Lower GI Bleeding and Left Colon Blue Rubber Blebs: Rare Case Report
Article Information
Fahad Al-Lhedan1*, Amr Mohammed Kurdi2
1Radiology and Nuclear Medicine Consultant, Medical Imaging Department, King Abdullah bin Abdulaziz University Hospital, Riyadh, Saudi Arabia
2Adult gastroenterologist and internist, IMCC Department, King Abdullah bin Abdulaziz University Hospital, Riyadh, Saudi Arabia
*Corresponding Author: Fahad Al-Lhedan, Radiology and Nuclear Medicine Consultant, Medical Imaging Department, King Abdullah bin Abdulaziz University Hospital, Riyadh, Saudi Arabia.
Received: 17 November 2022; Accepted: 29 November 2022; Published: 07 December 2022
Citation:
Fahad Al-Lhedan, Amr Mohammed Kurdi. Lower GI Bleeding and Left Colon Blue Rubber Blebs: Rare Case Report. Archives of Clinical and Medical Case Reports 6 (2022): 766-767.
View / Download Pdf Share at FacebookAbstract
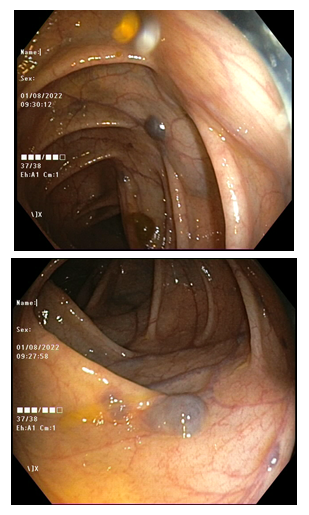
A middle-aged male who is known to have acne vulgaris on oral treatment complaining of hematochezia containing blood clots for few weeks. The patient underwent colonoscopy displaying several left colon blue rubber blebs and here we are presenting this rare case.
Keywords
Hematochezia; Melanocytic proliferation; Gastrointestinal tract
Article Details
1. Introduction
The blue nevus is a benign melanocytic proliferation that is typically a skin lesion [1]. The extra cutaneous blue nevi are rare especially in the gastrointestinal tract. The blue rubber bleb represents venous malformation that almost can involve any organ. However, the skin and gastrointestinal tract are the most frequently involved sites.
2. Case Report
This is a case of a 37-year-old male who was on 20 mg/OD isotretinoin capsule for acne vulgaris treatment. The patient presented few weeks after lower gastrointestinal tract bleeding that is containing blood clots following increasing isotretinoin dose to 40 mg/OD. The patient denied appetite change, weight loss, abdominal pain, dysphagia, rashes, fever and rigors. There was no family history of colon cancer or inflammatory bowel disease. The rectal exam revealed small internal hemorrhoids and there were no fissures. There were no skin lesions. The ophthalmic exam was normal. The iron was mildly reduced measuring 10.7 umol/L and apart from that no another abnormal laboratory result. A contrast enhanced abdomen and pelvis CT scan was obtained demonstrating no colonic masses or diverticular disease. Colonoscopy was performed showing several descending and sigmoid colon blue rubber blebs. Random biopsies were taken and the result is nonspecific colitis. Angiography via right common femoral artery approach was done and inferior mesenteric artery was catheterized delineating no obvious left colic artery or its branches vascular abnormality. Superior rectal artery terminal branches were superselectively embolized successfully but with no subsequent significant improvement. Hemorrhoids were removed using rubber band ligation and finally the PR bleeding is off.
3. Discussion
The blue nevus is a pigmented commonly encountered skin lesion. Involvement of mucosal surfaces, namely genitourinary tract, has been described but gastrointestinal tract mucosa blue nevus is an extremely rare finding. No consensus about the origin of blue nevus but the most commonly accepted theory is that it is originating form migrating neural crest cells. The blue nevus has two histological variants, which are the common and the cellular types [2,3]. The common blue nevus predominantly affects young females and it is commonly found in the extremities, hips and scalp while the cellular blue nevus usually affects older individuals and it is commonly found in the sacrum. The cellular blue nevus has the tendency to be larger than the common blue nevus and it can grow up to 2 cm in size. Histologically, a blue nevus has proliferating melanocytes in the dermis layer of skin. These melanocytes contain different amounts of melanin and this what gives them the characteristic blue color. They are usually benign lesions but the compound variant of blue nevus that involves dermo-epidermal junction has malignant potential [2]. The blue nevus appears as superficial hyperpigmented area [4,5]. Blue rubber bleb nevus syndrome is a rare disease manifested by multiple skin and visceral organs venous malformations and hemangiomas those can be present at any age. The most common presentation is lower gastrointestinal tract bleeding with resultant iron deficiency anemia. This syndrome lesion appears as cavernous venous dilations with a thin wall of smooth muscle cells lined by endothelial cells under a microscope [6,7]. The management plan of gastrointestinal tract lesions is controversial and is determined mainly by the disease extent and severity. Whereas most of the patients with mild-disease-form respond well to supportive therapy utilizing iron supplementation. However, surgical resection, endoscopic sclerosis and laser photocoagulation are all have been proposed for patients with severe bleeding [6].
4. Conclusion
Due to the rarity of its occurrence, the gastrointestinal tract blue rubber bleb clinical course is not clearly well known [7]. This entity is typically a skin lesion and it is apparently a benign abnormality but it has the potential for malignant transformation. Therefore, the possibility of extra cutaneous blue rubber bleb should be entertained. A multidisciplinary approach is mandatory to protocol proper therapeutic plan.
The patient was given consent to participate and to publish the data.
References
- Assarzadegan N, Salimian K, Hutchings D, et al. Clinicopathological study of blue nevi of the gastrointestinal (GI) tract: first case series. J Clin Pathol 74 (2021): 167-170.
- Makker J, Sakam S, Arety P, et al. Rectal blue nevus: Case report of a rare entity and literature review. Pathology - Research and Practice 211 (2015): 625-627.
- González-Cámpora R, Galera-Davidson H, Vázquez-Ramirez FJ, et al. Blue Nevus: Classical Types and New Related Entities: A Differential Diagnostic Review. Pathology - Research and Practice 190 (1994): 627-635.
- Jacob Schreiber Z, Pal TR, Hwang SJ. Blue nevus of the colorectal mucosa. Annals of Diagnostic Pathology 15 (2011): 128-130.
- Zaher S, Sedeeq Z. A rare case of blue nevus in the rectum. Human Pathology: Case Reports 18 (2019): 200341.
- Jin LX, Wang ZH, Xiao XB, et al. Blue rubber bleb nevus syndrome: A case report and literature review. World J Gastroenterol 20 (2014): 17254-17259.
- Mohan N, Tofani C, McCue P et al. Rectal Blue Nevus: Distinguishing Features of a Rare Entity. ACG case reports journal 3 (2016): e168.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
