid follicles. They are generally solitary and can be as large as 20 cm in diameter and are mostly asymptomatic [34]. They are well circumscribed solid lesions and show homogenous to heterogenous echogenicity with occasional areas of calcification within. On MRI, hamartomas are usually isointense on TI-weighted images and heterogeneously hyperintense on T2-weighted images. with a hypoitense capsule around it. On post contrast study on CT and MRI lesion shows heterogenous enhancement with diffuse early enhancement that helps to differentiate from haemangioma [35]. There may be central non-enhancing areas seen within suggestive of necrosis.
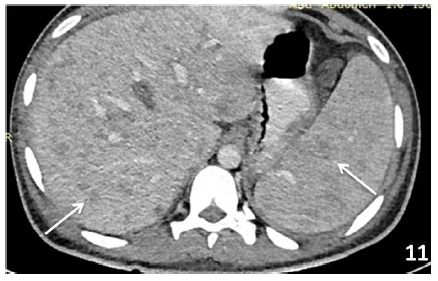
3.8 Malignant
3.8.1 Splenic Lymphoma: Lymphoma is one of the most common malignancies of spleen. The involvement of the spleen and/or splenic hilar nodes individually is defined as primary splenic lymphoma and usually is non-Hodgkin type of lymphoma [34]. Secondary spread of disease to the spleen occurs commonly in both Hodgkin and non-Hodgkin lymphoma and is much more common than primary lymphoma. On imaging there is homogeneous enlargement of spleen with multiple small nodules generally around 1 cm in size and less likely may present as single solitary mass [36] (Figure 11). They are generally hypodense on CT and on MRI appears as isointense with spleen on T1- and T2-weighted images which differentiates them from metastasis which are hyperintense on T2 [37].
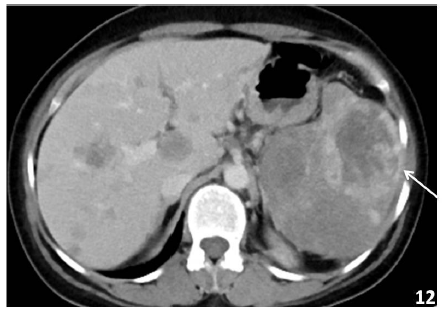
3.8.2 Angiosarcoma: Mesenchymal tumour of vascular origin are most common primary tumour of spleen and are rarely encountered. Hemangioendothelioma has borderline malignant potential wheras angiosarcoma refers to the malignant type of vascular tumour [34]. They are highly aggressive lesions with high mortality rate. On Imaging splenic angiosarcoma appear as large heterogeneous lesions sometimes completely replacing most of splenic parenchyma. Lesions vary in size and may show areas of necrosis, acute hemorrhage, hemosiderin deposits, or calcification (Figure 12). Metastases are frequently present at the time of diagnosis [38].
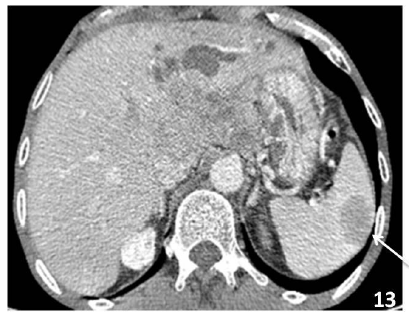
3.8.3 Metastasis: The metastasis to spleen is rare and usually seen in advanced malignant disease with poor prognosis. The most common sites for metastases to spleen are from lymphoma and melanoma, followed by carcinoma of the ovary, breast, lung, stomach, prostate and colon [39, 40] (Figure 13).
3.9 Miscellaneous
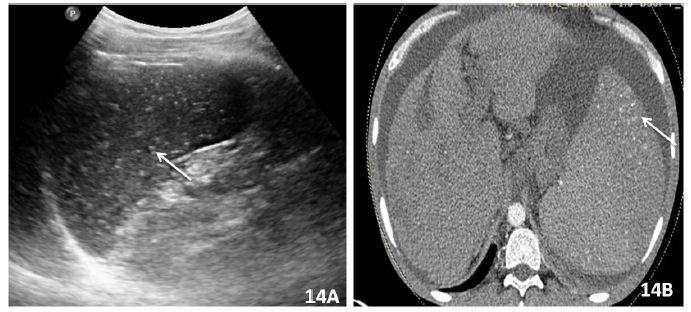
9. 1 Siderosis: Portal hypertension is in late stages is associated with splenomegaly. In addition there are, multiple tiny foci of hemosiderin deposits also named as Gamma-Gandy bodies are seen in 9 to 12% of patients with portal hypertension. These foci on USG appear as tiny hyperechoic foci. On CT they appear as hyperdense and MRI as low SI on all sequences with “blooming” on gradient echo sequences secondary to iron deposition [41] (Figure 14).
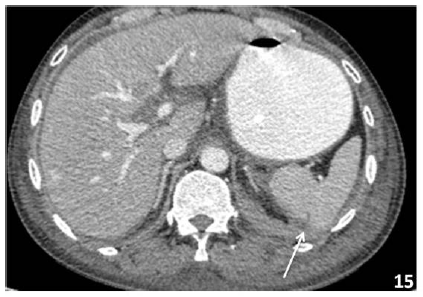
3.9.2 Splenic trauma: Ultrasound can be used for screening of splenic trauma with hypoechoic to illdefined anechoic areas may be seen in the splenic parenchyma suggestive of either contusion or lacerations. A subcapsular haematoma or perisplenic fluid may also indicate splenic injury. However Computed-tomography is the gold standard for diagnosis of splenic trauma and grading of injury [42] (Figure 15).
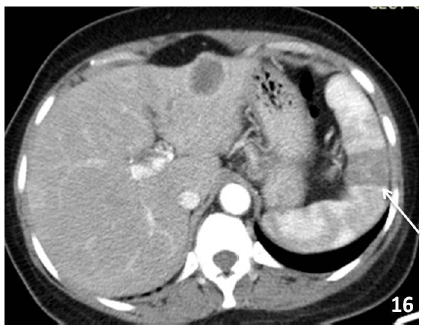
3.9.3 Splenic infarct: Infarct are caused due to ischaemic insult to the spleen and associated with haematological disorders,hypercoagulable states, emlbolic event or post trauma sequale. They usually appears as wedge shaped, peripheral hypoechoic or hypodense on USG and CT repectively. No internal vascularity or enhancement is seen within the affected area [43] (Figure 16).
4. Conclusion
A wide range of abnormalities can involve spleen and imaging plays a key role in identification of these pathologies. These findings can help in correct diagnosis and guiding management of splenic pathologies.
References
- Liliana Chiorean, Mihnea Zdrenghea, Radu Badea. Ultrasonography of the spleen. Pictorial essay. Med Ultrason 16 (2014): 48-59.
- Gayer G, Hertz M, Strauss S, et al. Congenital Anomalies of the Spleen. Semin Ultrasound CT MRI 27 (2006): 358-369.
- Moore KL, Persaud TVN. The digestive system, in Moore KL, Persau: The Developing Human (ed 7). Clinically Oriented Embryology. Philadelphia, PA, Saunders (2003): 256-285.
- Mortele KJ, Mortele B, Silverman SG. CT features of the accessory spleen. AJR Am J Roentgenol 183 (2004): 1653-1657.
- Freeman JL, Jafri SZ, Roberts JL, et al. CT of congenital and acquired abnormalities of the spleen. Radiographics 13 (1993): 597-610.
- Gayer G, Apter S, Jonas T, et al. Polysplenia syndrome detected in adulthood: report of eight cases and review of the literature. AbdomImaging 24 (1999): 178-184.
- Facon T, Caulier MT, Fenaux P, et al. Accessory spleen in recurrent chronic immune thrombocytopenic purpura. Am J Hematol 41 (1992): 184-189.
- Budzynski A, Bobrzynski A, Sacha T, et al. Laparoscopic removal of retroperitoneal accessory spleen in patient with relapsing idiopathic thrombocytopenic purpura 30 years after classical splenectomy. SurgEndosc 16 (2002): 1636.
- Napoli A, Catalano C, Silecchia G, et al. Laparoscopic splenectomy: multi-detector row CT for preoperative evaluation. Radiology 232 (2004): 361-367.
- Elsayes KM, Narra VR, Mukundan G, et al. MR imaging of the spleen: spectrum of abnormalities. Radiographics 25 (2005): 967-982.
- Gayer G, Zissin R, Apter S, et al. CT findings in congenital anomalies of the spleen. Br J Radiol 74 (2001): 767-772.
- Paterson A, Frush DP, Donnelly LF, et al. A pattern-oriented approach to splenic imaging in infants and children. Radiographics 19 (1999): 1465-1485.
- Heydenrych JJ, Du Toit DF. Torsion of the spleen and associated “prunebelly syndrome”. A case report and review of the literature. S Afr Med J 53 (1978): 637-639.
- Gilman RS, Thomas RL. Wandering spleen presenting as acute pancreatitis in pregnancy. Obstet Gynecol 101 (2003): 1100-1102.
- Raissaki M, Prassopoulos P, Daskalogiannaki M, et al. Acute abdomen due to torsion of wandering spleen: CT diagnosis. Eur Radiol 8 (1998): 1409-1412.
- Bartram U, Wirbelauer J, Speer CP. Heterotaxy syndrome—asplenia and polysplenia as indicators of visceral malposition and complex congenital heart disease. Biol Neonate 88 (2005): 278-290.
- Marx MV, Van Allan R. SIR 2005 film panel case: heterotaxia with polysplenia. J Vasc Interv Radiol 16 (2005): 1055-1059.
- Winer-Muram HT, Tonkin IL. The spectrum of heterotaxic syndromes. Radiol Clin North Am 27 (1989): 1147-1170.
- Fulcher AS, Turner MA. Abdominal manifestations of situs anomalies in adults. Radiographics 22 (2002): 1439-1456.
- Goerg C, Schwerk WB, Goerg K. Sonography of focal lesions of the spleen. AJR Am J Roentgenol 156 (1991): 949-953.
- Balzan SM, Riedner CE, Santos LM, et al. Posttraumatic splenic cysts and partial splenectomy: report of a case. Surg Today 31 (2001): 262-265.
- Giovagnoni A, Giorgi C, Goteri C. Tumors of the spleen. Cancer Imaging 5 (2005): 73-77.
- Polat P, Kantarci M, Alper F, et al. Hydatid disease from head to toe. Radiographics 23 (2003): 475-494 quiz 536-477,.
- Chang K-C, Chuah S-K, Changchien C-S, et al. Clinical characteristics and prognostic factors of splenic abscess: a review of 67 cases in a single medical center of Taiwan. World J Gasteroenterol 12 (2006): 460-464.
- Chun CH, Raff MJ, Contreras L. Splenic abscess. Medicine 59 (1980): 50-65.
- Ng KK, Lee TY, Wan YL, et al. Splenic abscess: diagnosis and management. Hepatogastroenterology 49 (2002): 567-571.
- Choi BI, Im JG, Han MC, et al. Hepatosplenic tuberculosis with hypersplenism: CT evaluation. Gastrointest Radiol 14 (1989): 265-267.
- Tarantino L, Giorgio A, de Stefano G, et al. Disseminated mycobacterial infection in AIDS patients: abdominal US features and value of fine needleaspiration biopsy of lymph nodes and spleen. Abdom Imag 28 (2003): 602-608.
- Abbott RML, Angela D, Aguilera NS, et al. Primary vascular neoplasmsof the spleen: radiologic-pathologic correlation. Radiographics 24 (2004): 1137-1163.
- Pakter RL, Fishman EK, Nussbaum A, et al. CT findings in splenic hemangiomas in the Klippel-Trenaunay-Weber syndrome. J ComputAssist Tomogr 11 (1987): 88-91.
- Ros PR, Moser RP Jr, Dachman AH, et al. Hemangioma of the spleen: radiologic-pathologic correlation in ten cases. Radiology 162 (1987): 73-77.
- Morgenstern L, Bello JM, Fisher BL, et al. The clinical spectrum of lymphangiomas and lymphangiomatosis of the spleen. Am Surg 58 (1992): 599-604.
- Komatsuda T, Ishida H, Konno K, et al. Splenic lymphangioma: US and CT diagnosis and clinical manifestations. Abdom Imag 24 (1999): 414-417.
- Warnke RA, Weiss LM, Chan JKC, et al. Tumors of the lymph nodes and spleen, third series ed. Washington, DC, Armed Forces Instituteof Pathology (1995).
- Ramani M, Reinhold C, Semelka RC, et al. Splenic hemangiomas and hamartomas: MR imaging characteristics of 28 lesions. Radiology 202 (1997): 166-172.
- Fishman EK, Kuhlman JE, Jones RJ. CT of lymphoma: spectrum of disease. Radiographics 11 (1991): 647-669.
- Elsayes K, Narra V, Mukundan G, et al. MR imaging of the spleen: spectrum of abnormalities. Radiographics 25 (2005): 967-982.
- Thompson W, Levy A, Aguilera N, et al. Angiosarcoma of the spleen: imaging characteristics in 12 patients. Radiology 235 (2005): 106-115.
- Andrews MW. Ultrasound of the spleen. World J Surg 24 (2000): 183-187.
- Wan YL, Cheung YC, Lui KW, et al. Ultrasonographic findings and differentiation of benign and malignant focal splenic lesions. Postgrad Med J 76 (2000): 488-493.
- Aya Kamaya, Stefanie Weinstein, Terry S Desser. Multiple Lesions of the Spleen: Differential Diagnosis of Cystic and Solid Lesions. Semin Ultrasound CT MRI 27 (2006): 389-403.
- McKenney KL, Nuñez DB Jr, McKenney MG, et al. Sonography as the primary screeningtechnique for blunt abdominal trauma: experience with 899 patients. AJR Am J Roentgenol 170 (1998): 979-985.
- Goerg C, Schwerk WB, Goerg K. Sonography of focal lesions of the spleen. AJR Am J Roentgenol 156 (1991): 949-953.



 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
