Atypical Presentation of a Large Aortopulmonary Window in a Very Low Weight and Preterm Born Infant
Article Information
Katja Schumacher, Sabine Meier, Michael A Borger, Martin Kostelka, Marcel Vollroth
Department of Cardiac Surgery, Heart Center, HELIOS Clinic, University Hospital Leipzig, Leipzig, Germany
*Corresponding Author: Marcel Vollroth, Department of Cardiac Surgery, Heart Center, HELIOS Clinic, University Hospital Leipzig, Leipzig, Germany.
Received: 21 March 2022; Accepted: 05 April 2022; Published: 13 May 2022
Citation: Katja Schumacher, Sabine Meier, Michael A Borger, Martin Kostelka, Marcel Vollroth. Atypical Presentation of a Large Aortopulmonary Window in a Very Low Weight and Preterm Born Infant. Archives of Clinical and Medical Case Reports 6 (2022): 370-373.
View / Download Pdf Share at FacebookKeywords
Aortopulmonary; Cardiac malformations; Surgery
Article Details
1. Introduction
With a prevalence of only 0.2-0.3% of all congenital cardiac malformations, aortopulmonary window is a rare but surgically correctable anomaly [1]. It is caused by the incomplete fusion of two conotruncal ridges that usually separate the embryonal truncus arteriosus into the aorta and pulmonary artery [1]. Frequently, aortopulmonary window is associated with other cardiac anomalies such as arch abnormalities, transposition of the great arteries, ventricular septal defects and tetralogy of Fallot [1-3]. Due to similar hemodynamic, differential diagnosis may include large ductus arteriosus and truncus arteriosus [1]. Because of the left-to-right-shunt, the defect leads to increased pulmonary blood flow following congestive heart failure, pulmonary hypertension and failure to thrive [1]. Depending on the size of the defect, the majority of patients suffer from severe clinical symptoms at young age, for example tachycardia, fatigue, tachypnea and increased respiratory symptoms with recurrent infections [2]. Surgery is indicated as soon as the diagnosis is made to prevent fixed pulmonary hypertension [1].
2. Case presentation
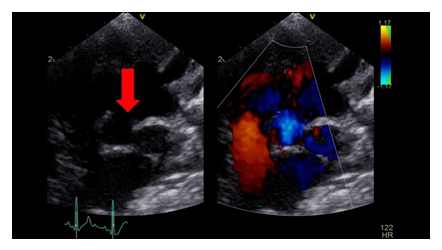
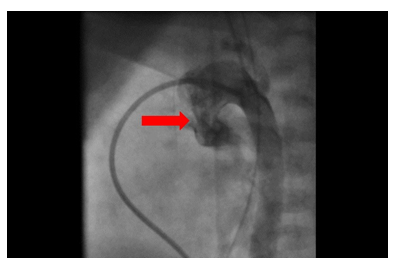
A one-month old premature born and low-weight (1348 g) female infant (born at gestational age 32+1) presented intubated and ventilated with progredient signs of heart failure and recurrent respiratory infections since birth. Clinical examination revealed a systolic murmur at the left sternal border. Echocardiography (Figure 1) and cardiac catherization (Figure 2) showed a large atypical aortopulmonary window >6mm located between the pulmonary artery bifurcation and the ascending aorta extending to the aortic arch.
The pressure in the right ventricle was nearly systemic, pulmonary artery pressure was very high (80/31-51). Additionally, echocardiography demonstrated an ostium secundum atrial septal defect with significant left to right shunt. Both ventricles were dilated, the right ventricle presented hypertrophic. Based on the clinical symptoms and the diagnostic findings, surgical correction was indicated. Surgery was performed 23 days before the expected delivery date. At the time of surgery, the weight of the infant was 2000g. Access was through median sternotomy; cardiopulmonary bypass was established with aorto-right- atrial cannulation. Surgery was performed in deep hypothermic circulatory arrest (18°C). Neuromonitoring was assessed with cerebral oximeter. The pulmonary arteries were snared, and aortic cross clamp was applied. Cardiac arrest was induced administering antegrade St. Thomas cardioplegia (30ml/kg/BW). The bypass was stopped for 25 minutes. After aortotomy, the location of the aortopulmonary window was identified and closed with autologous pericardial patch in sandwich-patch closure technique. The atrial septal defect was closed by direct suture. Cardiopulmonary bypass was re-started, and the patient was warmed up and weaned off bypass. The postoperative course was prolonged due to respiratory insuffiency with subsequent prolonged mechanical ventilation. There was no evidence of pulmonary hypertension. Chest X-ray demonstrated right upper lobe atelectasis. After bronchoscopy, the patient could be extubated four days after surgery. She was discharged from Intensive Care Unit after 19 days. Postoperative echocardiography revealed no residual defect and no shunting across the patch. The patient could leave the hospital 25 days postoperatively in a very good condition.
3. Comments
Since the aortopulmonary window is such a rare disease, there is no standardized surgery technique for its treatment so far. Over time, the surgical repair evolved from simple ligation, division and suturing to different patch closure techniques [3]. Surgery is mostly performed on cardiopulmonary bypass [3]. Aortopulmonary window may be classified by Mori et al [4]: Type I (proximal) located just above the sinus of Valsalva, type II (distal) located in the uppermost portion of the ascending aorta and type III (total) involving the majority of the ascending aorta. In our presented case, the defect extended to the proximal aortic arch on the opposite of the supraaortic vessels. This atypical localization justifies performing surgery in deep hypothermic circulatory arrest to provide neuroprotection. Furthermore, the surgical management was complex and challenging due to of the young age and low weight of the patient. Conventionally, surgery is tried to postpone until a higher weight is attained to decrease the risk of bypass-related complications such as coagulopathy, renal dysfunction and intracranial hemorrhage and finally an increased mortality [5]. In this case, delaying the surgical procedure was not possible because of the massive left-to-right-shunt following severe pulmonary hyperperfusion with increased pulmonary artery pressure.
4. Conclusions
We accomplished a very successful surgical repair of a very complex aortopulmonary window in a low-birth-weight premature born infant. Our report supports the approach to consider surgical repair as soon as the diagnosis is established, regardless of the patient's age and weight [1].
Competing Interests
None.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
References
- Gowda D, Gajjar T, Rao JN, et al. Surgical management of aortopulmonary window: 24 years of experience and lessons learned. Interact Cardiovasc Thorac Surg 25 (2017): 302-309.
- Demir IH, Erdem A, Saritas T, et al. Diagnosis, treatment and outcomes of patients with aortopulmonary window. Balkan Med J. Jun 30 (2013): 191-196.
- Backer CL, Mavroudis C. Surgical management of aortopulmonary window: a 40-year experience. Eur J Cardiothorac Surg. May 21 (2002): 773-779.
- Mori K, Ando M, Takao A, et wl. Distal type of aortopulmonary window. Report of 4 cases. Br Heart J 40 (1978): 681-689.
- Curzon CL, Milford-Beland S, Li JS, et al. Cardiac surgery in infants with low birth weight is associated with increased mortality: analysis of the Society of Thoracic Surgeons Congenital Heart Database. J Thorac Cardiovasc Surg 135 (2008): 546-551.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
