Transapical TAVR and Off-pump Coronary Artery Bypass: How to Tackle a Porcelain Aorta from Two Sides
Article Information
Matteo Scarpanti1, Alan Gallingani2, Andrea Agostinelli2, Francesco Formica1, Francesco Nicolini1
1Cardiac Surgery Unit, Department of Medicine and Surgery, University Hospital of Parma, Parma, Italy
2Cardiac Surgery Unit, Cardio-Thoracic and Vascular Surgery Department, University Hospital of Parma, Parma, Italy
*Corresponding Author: Alan Gallingani, Cardiac Surgery Unit, Cardio-Thoracic and Vascular Surgery Department, University Hospital of Parma, Parma, Italy.
Received: 18 March 2022; Accepted: 01 April 2022; Published: 20 May 2022
Citation: Matteo Scarpanti, Alan Gallingani, Andrea Agostinelli, Francesco Formica, Francesco Nicolini. Transapical TAVR and Off-pump Coronary Artery Bypass: How to Tackle a Porcelain Aorta from Two Sides. Archives of Clinical and Medical Case Reports 6 (2022): 437-441.
View / Download Pdf Share at FacebookAbstract
Here we report the case of a 77-year-old man who presented to our department with a history of aortic stenosis and newly discovered left main disease. He had a past medical history relevant for peripheral artery disease and the latest CT scan highlighted a severely calcified aorta circumferentially throughout its whole course (so called “porcelain aorta”). To find a definitive solution for the patient’s presenting problem, he underwent Off-Pump Coronary Artery Bypass (OPCAB) and, subsequently, Transapical Transcatheter Aortic Valve Replacement (TATAVR). We believe that, in selected patients presenting with aortic stenosis and coronary artery disease, for whom the risk for either percutaneous intervention or surgical aortic valve replacement are deemed too high, a hybrid approach with OPCAB and TA-TAVR is a very effective solution in tackling such a critical clinical scenario.
Keywords
Calcified ascending aorta; Off-pump coronary artery bypass; TAVR; Transapical TAVI
Calcified ascending aorta articles; Off-pump coronary artery bypass articles; TAVR articles; Transapical TAVI articles
Article Details
1. Case Report
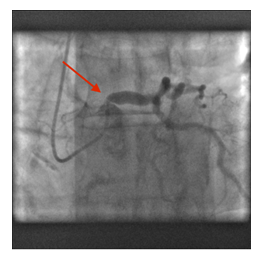
A 77-year-old man presented to our department with dyspnea, which had worsened over the past few months, and a longstanding history of aortic stenosis. His latest cardiac Ultrasound (US) showed a mean gradient of 48mmHg and an aortic valve area (AVA) of 0,9cm2. In light of the clinical status and ultrasound evidence, the patient was enlisted for aortic valve replacement after routine coronary angiography, which revealed severe stenosis of the proximal left main coronary artery (Figure 1, red arrow). The patient’s past medical history (PMH) was remarkable for severe peripheral vascular disease and had undergone multiple surgeries on the femoral-popliteal axis. Because of this, a preoperative CT angiography was deemed of paramount importance. The CT-scan showed a type-IA porcelain aorta [1], with extensive circumferential calcifications throughout its whole course (Figure 2). This latest finding posed a true surgical challenge, in a patient with indication for aortic valve replacement and myocardial revascularization. To tackle the two procedures required, the case was discussed among staff cardiac surgeons and a hybrid approach was devised: beating-heart Off-Pump Coronary Artery Bypass (OPCAB) and subsequent Transcatheter Aortic Valve Replacement via a Trans-Apical Access (TA-TAVR). The OPCAB was performed via a median sternotomy; the left Internal Mammary Artery (LIMA) was harvested as a skeletonized in-situ graft. Heparin was given at a dose of 1.5mg/kg without protamine administration at the end of the hybrid procedure. The LIMA was then anastomosed on the Left Anterior Descending (LAD) coronary artery utilizing the Octopus™ stabilizer (Medtronic plc, Minneapolis, MN). After completion of the revascularization, the sternum was closed and an antero-lateral mini-thoracotomy of approximately 5-7cm was performed at the level of the 5th intercostal space. The Left Ventricular (LV) apex was identified under Trans-Esophageal Echocardiography (TEE) via the “finger test”, two orthogonal 2-0 polypropylene U-shaped purse-string sutures reinforced by Teflon felts were placed and the TAVR introducer sheath was positioned. Under rapid ventricular pacing and utilizing a C-arm intensifier for visualization, a Sapien™ 23mm valve (Edwards Lifescience Corp., Irvine CA) was deployed with trivial paravalvular leak at post-operative TEE. Intraoperative course was uneventful, and the patient was brought to the cardiac intensive care unit (ICU), where he was extubated within 3 hours. He was taken to the in-patient ward on Post-Operative Day (POD) 1, with early mobilization, and was discharged on POD 7 to a rehabilitation facility, as by routine practice.
2. Discussion
The great prevalence of people living with coronary artery disease alongside degenerative calcific aortic stenosis warrants a systematic approach to these patients [2]. This is especially true in the presence of severe comorbidities that limit our therapeutic options. The presence of a true porcelain aorta constitutes a severe contraindication for any procedure that requires the placement of an aortic cannula, aortic cross clamping and performing an aortotomy, all necessary steps for surgical aortic valve replacement (SAVR). The presence of a porcelain aorta greatly favors TAVR as it is evident from the most recent guidelines both from the US [3] and from Europe [4]; since SAVR in these patients is associated with extremely high risks, not only of rupture but also for embolization of calcified plaques and delayed complications. This issue can be solved in the same operative setting by deploying the valve with a transaortic (if the anatomy of the patient allows it with a safe entrance point) [5] or transapical approach, given the impossibility to access from peripheral vessels. The latter, although of marginal implementation in current practice, can be of key importance in those patients with prohibitive access to any major artery [6]. At our institution we have extensive experience with the transapical approach, as it is a well-established route for many different structural cardiovascular procedures. Therefore, in the patient described in the case above as well as many others with such critical peripheral vascular anatomy, it is not only a safe route but also an advisable access point that should be part of the armamentarium of the modern cardiac surgeon. It is well established nowadays that the results for TAVR versus SAVR in the high-risk and elderly population are comparable [7]. In particular, in our case we strongly suggested TA-TAVR even if the patient was not affected by significant comorbidities, making him a high-risk surgical candidate, nor was his age a clear indication for a TAVR procedure. The only high, if not prohibitive, risk factor was a type IA porcelain aorta. The choice for coronary artery bypass grafting versus percutaneous intervention (PCI) in this setting was justified by the coronary anatomy of the patient, who presented with critical proximal left main disease [8], in the absence of coronary symptoms and in good hemodynamic conditions. Moreover, the technical and procedural risk associated with approaching a severely calcified coronary lesion in such critical location on the coronary tree via PCI led the decision-making process to favor an off pump surgical approach. In the modern era of personalized medicine, one should make the most of his/her expertise and know-how to find the best tailored approach for each patient’s clinical and surgical challenges. More specifically, in the field of increasingly complex cardiovascular disease in an ageing population, cardiac surgeons are bound to adapt and using the right tool for the right patient; this means a more widespread inclusion of less invasive techniques, such as OPCAB, endovascular and hybrid procedures in their everyday practice.
Conflict of interest
No conflict of interest to declare.
Funding
None
References
- Amorim PA, Penov K, Lehmkuhl L, et al. Not all porcelain is the same: classification of circular aortic calcifications (porcelain aorta) according to the impact on therapeutic approach. Thorac Cardiovasc Surg 61 (2013): 559-563.
- Mayr B, Firschke C, Erlebach M, et al. Transcatheter aortic valve implantation and off-pump coronary artery bypass surgery: an effective hybrid procedure in selected patients. Interact Cardiovasc Thorac Surg 27 (2018): 102-107.
- Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 143 (2021): e72-e227.
- Vahanian A, Beyersdorf F, Praz F, et al. ESC/EACTS Scientific Document Group; ESC Scientific Document Group. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J 28 (2021): 395.
- Baquero GA,Azarrafiy R, de Marchena EJ, et al. Hybrid off-pump coronary artery bypass grafting surgery and transaortic transcatheter aortic valve replacement: Literature review of a feasible bailout for patients with complex coronary anatomy and poor femoral access. J Card Surg 34 (2019): 591- 597.
- Agostinelli A, Gallingani A, Maestri F, et al. Left Ventricular Apex: A "Minimally Invasive Motorway" for Safe Cardiovascular Procedures. J Clin Med 10 (2021): 3857.
- Mack MJ, Leon MB, Smith CR, et al. PARTNER 1 trial investigators. 5-year outcomes of transcatheter aortic valve replacement or surgical aortic valve replacement for high surgical risk patients with aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet 385 (2015): 2477-2484.
- Holm NR, Mäkikallio T, Lindsay MM, et al. Percutaneous coronary angioplasty versus coronary artery bypass grafting in the treatment of unprotected left main stenosis: updated 5-year outcomes from the randomised, non-inferiority NOBLE trial. Lancet 395 (2020): 191-199.



 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
