A Pilot study on Educational Workshops for Caregivers of Patients with Brain Tumors Called AGAPE Showed its Feasibility and Indicated that it Could Help Maintain Caregiver’s Quality of Life despite the Patient’s Disease Progression
Article Information
Heloise Bourien1, Elodie Pelotte2*, Aurelie Thebault2, Claire Larible-Lefort1, Frederique Lebrun2, Elodie Vauleon1
1Department of Medical Oncology, Neuro-oncology Unit, Centre Eugene Marquis, 35042 Rennes, France
2Department of Supportive Care, Neuro-oncology Unit, Centre Eugene Marquis, 35042 Rennes, France
*Corresponding author: Elodie Vauleon, Department of Supportive Care, Neuro-oncology Unit, CENTRE EUGENE MARQUIS, 35042 Rennes, France.
Received: 11 March 2022; Accepted: 19 March 2022; Published: 29 April 2022
Citation:
Heloise Bourien, Elodie Pelotte, Aurelie Thebault, Claire Larible-Lefort, Frederique Lebrun, Elodie Vauleon. A Pilot study on Educational Workshops for Caregivers of Patients with Brain Tumors Called AGAPE Showed its Feasibility and Indicated that it Could Help Maintain Caregiver’s Quality of Life despite the Patient’s Disease Progression. Archives of Clinical and Medical Case Reports 6 (2022): 298-312.
View / Download Pdf Share at FacebookAbstract
Background: Studies have highlighted the difficulties faced by caregivers of patients with brain tumors. We created the educational workshops called AGAPE. Their aim is to explain precisely the medical aspects of brain tumors, describe resources available, and allow a moment of exchange between caregivers.
Purpose: To evaluate outcomes of AGAPE.
Methods: This was an observational uncontrolled study. Feasibility was evaluated by the caregivers’ attendance of at least 2 out of 3 monthly workshops and their satisfaction. Additional outcomes were the percentage of caregivers in favour of AGAPE sustainability and the impact on their Quality of Life (QoL) according to CarGOQoL questionnaires (Caregiver Oncology Quality of Life) between baseline before the first workshop and after the last one.
Results: From February 2015 to March 2019, 12 threemonth sessions were organized allowing 75 caregivers to participate. 84% of caregivers attended at least 2 workshops, the level of satisfaction was very high, and all caregivers responded in favor of AGAPE sustainability. 36 caregivers submitted completed questionnaires at baseline and after the last workshop attended, separated by more than 2 months. The first workshop took place mostly during or after the adjuvant treatment of their loved ones. Twothirds of their loved ones had a progressive disease after the first workshop and 21 died. Caregivers’ QoL was stable between the first and last attended workshop.
Conclusion: Our study showed that educational workshops were feasible and that they could help maintain caregiver’s QoL in the patients. Further studies are necessary to implement them in daily practice.
Keywords
Brain Tumor; Caregivers; Educational Workshops; Quality of Life
Article Details
1. Introduction
In most brain tumor patients, evolution of the disease leads to neurological and cognitive decline. Patients need daily assistance and become dependent on caregivers (spouses, partners, children, relatives and friends). Caregivers are often the primary source of support, such as nursing. If patients display neurocognitive disorders such memory loss or dyscalculia, caregivers have to conduct administrational procedures. For patients with behavioral disorders, caregivers have to maintain the social relationship [1]. The caregivers have to cope with the uncertain prognosis despite treatments, the risk of neurological sequelae or progressive changes in neurocognitive functions [2-5]. The caregivers often feel untrained and unprepared to face the adjustment to their new responsibilities and neglect their own needs [6, 7], by reducing their leisure, social and working periods [8, 9]. More than two-thirds of caregivers of patients with brain tumors experience significant stress [10-12], 10 to 50% report depressive symptoms [9] that affect their Quality Of Life (QoL) [10-13]. Patients and caregivers had questions that they considered very important but were not satisfied [14]. Several studies focused on the importance of the nature of delivery information to patients and caregivers [6, 15-17], in maintaining hope, methods of coping, and the importance of relationships [18-20]. Studies have shown that the information requested was sometimes different between patients with brain tumors and their caregivers, in particular about the crucial question of prognosis [21, 22]. Caregivers appreciated the opportunity to ask sensitive questions about prognosis without their loved one present [23]. They also wanted the opportunity to talk to someone who has been through a similar experience, coping with the changes in their social, work, and family life, to reduce their anxiety [14]. Assessing caregivers’ well-being has to take a central place in medical supportive care [9, 24, 25]. Up until now three self-administered questionnaires were developed to evaluate the QoL in the caregivers’ population: Caregiver Quality of Life Index [26], Caregiver Quality of Life Index-Cancer Scale [5] and CareGiver Oncology Quality of Life (CarGOQoL) [27, 28]. CarGOQoL questionnaire has been validated in a large cohort (837 caregivers, 50 of them were brain tumors patients’ caregivers, 187 dyades (patients and caregivers) in the validation cohort, 65 of them made all the evaluations).
Medical information and more communication with healthcare providers could improve caregivers’ QoL [20]. More education about the disease, the potential cognitive effects of treatment and support groups is required [29]. Educational programs for caregivers have always been a positive experience; and several teams reported their experience for reducing stress [30-32]. However, very few of them studied their impact on the QoL of caregivers [13]. A better QoL for caregivers could positively impact outcomes of patients with glioblastoma [13] and the physical health of brain tumor patients [4, 33]. A study has even shown that the more glioblastoma patients’ caregivers know about the disease, the less likely the patient is to die [34]. We conducted educational workshops for caregivers of patients with primary brain tumors. The objective is to explain precisely the medical aspects of brain tumors, describe resources available, and allow a moment of exchange between caregivers. We asked the caregivers to complete a QoL questionnaire after each workshop and retrospectively studied the impact of our educational workshops on caregivers’ QoL.
2. Material and Methods
2.1. Creation of Educational Workshops called AGAPE (‘Atelier Goûter pour les Aidants Proches de Patients ayant une tumeur Encéphalique’, snack workshops for caregivers of patients with brain tumors)
We developed educational workshops called AGAPE based on the caregivers’ feedback of patients with primary brain tumors who wanted a place for discussion without any psychologist present. Caregivers had been informed about the aims of AGAPE, as indicated on the flyer, to provide them a place for discussion and exchange with peers, in order to prevent exhaustion, whenever possible. Caregivers sign consent prior to attending the first workshop in particular for the use of data in a publication. To allow time for discussion, the first and the second workshops were held only if at least 3 participants from different family were present and the workshops were initially limited to six participants to ensure privacy. In 2015, oncologists initially only proposed AGAPE for recurrent glioblastoma patients’ caregivers according to the scoring described in Annex 1.
|
Assessment grid to identify caregivers who needed AGAPE workshops |
|
|
Frontal syndrome |
4 |
|
Disabling motor deficit (e.g.: hemiplegia, wheelchair) |
4 |
|
Delirium |
3 |
|
Behavioral disorder |
3 |
|
Frequent seizures |
3 |
|
Caregiver’s anxiety |
2 |
|
Young children |
2 |
|
Hospitalisation in medecine |
1 |
|
High grade glioma / uncertainty of the future |
1 |
|
Request for informations by caregivers |
1 |
|
Total: if ≥ 5: AGAPE Workshops were offered to caregivers |
Annex 1: Proposed AGAPE for recurrent glioblastoma patients’ caregivers.
Since the most frequent remark of the satisfaction questionnaire was to introduce AGAPE earlier, as of October 2016, the oncologist gave caregivers of patient with primary brain tumor the information about the workshops at the initial medical consultation not only after relapse but also during adjuvant treatment. For each patient, several different caregivers could take part in these educational workshops initially limited to 6 families. Some caregivers were so eager to take part in AGAPE, that up to 11 caregivers from 9 different families were allowed to attend the first workshop. But only the closest or most involved caregiver per family completed questionnaires.
2.2. Handbook for Brain Tumor Patients’ Caregivers
A handbook for brain tumor patients’ caregivers was written by members of our neuro-oncology unit; including 2 neuro-oncologists, 2 nurses specialized in neuro-oncology and educational workshops, a nurse responsible for the supportive care department, a radiation therapist, a social worker, 2 physiotherapists, a pharmacist, a radiotherapy manipulator and a dietician. The advantages and disadvantages of the diverse hospital facilities have also been validated by doctors in these institutions. This handbook was given only to AGAPE participants.
2.3. AGAPE Workshops
AGAPE took place in a quiet, soothing space in the supportive care department, outside of the treatment and consultation rooms, where snacks and drinks were provided. A medical oncologist and a nurse specialized in neuro-oncology or the nurse responsible for the supportive care department also took part in the AGAPE session. AGAPE was divided into 3 workshops of 2 hours, each one of them was between 3 to 4 weeks apart. All AGAPE sessions began by a round-table that permitted caregivers to introduce themselves and to express their expectations. During the first theoretical workshop, neurological symptoms as well as therapeutics were discussed. The aims were to better understand the brain tumor disease, its evolution, and to manage potential side effects of treatment. The second theoretical workshop was dedicated to information on instrumental human resources available (e.g., wheelchairs, walkers, crutches and psychometrics, nutrition, psychologists, social workers) and hospital facilities (e.g., rehabilitation and follow-up care, palliative care units, home hospitalization, mobile support and rehabilitation teams). The website of our Centre was also shown to caregivers, in particular the neuro-oncology unit homepage, (http//:www.centre-eugene-marquis.fr/). The third workshop was run as a support group open for free discussions. Every caregiver had the opportunity to share their difficulties and burdens with professionals and could obtain answers personalized to their specific needs. Caregivers of the previous session, whose loved one was still alive, were invited to participate in this third workshop.
2.4. Evaluation of Feasibility of AGAPE
AGAPE feasibility was evaluated by the caregivers’ attendance of the 2 theoretical scheduled sessions and their satisfaction according to a questionnaire filled out during the third workshop attended. Caregivers evaluated the general organization and the logistics (schedule, location, number of participants) of the workshops and could add comments, suggestions to improve them.
2.4. AGAPE Outcomes
Caregivers answered the final question: do you think these workshops should be maintained over time? Additional outcomes were the percentage of caregivers in favour of AGAPE sustainability.
2.5. Evaluation of the Impact of AGAPE on Caregivers’ QoL
In order to objectively evaluate the impact of AGAPE, caregivers were asked to complete a self-administered CarGOQoL questionnaire at the beginning of the first workshop: the baseline and after each workshop (only one per family). Through 29 items, CarGOQoL described 10 dimensions of caregivers’ QoL: psychological well-being, burden, relationship with healthcare professionals, administration and finances, coping, physical well-being, self-esteem, leisure time, social support, and private life. An index was calculated as the mean of all dimension scores. Each dimension and the index were ranged from 0 to 100, i.e., better QoL corresponding to higher score. We retrospectively analyzed CarGOQoL questionnaire scores for each caregiver during their involvement in the AGAPE workshops. As usual, the evaluation between QOL questionnaires is between 3 and 6 months. We choose a minimal time of at least 2 months, as the first three workshops could be scheduled during this time interval and during the longer interval between the first and last workshop to identify the change of QOL that occurs over the therapeutic management.
2.6. Statistical analysis
Patients’ and caregivers’ sociodemographic characteristics, time from diagnosis, workshops, progression, and death, carGOQOL score at baseline, and after every workshop were prospectively collected during the study. Statistics for continuous variables were presented by mean, standard deviation or median and range, whereas frequencies and percentages were used for categorical variables. Comparisons were made using nonparametric tests such as Mann-Whitney, Wilcoxon signed ranks. As is often the case with subjective scale measures, many missing data were expected. To account for most caregivers' responses without overestimating the QoL measures, different imputation for missing data was proposed based on the maximum bias rule. If there was a missing value on an item, the lowest score, the median and the mean of lowest and median score for that item was imputed [35, 36]. Unfortunately, questionnaires with more than half of the items missing were excluded completely.
3. Results
3.1. AGAPE workshops
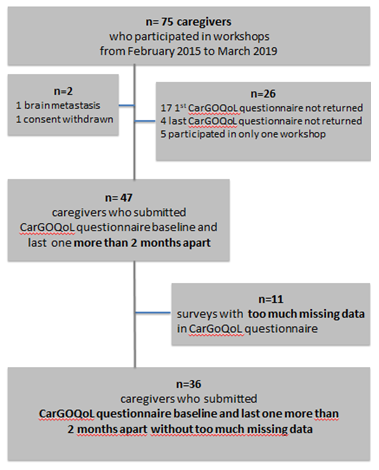
In total, between February 2015 and March 2019, 12 three-month sessions were organized allowing the attendance of 87 caregivers from 75 families (Figure 1). 2 caregivers were excluded: one after withdrawal of consent and a loved one treated for brain metastasis. 21 caregivers hadn’t submitted the first or the last CarGOQoL questionnaires, 11 with too much missing data and 5 other caregivers attended only one workshop (1 died, 4 loved one have a progressive disease after the first workshop of which 2 had been transferred to a palliative care unit before the second workshop). Only 36 caregivers submitted the baseline questionnaire and at least one other more than 2 months apart CarGoQol questionnaire (Figure 1). However, we tried to analyze the 2 groups (36 included and 37 excluded) to avoid bias as much as possible.
3.2. AGAPE Feasibility
84% of the caregivers attended the first two theoretical workshops. 1 caregiver didn’t take part in the second workshop because of scheduling issues (but she attended the 3rd workshop support group several times), one caregiver died before the second workshop, and 10 caregivers didn’t attend the 2nd workshop because of their loved one’s rapid progressive disease.
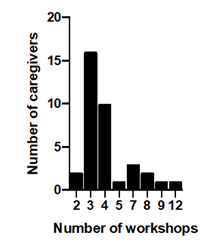
3.3. Caregivers and Patients Characteristics
89% of the caregivers were spouses (Table 1). In addition to the caregivers who completed the questionnaire, 3 sisters, 2 fathers, 3 mothers and 4 daughters took part in AGAPE. Two thirds of the patients were male, treated for glioblastoma (67%) after the first relapse (46%) (Table 2). As the caregivers who did not participate in 2 workshops (16%) were systematically excluded, the median number of workshops is statistically different between the 2 groups. The 36 caregivers included in the final analysis participated in between 2 and 12 workshops. (Figure 2). Two-thirds of the 36 loved ones had a progressive disease after the first workshop and 21 died. The interval between the first and the last workshop was up to 4 years.
|
Caregivers' Characteristics |
n= 73 |
n=36 included |
n=37 excluded |
p |
|
Relationships with the patients: |
||||
|
Wives |
42 |
13 |
11 |
|
|
Husbands |
23 |
10 |
13 |
|
|
Daughters |
3 |
2 |
1 |
|
|
Brother |
2 |
1 |
1 |
|
|
Mother |
1 |
0 |
1 |
|
|
Father |
1 |
0 |
1 |
|
|
Friend |
1 |
0 |
1 |
0.17 |
|
Time interval between first and last workhops |
||||
|
Median (months) |
1 |
4.5 |
1 |
|
|
[1st quartile-3rd quartile] |
[1-5] |
[1-10.3] |
[0-1] |
<0.0001 |
|
Number of workshop |
||||
|
Median |
2 |
3 |
2 |
|
|
[1st quartile-3rd quartile] |
[2-4] |
[3-4] |
[1-3] |
<0.0001 |
Table 1: Caregivers’ characteristics.
|
Patients' Characteristics |
n=73 |
n=36 included |
n=37 excluded |
p |
|
Age at diagnosis (years): Median |
55 |
54 |
55 |
|
|
[1st quartile-3rd quartile] |
[45-62] |
[44-62] |
[49-63] |
0.97 |
|
Patients' gender |
||||
|
Male |
48 |
23 |
25 |
|
|
Female |
25 |
13 |
12 |
0.75 |
|
Histology |
||||
|
Glioblastoma |
49 |
24 |
25 |
|
|
Without histological proof but treated as GBM |
3 |
2 |
1 |
|
|
Anaplatic astrocytoma |
4 |
3 |
1 |
|
|
Anaplastic oligodendroglioma |
10 |
6 |
4 |
|
|
Low grade glioma |
7 |
1 |
6 |
0.86 |
|
Time of the first workshop: (n) |
||||
|
During or after adjuvant treatment |
27 |
17 |
1 |
|
|
After 1st relapse |
34 |
14 |
20 |
|
|
After 2nd relapse |
7 |
5 |
2 |
|
|
After 3rd relapse |
5 |
0 |
5 |
0.08 |
|
Time interval between diagnosis and first workshop |
||||
|
Median (months) |
10 |
10 |
10 |
|
|
[1st quartile-3rd quartile] |
[7-24] |
[4.8-20.5] |
[7-34] |
0.46 |
|
Time interval between last workshop and palliative |
||||
|
management decision |
||||
|
Median (months) |
3 |
6 |
2 |
|
|
[1st quartile-3rd quartile] |
[1.5-5.5] |
[5.5-8.5] |
[0.8-4] |
0.04 |
Table 2: Patients’ characteristics.
3.4. Additional AGAPE Outcomes
Each caregiver was in favor of AGAPE sustainability. The level of AGAPE satisfaction on the general organization, logistics and workshops was very high (80%), the most frequent written remark was to propose AGAPE earlier, even during adjuvant treatment (not only after the first relapse). At the end of each workshop, an oral round table allowed each caregiver to express their feelings, satisfaction or discontent. For example, after the first workshop, caregivers reported being satisfied with knowing all possible symptoms, even though they admitted to be worried but they were also reassured to know how they should react and what they should do. The presentation has evolved to be more interactive: the caregivers had to identify all the potential brain tumor’s symptoms by themselves
3.5. Impact of AGAPE on QoL Evaluated by CarGOQoL
As indicated in Table 3, we compared dimension scores and index obtained after the first workshop to the last workshop that the 36 caregivers participated in. Overall, there was no difference in all these scores. Caregivers’s CarGOQoL index mean score was 70.0 at baseline before the first workshop and 69.9 for the last workshop they took part in (p=0.95). At baseline and after the last workshop, highest scores were obtained for administration and finances, social support dimensions, self-esteem, and relationship with healthcare professionals. Caregivers reported the lowest scores at the baseline and after the last workshop for leisure time, psychological well-being and private life. There was no statistical decrease in QoL between baseline and the last workshop. Even though these findings are not significant, caregivers seemed to have a better relationship with healthcare providers and better self-esteem after attending the AGAPE workshops. The 37 excluded caregivers’s CarGOQoL index mean score was 62,7, 64,0 and 62,6 with lowest, median and mean imputation respectively, which was significantly lower than the index of the 36 included caregivers (p<0.005). But the score was skewed with the integration of the lowest possible number to the missing data, which sometimes corresponded to half the questionnaire. This potential underestimation of quality of life may explain this significant difference. Moreover, when comparison is possible between the first and the last workshop in this group (if the questionnaires have been returned), there is no statistically significant difference whatever the imputation. Moreover, the median time between the last workshop attended by the caregivers and the palliative care decision for their loved one is shorter among the 37 excluded caregivers than the 36 included caregivers (p=0.04). The loved-ones of the 37 excluded caregivers were probably more symptomatic, so the burden was probably heavier on them.
|
CargoQoL dimension |
First workshop |
Last workshop |
IC 95% |
p |
|
Mean ± SD |
Mean ± SD |
|||
|
Psychological well-being |
57.64 ± 2.62 |
57.78 ± 2.96 |
-7.74 : 8.01 |
0.972 |
|
Burden |
76.67 ± 3.13 |
75.28 ± 3.14 |
-10.24 : 7.46 |
0.7552 |
|
Relationship with healthcare |
72.96 ± 2.35 |
77.96 ± 2.45 |
-1.76 : 11.76 |
0.1446 |
|
providers |
||||
|
Administration finances |
87.22 ±2.73 |
84.63 ±2.65 |
-10.18 : 5.0 |
0.4979 |
|
Coping |
63.33 ± 3.10 |
64.81 ± 2.70 |
-6.73 : 9.70 |
0.72 |
|
Physical well-being |
68.47 ± 2.69 |
69.03 ± 2.75 |
-7.10 : 8.21 |
0.8854 |
|
Self-esteem |
78 ± 1.91 |
79.43 ± 2.35 |
-4.62 : 7.48 |
0.6392 |
|
Leisure time |
56.11 ± 2.962 |
55.28 ± 3.0 |
-9.23 :7.57 |
0.8437 |
|
Social support |
80.56 ± 2.93 |
75.83 ± 2.97 |
-13.03 : 3.59 |
0.2608 |
|
Private life |
59.17 ± 3.89 |
58.33 ± 3.18 |
-10.85 : 9.18 |
0.8687 |
|
Index |
70.04 ± 1.65 |
69.89 ± 1.65 |
-4.80 : 4.50 |
0.9478 |
Table 3: Caregivers’ CargoQoL scores between the first and last AGAPE workshops.
4. Discussion
Information about brain tumors and treatment effects were the first expectations expressed by caregivers at the beginning of the first workshop, as found by Ownsworth and et al [37]. Small groups allowed each participant to share his/her own experience of caregiving including difficulties and abilities. AGAPE is a valuable source of information, the caregivers relating easily to a peer who is coping with a similar situation rather than a healthcare provider, as described in the literature [4, 10]. AGAPE was mostly offered to caregivers of patients with glioblastoma, due to rapid neurocognitive decline. AGAPE guide caregivers along several steps of the disease, from the announcement of the diagnosis to palliative care, according to the oral discussion in the 3rd workshop seems to help them accept the changes in the condition of their loved one and their death. Compared to a similar population of glioma [38], our population had higher scores at baseline in all dimensions and index. Another educational program with 24 caregivers had shown a statistical improvement on knowledge scores testing from baseline to the end of the workshops, but found a decline 4 to 6 weeks after the workshops [30]. Some studies have shown that neurological symptoms at progression [39] and recurrence also have a negative impact on brain tumor patients’ QoL [40]. A significant correlation between patients’ and caregivers’ overall QoL has been shown with similar reductions especially in their emotional and social well-being [10]. As two thirds of the patients presented neurocognitive decline, physical debilitation or behavioral changes due to disease progression since the baseline, maintain caregivers’ QoL between the first and the last workshop is essential. The absence of significant decline score highlighted one of the positive effects of AGAPE as a resource for caregiver to face the impact of the disease on their loved one.
Caregivers shared that they felt they had become invisible; neither friends nor doctors asked them about their well-being. As caregivers felt valued, AGAPE allowed an increase of self-esteem, coping, and relationship with healthcare providers between the first and the last workshop, but this was not significant. Moreover, confidence increased between caregivers and healthcare providers as a result of the workshops, as caregivers shared their private lives including their personal thoughts and feelings. Caregivers learned that it was fundamental to take care of themselves in order to take care of their loved one, they reported a stable sense of well-being between the first and the last workshop. Indeed, 2 caregivers from the first workshop (4 years ago), whose loved one was still alive, continue to attend the third workshop. The support group allowed caregivers to feel sometimes overburdened without guilt. The anxiety and worries about the future still predominated, as shown in others teams [21, 22], however caregivers felt that they could express themselves without judgment. The testimony of other caregivers, whose loved one had finished treatment without relapse or responded to bevacizumab after a relapse, maintained some hope of possible stabilization of the disease, even after a possible rapid neurological deterioration. Another team led to the same observation; caregivers appreciated sharing their own experiences with others caregivers [41]. Through AGAPE importance of social support as a crucial endpoint to allow caregivers to take time for themselves without feeling guilty. We insisted on the use of a list of resources to activate, if necessary. In the case of administrative or financial difficulties, caregivers from previous sessions emphasized how our social worker could easily help them in administrative procedures. Social help was appreciated to decrease the perceptual aspect of feeling overwhelmed. Reblin and al. [32] have found an association between greater burden at diagnosis and lower social support. Moreover, lower social support was related to higher depression and anxiety. This underlines the importance of early programs for caregivers in order to ensure low initial levels of burden. Sherwood and al. [9] concluded that researchers might not be able to reduce distress but could focus on preventing an increase of distress over time. Thanks to AGAPE, the caregivers felt that they were not alone in particular with administration difficulties and shared the burden with the support group. The decrease of burden, social isolation, administration and financial dimensions between baseline and last workshop attended was not significant in our study. Several limitations to our study should be discussed, including the small size of our cohort, due to the low incidence of primary brain tumors and our choice to limit the number of caregivers from different families during the first 2 workshops to 9. Moreover, this feasibility study had no control group. Caregivers, who didn’t attend AGAPE, were not interested in completing the QoL questionnaire. The participants may not represent all caregivers, but they correspond to those who wanted a support. Initially, we proposed AGAPE only for caregivers of patients with recurrent glioblastoma, but since caregivers asked us to introduce AGAPE earlier, we then authorized all caregivers whatever stage and histology of brain tumor. So it became heterogeneous with different impacts of prognosis on QoL. Only the closest caregiver completed the questionnaires to reduce the bias of multiple data on the same patient even though we ran risk of ignoring the impacts on other caregivers. Piil and et al. [41] have already shown that caregivers wanted interventions to maintain hope after diagnosis, early initiate health promotion activities, strategies for symptoms management and life planning. Only few studies in neuro-oncology [13, 30, 42, 43] have analyzed the impact of an intervention on the QoL of caregivers of patients with a primary brain tumor. Without any intervention, a significant decline had been found in all dimensions of QoL for patients with a recurrent high-grade glioma and their caregivers [13, 44]. An educational program for caregivers found an improvement of knowledge at 4 weeks but scores decreased at 6 weeks, suggesting that information needed to be repeated [30]. In our experience, some caregivers continued to join us for the third workshop, ensuring knowledge and sharing the burden throughout the disease’s trajectory from the initial announcement to palliative care. We found the same benefits (e.g., camaraderie, cohesion, motivation etc.) and barriers of support groups, such as logistical factor like transportation as Mallya and al. [45]. A meta-analysis on distress in neuro-oncology caregivers highlighted a feeling of isolation and lack of support from healthcare systems [46]. It is crucial to generalize early caregivers’ support to improve psychosocial outcomes [32]. Our educational workshops could easily be developed in other hospitals. Recent studies have demonstrated that caregivers’ mastery not only improves their own QoL [44], but increases the overall survival of patients with glioblastoma [34]. These two studies have found that mutual respect, good communication, caregiver mastery, and resilience benefit both patients and caregivers. Our real-life study shows, in spite of these limitations, that AGAPE workshops have helped maintain caregivers’ QoL even though the patients had a progressive disease, which is usually correlated to QoL decline [47].
5. Conclusion
Caregivers have to modify their everyday life to face new challenges imposed by brain tumors. Integrating them in health care through early educational workshops such as AGAPE is crucial. AGAPE combines 2 theoretical workshops to acknowledge and guide caregivers and a support group to share the burden of their new key role. Our study showed that educational workshops are feasible and indicated that they could help maintain caregiver’s QoL in patients with brain tumor. Further studies are necessary to implement them in daily practice.
Authors’ Contributions
All the authors contributed to the study conception and design. Material preparation, data collection, and analysis were completed by Heloïse Bourien and Elodie Vauléon. The first draft of the manuscript was written by Heloïse Bourien and Elodie Vauléon and all the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Funding
None
We thank Catherine Gaughan, a native English speaker, that has critically revised the manuscript.?
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The study was performed in accordance with the Declaration of Helsinki and was approved by a local Ethics committee of Rennes (IRB-ID: 28.08).
Consent to participate
All participants provided written informed consent prior to study participation.
Consent for publication
Authorization was included in the participation consent.
Availability of data and material
Data were collected to comply with the European law of the General Data Protection Regulation (GDPR).
Code availability
Not applicable
References
- Ullgren H, Tsitsi T, Papastavrou E, et al. How family caregivers of cancer patients manage symptoms at home: A systematic review. Int J Nurs Stud 85 (2018): 68-79.
- Taphoorn MJB, Klein M. Cognitive deficits in adult patients with brain tumours. Lancet Neurol 3 (2004): 159-168.
- Madsen K, Poulsen HS. Needs for everyday life support for brain tumour patients’ relatives: systematic literature review. Eur J Cancer Care (Engl) 20 (2011): 33-43.
- Sherwood P, Given B, Given C, et al. Caregivers of persons with a brain tumor: a conceptual model. Nurs Inq 11 (2004): 43-53.
- Weitzner MA, Jacobsen PB, Wagner H, et al. The Caregiver Quality of Life Index-Cancer (CQOLC) scale: development and validation of an instrument to measure quality of life of the family caregiver of patients with cancer. Life Res Int J Qual. Life Asp Treat Care Rehabil 8 (1999): 55-63.
- Schubart JR, Kinzie MB, Farace E. Caring for the brain tumor patient: family caregiver burden and unmet needs. Neuro-Oncol 10 (2008): 61-72.
- Piil K, Nordentoft S, Larsen A, et al. Bereaved caregivers of patients with Caring for the brain tumor patient: family caregiver burden and unmet needs. Neuro Oncol 10 (2008): 61-72. high-grade glioma: a systematic review. BMJ Support. Palliat. Care 9 (2019): 26-33.
- Pinquart M, Sorensen S. Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Aging 18 (2003): 250-267.
- Sherwood PR, Cwiklik M, Donovan HS. Neuro-oncology family caregiving: review and directions for future research. CNS Oncol 5 (2016): 41-48.
- Janda M, Steginga S, Langbecker D, et al. Quality of life among patients with a brain tumor and their carers. J Psychosom Res 63 (2007): 617-623.
- Muñoz C, Juarez G, Munoz ML, et al. The quality of life of patients with malignant gliomas and their caregivers. Work Health Care 47 (2008): 455-478.
- Ramirez C, Christophe V, Dassonneville C, et al. Caregivers’ quality of life and psychological health in response to functional, cognitive, neuropsychiatric and social deficits of patients with brain tumour: protocol for a cross-sectional study. BMJ Open 7 (2017): e016308.
- Boele FW, Hoeben W, Hilverda K, et al. Enhancing quality of life and mastery of informal caregivers of high-grade glioma patients: a randomized controlled trial. Neurooncol 111 (2013): 303-311.
- Parvataneni R, Polley MY, Freeman T, et al. Identifying the needs of brain tumor patients and their caregivers. Neurooncol 104 (2011): 737-744.
- Janda M, Eakin EG, Bailey L, et al. Supportive care needs of people with brain tumours and their carers. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 14 (2006): 1094-1103.
- McConigley R, Halkett G, Lobb E, et al. Caring for someone with high-grade glioma: a time of rapid change for caregivers. Med 24 (2010): 473-479.
- Arber A, Faithfull S, Plaskota M, et al. A study of patients with a primary malignant brain tumour and their carers: symptoms and access to services. J. Palliat. Nurs 16 (2010): 24-30.
- Strang S, Strang P. Spiritual thoughts, coping and “sense of coherence” in brain tumour patients and their spouses. Palliat Med 15 (2001): 127-134.
- Rosenblum ML, Kalkanis S, Goldberg W, et al. Odyssey of hope: a physician’s guide to communicating with brain tumor patients across the continuum of care. J Neurooncol 92 (2009): 241-251.
- Spetz A, Henriksson R, Bergenheim AT, et al. A specialist nurse-function in neurooncology: a qualitative study of possibilities, limitations, and pitfalls. Support. Care 3 (2005): 121-130.
- Salander P, Spetz, A. How do patients and spouses deal with the serious facts of malignant glioma? Med 16 (2002): 305-313.
- Applebaum AJ, Buda K, Kryza-Lacombe M, et al. Prognostic awareness and communication preferences among caregivers of patients with malignant glioma. Psychooncology 27 (2018): 817-823.
- Hazen RJ, Lazar A, Gennari JH. Assessing patient and caregiver needs and challenges in information and symptom management: a study of primary brain tumors. Annu Symp Proc 2016 (2017): 1804-1813.
- Pace A, Dirven L, Koekkoek JAF, et al. European Association for Neuro-Oncology (EANO) guidelines for palliative care in adults with glioma. Lancet Oncol 18 (2017): e330-e340.
- Hudson P, Remedios C, Zordan R, et al. Guidelines for the Psychosocial and Bereavement Support of Family Caregivers of Palliative Care Patients. J Palliat Med 15 (2012): 696-702.
- McMillan SC, Mahon M. Measuring quality of life in hospice patients using a newly developed Hospice Quality of Life Index. Qual Life Res Int J Qual Life Asp Treat. Care Rehabil 3 (1994): 437-447.
- Minaya P, Baumstarck K, Berbis J, et al. The CareGiver Oncology Quality of Life questionnaire (CarGOQoL): development and validation of an instrument to measure the quality of life of the caregivers of patients with cancer. Eur J Cancer Oxf Engl 48 (2012): 904-911.
- Kaveney SC, Baumstarck K, Minaya-Flores P, et al. Validation of the American version of the CareGiver Oncology Quality of Life (CarGOQoL) questionnaire. Health Qual. Life Outcomes 14 (2016): 82.
- Lageman SK, Brown PD, Anderson SK, et al. Exploring primary brain tumor patient and caregiver needs and preferences in brief educational and support opportunities. Care Cancer Off. J Multinatl Assoc Support Care Cancer 23 (2015): 851-859.
- Cashman R, Bernstein LJ, Bilodeau D, et al. Evaluation of an educational program for the caregivers of persons diagnosed with a malignant glioma. Oncol. Nurs. J Rev Can Nurs Oncol 17 (2007): 6-15.
- Swartz JJ, Keir ST. Program preferences to reduce stress in caregivers of patients with brain tumors. Clin J Oncol Nurs 11 (2007): 723-727.
- Reblin M, Ketcher D, Forsyth P, et al. Outcomes of an electronic social network intervention with neuro-oncology patient family caregivers. J Neurooncol 139 (2018): 643-649.
- Finocchiaro CY, Petruzzi A, Lamperti E, et al. The burden of brain tumor: a single-institution study on psychological patterns in caregivers. J Neurooncol 107 (2012): 175-181.
- Boele FW, Given CW, Given BA, et al. Family caregivers’ level of mastery predicts survival of patients with glioblastoma: A preliminary report. Cancer 123 (2017): 832-840.
- Sterne JAC, White IR, Carlin JB, et al. Multiple Imputation for Missing Data in Epidemiological and Clinical Research: Potential and Pitfalls. BMJ 338 (2009).
- Dziura JD, Post LA, Zhao Q, et al. Strategies for Dealing with Missing Data in Clinical Trials: From Design to Analysis. Yale J Biol Med 86 (2013): 343-358.
- Ownsworth T, Goadby E, Chambers SK. Support after brain tumor means different things: family caregivers’ experiences of support and relationship changes. Front Oncol 5 (2015): 33.
- Minaya Flores P, Berbis J, Chinot O. Assessing the quality of life among caregivers of patients with gliomas. Neuro-Oncol Pract 1 (2014): 191-197.
- Osoba NK, Aaronson M, Muller K. et al. Effect of neurological dysfunction on health-related quality of life in patients with high-grade glioma D. Newlands 34 (1994): 263- 278.
- Bosma I, Reijneveld JC, Douw L, et al. Health-related quality of life of long-term high-grade glioma survivors. Neuro-Oncol 11 (2009): 51-58.
- Piil K, Jakobsen J, Christensen KB, et al. Needs and preferences among patients with high-grade glioma and their caregivers - A longitudinal mixed methods study. Eur J Cancer Care (Engl) 27 (2018): e12806.
- Keir ST, Guill AB, Carter KE, et al. Differential levels of stress in caregivers of brain tumor patients--observations from a pilot study. Care Cancer Off. J Multinatl Assoc Support Care Cancer 14 (2006):1258-1261.
- Rabow MW, Goodman S, Chang S, et al. Filming the Family: A Documentary Film to Educate Clinicians about Family Caregivers of Patients with Brain Tumors. Cancer Educ 25 (2010): 242-246.
- Sacher M, Meixensberger J, Krupp W. Interaction of quality of life, mood and depression of patients and their informal caregivers after surgical treatment of high-grade glioma: a prospective study. J Neurooncol 140 (2018): 367-375.
- Mallya S, Daniels M, Kanter C, et al. A qualitative analysis of the benefits and barriers of support groups for patients with brain tumours and their caregivers. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 28 (2020): 2659-2667.
- Applebaum AJ, Kryza-Lacombe M, Buthorn J, et al. Existential distress among caregivers of patients with brain tumors: a review of the literature. Neuro-Oncol. Pract 3 (2016): 232-244.
- Osoba D, Brada M, Yung WK, et al. Health-related quality of life in patients treated with temozolomide versus procarbazine for recurrent glioblastoma multiforme. J Clin Oncol Off J Am Soc Clin Oncol 18 (2000): 1481-1491.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
