Can Operating Room Efficiency be Increased by Applying the Lean Six Sigma Models?
Article Information
Lorenzo Michelin1,3 *, Beatrice Ricci2, Venerando Barbagallo3, Peter Perger4, Emanuele Padovani5, Federico Giardina6, Francesco Traina6,7, Anselmo Campagna3, Viola Damen3, Matteo Buccioli3
1Economist specialized in healthcare management and economics, University of Bologna, Italy
2Resident at School of Hygiene and Preventive Medicine, University of Bologna, Italy
3Rizzoli Orthopaedic Institute, Bologna, Italy
4PhD Student at UMIT – Private University for Health Sciences, Medical Informatics and Technology, Hall in Tirol, Austria
5Professor, Department of Business science, University of Bologna, Italy
6Hip and Knee Surgery Department, Rizzoli Orthopaedic Institute, Bologna, Italy
7Joint Professor, Department of Medicine, Universities of Messina and Bologna
*Corresponding Author: Lorenzo Michelin, Research fellow at Rizzoli Orthopaedic Institute, Bologna, Italy.
Economist specialized in healthcare management and economics, University of Bologna, Italy
Received: 27 April 2021; Accepted: 28 June 2021; Published: 21 July 2021
Citation: Lorenzo Michelin, Beatrice Ricci, Venerando Barbagallo, Peter Perger, Emanuele Padovani, Maurizia Rolli, Federico Giardina, Francesco Traina, Matteo Buccioli. Can Operating Room Efficiency be Increased by Applying the Lean Six Sigma Models? Archives of Clinical and Medical Case Reports 5 (2021): 549-558.
View / Download Pdf Share at FacebookAbstract
Executive summary This study was inspired by Operating Room efficiency studies and the growing use of management models established in the manufacturing sector, applied to the management of operating rooms. Furthermore, as these models are theoretical guidelines, the study will attempt to discuss their key concepts and application in the hospital sector.
The objective of the study is to understand if and how management models have been useful to improve the efficiency of operating theatres. Since operating theatres are a sector that mobilizes large amounts of resources and can be considered the production line of the hospital, it is useful to apply new organizational models to increase performance. To this end, data concerning operating theatres before (2018) and after the reorganization (2019) have been compared, inspired by the concepts of efficiency studied by Macario, the monitored data have been calculated using performance indicators using time as the main measure.
The hospital made an organizational change that led to reorganizing the OR schedule according to Lean Six Sigma management models. This has led to a change in the allocation of surgical sessions. In 2018 there was a prevalence of short OR (parallel) sessions in the mornings, while in 2019 a prevalence of (consecutive) sessions mornings and afternoons for the same surgical units. In 2019 an attempt was also made to group similar cases in the same session in order to standardize the process and reduce variability. The KPI values considered in the study show an improvement in performance and use of resources.
Keywords
Efficiency; OR scheduling; Working study; Overtime; Lean-Six-Sigma
Efficiency articles; OR scheduling articles; Working study articles; Overtime articles; Lean-Six-Sigma articles
Article Details
1. Introduction
Efficiency is one of the main targets of hospital management, in order to reduce costs while maintaining the level of quality standard and accessibility to the service for patients. Accessibility can be limited by several factors. The concept of efficiency considered in this study will be identified as the possibility of increasing the service while leaving the quality and resources available unchanged. The action will then be focused on creating an organizational change capable of reducing the value of resources not properly exploited to increase the number of patients served.
“The operating room (OR) is the financial nexus of the modern hospital, accounting for up to 40% of a hospital’s costs and 60-70% of revenue” [1].
Moreover, efficiency in the OR is directly connected and relevant to triggering a decrease in waiting lists and an increase in service provisions. In summary, we could state that OR efficiency is achieved when the service is performed at the right time without incurring excessive waiting times and costs, thus optimizing the use of medical resources in order to achieve maximum profitability. Another way to withstand the financial pressure on budget is to limit internal costs and decreasing inpatient length of stay. Unfortunately, the former is not always practicable without a notable reduction on the quality of the services provided, the latter is less effective in terms of costs savings if the OR is not efficient.
Applying new management strategies to increase the efficiency in the OR, the main objective of hospital management can be summarized in:
- maximizing revenue, by increasing the number of surgical cases performed without increasing the associated costs;
- maintaining and raising quality and safety standards;
- increasing the satisfaction of medical staff and patients treated [2].
The Italian national health system is facing difficulties with service provision, both because of an inability to expand the service due to a lack of budget and medical staff, and on the demand side, which has increased due to a large part of the population being elderly and chronically ill [3, 4]. [ISTAT 2017].
In order to respond to patients’ needs, the hospital has implemented specific strategies to reduce waiting times and increase efficiency in the use of resources. The following study aims to determine the effects on productivity and efficiency, as a result of an organizational change in the allocation of operating theatres and standardization in the planning of patients in the operating session.
2. Materials and Methods
2.1 Instruments
The choice of this reform in the organization was guided by two management models, Lean method and Six Sigma. The first one, inspired by the Japanese philosophy of Kaizen (continuous improvement), aims to make the process standard and fluid. While the Six Sigma was used applying the DMAIC process (Define, Measure, Analyze, Improve and Control) and to identify the MUDA (functions that do not create value but consume resources). Through the six-sigma model we have identified the MUDAs with the under-use and over-use times of the operating room, this choice is due to the centrality of time in our research, other examples of MUDAs can be little used instruments, inefficient but expensive procedures etc. Following the Lean model, the operating slots have been organized consecutively with long OR sessions, and an attempt has been made to standardize the visits allocated in the slot, in order to standardize the process, reduce unforeseen events and increase productivity [5].
In order to have a measure of both efficiency and economic value we have chosen time as the main measure. For this purpose, the operating room will always be considered with allocated staff [6]. The reorganization implemented is a change in the operating room schedule, time is allocated to the operating theatres in 380 min time slots, which can be allocated in parallel in two rooms or consecutively in the same room. In 2018 two short OR morning sessions managed in parallel were used in the Hip and Knee Prostheses Unit (HKPU), while in 2019 the solution used is a single long OR in which both morning and afternoon sessions are used. In addition to this reorganization of operating room time there is also a reorganization of the operating room schedules, in fact in 2019 the cases of joint replacements supposed to be easier and with few co-morbidities are put in sequence to increase productivity per allocated slot.
The KPIs that have been taken into consideration are: (STT) start time tardiness, (OT) over time, (TT) turnover time, (RU) raw utilization, (UU) underutilization and (N°) number of operations for each time slot allocated and average time for induction tasks [7]. The surgical process is determined by the sum of all the necessary tasks, and the efficiency is achieved when it is possible to minimize the time required without changing the quality of the service. In considering the efficiency of service we have also taken into account the satisfaction of patients and doctors. In fact, the intention is to reduce waiting times for patients and workload for health professionals (overtime) [2, 8]. Time in OR is never considered lost but is allocated to other activities and efficiency is the harmony between the different activities to be carried out.
These indicators were considered in terms of standard mean, standard deviation and frequency, a more detailed description of the formulas and indicators is present in the glossary at the end of the paper. In addition, 5 categories of surgical procedures have been identified, i.e., in order to use the tracer cases to define the performance for each type of surgery. In order to measure the impact of this organizational choice, two types of activities are distinguished and measured through KPIs, activities that use the OR beyond the estimated time and the amount of underutilization of the OR. The choice to consider under-utilization and over-utilization is explained by the fact that in both cases we have extra costs [9].
In order to make the direct data comparable, KPIs have been included in the formula derived by Macario’s studies on inefficient time and statistical surgery scheduling, to minimize inefficiency of OR use applying optimal planning that balances under and over utilization [6].
Inefficient use of OR time = (hours of under-utilized time) + (hours of over utilized time) x 2.
The other tools used in the research are management models, which have been used to establish the most correct process, the measurement procedure and the identification of inefficient processes.
2.2 Sample selection
For the study a single Unit was selected, HKPU, both to have a simplified usage case and because waiting lists for joint replacements are particularly critical in our environment. Furthermore, in terms of volume of costs generated and value of services provided, it is an essential unit in terms of contribution margin for the hospital. The study was developed in ex post form. We performed a retrospective observational analysis comparing cases performed in eligible OR within the 6-month pre- (from January 2018 to June 2018 and post- (January 2019 to June 2019) intervention periods, in this regard 2018 is considered the control group (t0), while 2019 is the treatment group (t1).
The data analysis was done using Excel and raw data comes from an Excel extraction provided by the digital system implemented in the hospital. In order to reduce endogenous factors and data deviating between the two years, some assumptions were made. The data taken into consideration concern only the prosthetic surgery unit, in order to consider the same case mix, moreover, in order to limit abnormal data, weeks of emergency availability, strikes and weeks of reduced service were eliminated. These eligibility criteria have made possible to consider the case mix and the expected service constant between (t0) and (t1). The data selection was complemented by an additional manual data cleaning process, patients with incorrect or incomplete data were not considered, only patients with complete data were used to compute the KPI results, while all patients treated in the allocated slots were considered to determine the number of operated patients.
(The total number of operations considered are 457 in (t0) 421 in (t1), and to evaluate KPI 445 operations in t0 and 415 in t1 were counted.). In 2018 (t0), we have a prevalence of 2 SHORT OR, for a total of 760 min of OR allocated in the morning section, organized in parallel with 2 different teams. On 2019 (t1), there is a reorganization with only 1 LONG OR where the two teams work consecutively. To evaluate the difference in assigned slots we considered the short operating room as X while the long operating room 2X, with X=380min. As is seen in (Table 1) there are no significant differences between t0 and t1, however, t1 has a lower amount of resources allocated, one day less (89 days) and fewer slots assigned.
|
YEAR |
OR TYPE |
OR HOURS ALLOCATED |
OR HOURS USED |
N° SLOTS ALLOCATED |
N° SUGERIES PERFORMED |
|
2018 |
SHORT |
760:00:00 |
599:37:00 |
120 |
334 |
|
LONG |
329:20:00 |
202:00:00 |
26 |
123 |
|
|
TOT |
1089:20:00 |
801:37:00 |
172 |
457 |
|
|
2019 |
SHORT |
133:00:00 |
96:54:00 |
21 |
58 |
|
LONG |
899:20:00 |
652:12:00 |
71 |
363 |
|
|
TOT |
1032:20:00 |
749:06:00 |
163 |
421 |
Table 1: Shows how hours were allocated/used in the OR in the two periods (2018) and (2019), showing the difference in allocated slots and the resulting number of operations performed per room type in each year.
3. Results
3.1 Case mix
Among the external factors that can influence performance we find the presence of a more complex case mix and therefore the distribution of the pathologies treated over the two years has been compared. The distribution of cases is different between (t0) and (t1) (Graph1), the case mixes in (t1) have a prevalence of surgeries that consume on average more operating room time. From the interview with the general practitioners, has been understood that the revision surgeries are more complicated than primary prosthesis, because when a prosthesis is revised the case has a bigger variability in terms of time, depending on the patient’s previous prosthesis condition and residual bone to apply the new one.
Moreover, primary knee prostheses procedures are more time consuming. It is worth saying, however, that even when the caseload was slightly more complex in 2019, this only affected efficiency in terms of the total number of operations carried out. As we can see from (Table 1) in 2019 we have 52 hours less allocated to the OR, which according to the average production values per hour of (Table 2) is equivalent to a production of at least 23 more cases. This factor, together with the more complex case mix, explains the smaller number of surgical procedures performed in (t1).
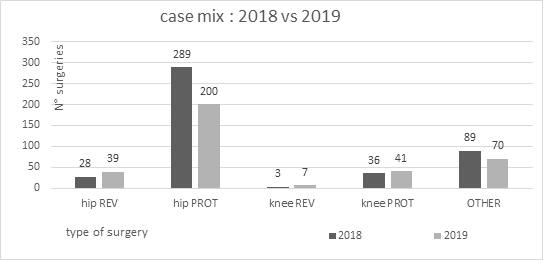
Graph 1: Shows distribution of treated pathologies between (2018) and (2019).
It is therefore evident that for time consumed, variability and number of cases the prostheses are more suitable for standardization. This evaluation together with clinical evaluations can be the starting point for selecting standard patient sample.
A further difference in terms of complication and variability of the surgery is determined by the nature of the pathology, in fact secondary arthritis can be more difficult than primary arthritis due to patient variable case history, however we must take into account that the difficulty of surgery is inversely proportional to the experience of the surgeon.
3.2 OR utilization
By checking the KPIs we can verify whether the application of these models has been useful in reducing MUDA and therefore if the time allocated has been used more efficiently. The total RU seems to have decreased slightly in 2019, the use of the long operating room improved considerably (+11%), while the short room decreased its RU. However, the total amount and the frequency of OT and UU was then counted, this highlighted the possibility that the RU in 2018 was overestimated due to more frequent use of the room beyond the allocated time (OT). Once the RU was adjusted for OT it was seen that the usage of the operating room was better in 2019 (Graph 2ta).
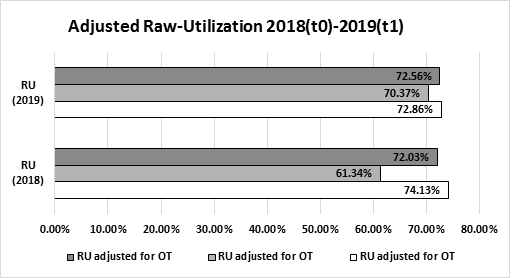
Graph 2: Shows the adjusted RU for short and long OR in (t0) and (t1).
Table 2: Collects all the KPIs taken into consideration and puts them in direct comparison between (t0) and (t1) and type of OR. The KPIs taken into consideration are: (STT) delay on the first patient of the day, (TT) time between the exit of one patient and the entry of the next, (OT) time used beyond the allocated time, (UU) unused allocated time, (OR inefficient use=hours of under-utilized time) + [(hours of over utilized time) x2. (Table 2) also shows the total number of patients operated, the average number of patients produced per slot allocated, and per hour allocated by comparing (t0) and (t11).
Through analysis the KPIs we noticed that not all performances improve in (t1), but overall values show a positive trend for efficiency (Table 2). The factors that worsen in (t1) are the delay on the first patient of the day (STT) that increase in both OR and the time between the exit of one patient and the entry of the next (TT) that remains constant for the long OR but worse for the short one, however these measures while increasing remain within an acceptable performance range.
The time used beyond the allocated time (OT) and unused allocated time (UU) indicators improve, the UU sees a substantial improvement with the long OR that halves its underutilization time and the short OR manages to improve a figure already positive in 2018. OT improves, even if it is not directly deducible from the (Table 2) numbers. In fact, the most used short room in 2018 produced a higher OT than the most used long room in 2019. In addition, in 2018 the rooms producing OT were two in parallel while in 2019 only one. The overall improvement is appreciable with the OR inefficient use index which shows a substantial improvement in 2019.
As the number of hours allocated is lower in t1, the productivity per allocated slot and the productivity per hour were compared. From (Table 2) it can be deduced that in (t1) productivity increases both for the long and short OR. Degrees of inefficiency were also compared, showing a reduction in efficiencies per slots allocated and per slot of time used. Following these results, average time and standard deviation for each pathology were tested using the 5 tracer case studies, as a way to understand how the timing for each type of operation has changed. We have seen a general improvement in surgical time for each pathology treated. In fact, the average times have improved for all types of pathology treated, except for other surgeries (Table 3). This leads us to think that there may be other factors that affect efficiency.
|
Type of surgery |
2018 (t0) |
2019 (t1) |
||
|
surgical time |
surgical time |
|||
|
average |
st dev |
average |
st dev |
|
|
Hip REV |
02:41 |
00:34 |
02:22 |
00:40 |
|
Hip PROT |
01:41 |
00:15 |
01:37 |
00:17 |
|
Knee REV |
02:31 |
00:44 |
02:28 |
00:47 |
|
Knee PROT |
02:11 |
00:19 |
02:01 |
00:24 |
|
others |
01:28 |
00:45 |
01:45 |
00:40 |
Table 3: show average time and standard deviation for each procedure in (t0) and (t1).
4. Discussion
This study on OR tries to explain how management can play a central role in the hospital’s excellence. As a matter of fact, OR is one of the most resource-consuming departments of the hospital, but at the same time, the one that can contribute the most in terms of possible margin of improvement. From the data resulting from the analysis there seems to have been an improvement in 2019 in terms of output per allocated OR hour, however the total number of interventions cannot be directly compared due to a difference in allocated hours and case mix between the two years. The RU increased slightly in 2019, which could be a sign of poor effectiveness, however, the operating theatres have benefited from a more balanced use of the two types of ORs.
Moreover, the maximization of OR efficiency is not to be understood as a point plate linked to a specific value, in fact it has been suggested by some studies that the OR is to be understood as a dynamic balance that allows us to minimize the probability of OT and UU [10]. It is therefore possible to say that there have only been benefits in terms of efficiency, resulting from the application of an operating room model in consecutive mode rather than in parallel, with the consequent halving of the times considered inefficient. However, the benefits may be overestimated, as it is natural to think that some performance has improved as a result of increased experience of surgeons (t1).
The performance of the support functions has declined, which confirms the correctness of our assessments, but raises the doubt that some functions may have adversely affected the performance of anesthesiologic operations. A more in-depth study would require analyzing what factors have changed in anesthesia operations, i.e., in order to correct any disharmony in the workflow caused by reorganization of timeslots. A further study should also take into account the aspect of staff perception, if in fact the reduction of overtime is definitely a positive aspect, but the perception of staff is not measured, studies suggest that very often the perception of staff tends to overestimate overtime [11].
What is directly perceivable by surgeons is the change of schedule and organization, if in fact the use of the long OR model is an ideal way to promote efficiency, but it can also be a reason for contrast, since the delay on the end of the first slot assigned goes to erode the time allocated to the afternoon session. Beyond the perception and the concept of efficiency, it is important to understand that reorganization has a value that can be evaluated in economic terms. In fact, by allocating the total costs for the allocated operating room hours, it is possible to evaluate the savings achieved by the reduction of even just one minute of the operating process. We can therefore say that, since the average time of operations and the number of inefficiencies has decreased, there is evidence of a reduction in absolute costs and cost per performed surgical operation [5, 12].
5. Conclusions
We can conclude this study by listing the strategy used and the benefits obtained. The long operating room seems to be a good option to reduce waste of resources caused by overuse and underuse, because inefficiency is produced by one OR instead of two. The use of a long room also allows us to put in sequence more similar cases and with less variability, creating as much as possible a standardization of work and promoting a constant rhythm. The short room instead can be extremely useful to organize the cases that are more difficult or that may have complications. However, standardization is not the solution, it is only a simplified method to organize operating sessions. The strategy of allocating cases to a specific type of room has a precise purpose, to use the long room as the main production line promoting an efficient output, while using the short OR for more complicated cases, reducing the number of delays and postponed patients in the main production line.
Finally, when considering possible future developments, the horizontal reorganization of the operating room has also been proposed as a solution to respond to the COVID-19 emergency, it follows that further reorganization will be necessary. In 2020 in fact, it will have to consider a further efficiency parameter that will be a reduction of exposure to infectious risks for operators and a higher TT to allow a more in-depth sterilization of operating rooms [13].
References
- Guerriero F, Guido R. Operational research in the management of the operating theatre: a survey. Health Care Manag Sci 14 (2011): 89-114.
- Girotto JA, Koltz PF, Drugas G. Optimizing your operating room: or, why large, traditional hospitals don't work. Int J Surg 8 (2010): 359-367.
- Rapporto Gimbe (2018).
- COAS Medici www.coasmedici.it Le Norme da rispettare nella compilazione degli Orari di Servizio dei Medici Dirigenti.
- Tagge EP, Thirumoorthi AS, Lenart J, et al. Improving operating room efficiency in academic children's hospital using Lean Six Sigma methodology. J PediatrSurg 52 (2017): 1040-1044.
- Macario A. What does one minute of operating room time cost? Journal of Clinical Anesthesia 22 (2010): 233-236.
- Macario A. Implementing operating room management science. Eur JAnaesthesiol 31 (2014): 355-360.
- Tyler DC, Pasquariello CA, Chen CH. Determining optimum operating room utilization. Anesth Analg 96 (2003): 1114-1121.
- Franklin Dexter MD, PhD, Richard H Epstein MD, Rodney D Traub PhD, et al. Making Management Decisions on the Day of Surgery Based on Operating Room Efficiency and Patient Waiting Times Anaesthesiology 101 (2004): 1444-1453.
- Wang J, Yang K. Using type IV Pearson distribution to calculate the probabilities of underrun and overrun of lists of multiple cases. Eur J Anaesthesiol 31 (2014): 363-370.
- Masursky D, Dexter F, Sheldon A, et al. Surgeons and Anesthesiologists Perceptions of Turnover Times Anesthesia and Analgesia: February 112 (2011): 440-444.
- Buccioli M, Perger P, Agnoletti V, et al. Operating Room Management Accounting: Cost Calculation Model for Operating Room Encyclopedia of Information Science and Technology (2015): 11.
- Franklin Dexter MD PhD FASA, Michelle C Parra MD, Jeremiah R Brown PhD, et al. University of Iowa, Dartmouth Geisel School of Medicine Perioperative COVID-19 Defense: An Evidence-Based Approach for Optimization of Infection Control and Operating Room Management.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
