A case of EBUS-TBNA in a Total Laryngectomy Patient using High Flow Nasal Oxygen
Article Information
Ralph Nehme*
Pulmonary and critical care – Interventional pulmonology, Fulltime faculty Lebanese American University School of Medicine (LAU-SOM), Zahar Street, Achrafieh , Beirut Lebanon
*Corresponding Author: Ralph Nehme, Pulmonary and critical care – Interventional pulmonology, Fulltime faculty Lebanese American University School Oof Medicine (LAU-SOM), Zahar Street, Achrafieh, Beirut Lebanon.
Received: 13 January 2023; Accepted: 23 January 2023; Published: 06 February 2023
Citation: Ralph Nehme. A case of EBUS-TBNA in a Total Laryngectomy Patient using High Flow Nasal Oxygen. Archives of Clinical and Medical Case Reports 7 (2023): 73-76.
View / Download Pdf Share at FacebookAbstract
Endobronchial Ultrasound transbronchial needle aspiration (EBUSTBNA) is currently considered as the gold standard technique for the assessment of mediastinal, hilar and centrally located lymph nodes and tumours. However, the ideal approach to sedation and oxygen supplementation during the procedure has not been clearly defined especially in particular clinical scenarios like total laryngectomy patients. In the following article we present the case of an EBUS-TBNA in a total laryngectomy patient done under moderate sedation and oxygenation using a heated High Flow Nasal Oxygen canula. The purpose of this case report is to shed light on the feasibility of the procedure under moderate sedation and the utility of the HFNO in special patients as those having a total laryngectomy.
Keywords
Endobronchial Ultrasound; EBUS-TBNA; High Flow Nasal Oxygen; HFNO; Laryngectomy; Sedation
Article Details
1. Case Presentation
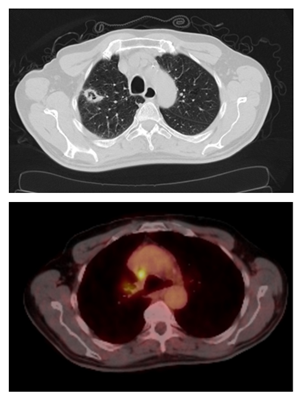
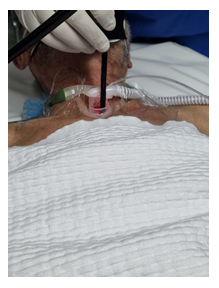
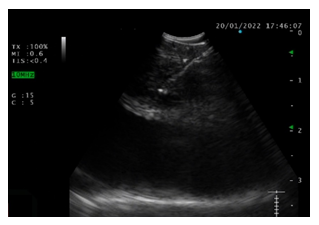
A 70-year-old male patient with a 70 Pack-year smoking history was diagnosed with a low to intermediate grade adenosquamous carcinoma of the larynx in 2017 for which he was treated by radiotherapy followed by total laryngectomy. A follow-up PET CT scan done in December 2021 showed a right upper lobe 2.5cm cavitating lung nodule with an SUVmax = 4.5 associated with a right lower para-tracheal (IV-R) lymph node station that is 1cm in size and has an SUVmax = 5.5 (Figure 1a and 1b). He was referred to our institution for Endobronchial Ultrasound Transbronchial Needle Aspiration (EBUS-TBNA) of the IV-R station. The challenge in this case was to find the best way to safely ventilate the patient while performing the procedure. Should it be done under general anesthesia or moderate sedation? And what would be the ideal method of ventilation/oxygenation? Having a total laryngectomy meant that access through the mouth was impossible. At the same time, inserting an endotracheal (ET) tube through the tracheotomy for a deep sedation approach would have made the procedure difficult because the ET tube’s position inside the trachea covers the IV-R station. The decision was taken to provide oxygenation through a heated High Flow Nasal Oxygen (HFNO) canula (Figure 2) while providing moderate sedation with a continuous propofol drip. HFNO settings were 60 L/min and SpO2 80%. The procedure was successfully performed (Figure 3) and station IV-R was sampled 5 times for cytology (Figure 4). The patient maintained good vital signs and a SpO2 >93% throughout the procedure. He was discharge at home the same day without any complications.
2. Discussion and Conclusions
EBUS-TBNA has become the gold standard tool for the assessment of mediastinal, hilar and centrally located lung tumors and lymph nodes for many reasons [1]. First, several meta-analyses on the performance of EBUS-TBNA have shown a pooled sensitivity of 88-93% and a pooled specificity of 100% [2–4]. Second, studies comparing EBUS-TBNA to mediastinoscopy in the staging of non-small cell lung cancer (NSCLC) showed similar performance in terms of sensitivity, specificity, positive and negative likelihood ratios [5]. Some studies were even able to demonstrate a superiority for EBUS-TBNA over mediastinoscopy in terms of sensitivity, diagnostic accuracy and negative predictive value [6]. This difference could be attributed to the fact that some lymph node stations like the hilar, subcarinal if in a low position and the left lower paratracheal in case it is located deep beneath the aortic arch, are more frequently and easily accessible via EBUS-TBNA than mediastinoscopy. The optimal type of sedation for EBUS-TBNA has not been established yet and studies on the subject have been sometimes contradictory. Yarmus et al. demonstrated that more lymph nodes per patient were sampled (2.2 vs 1.4; P<0.01) and the diagnostic yield was higher (80% vs 66%; P<0.01) when EBUS-TBNA was performed under deep sedation as opposed to moderate sedation [7]. On the other hand, Casal et al. found that EBUS-TBNA done under moderate sedation, resulted in a comparable diagnostic yield [8]. Patient safety and satisfaction are also two important variables to take into consideration when choosing the type of sedation. Patient satisfaction was assessed in a study by Jeyabalan et al., the most frequently reported symptom was cough, being described as mild by 71% of the patients and 87% of the patients stated that they are willing to undergo a repeat EBUS-TBNA [9]. However, it is important to mention the lack of control group as a limitation of this study. Finally, the rate of severe complications seems to be the same when performing EBUS-TBNA under either moderate or deep sedation [10,11]. Factors that seem to influence the choice of sedation are: Number and size of stations to be sampled, number of passes per station, in case other procedures are to be done in addition to the EBUS-TBNA like airway stenting or debulking, availability of an operating room to the endoscopist, cost of the procedure and finally operator experience and prior training. It is also important to mention and to take into consideration the fact that most of the studies showing similar results between the two sedation modalities have been done in expert hands and that these results might not be replicable in less experienced centers. In our particular case, having a laryngectomy made it difficult to go for a deep sedation approach because of the difficulty to properly ventilate the patient. For that reason, moderate sedation with oxygenation via a HFNO canula was done. Oxygen delivery during EBUS-TBNA via HFNO has been reported in a few studies. The rationale behind the use of HFNO are potential oxygenation improvement and better patient tolerance. In fact, Takakuwa et al. have demonstrated that the use of HFNO during EBUS-TBNA resulted in a statistically better mean lowest SpO2 of 93% vs 88% in the conventional nasal cannula group [12]. In another study, there was statistically more patient discomfort in the nasal canula group when compared to the HFNO group [13]. This approach was successfully employed in our patient. He maintained a SpO2 > 93% throughout the procedure and didn’t report any discomfort during or when asked after the procedure. To our knowledge, this is the first case of a total laryngectomy patient undergoing EBUS-TBNA to be reported in the literature. Through this case report we aim to shed awareness on the feasibility of EBUS-TBNA under moderate sedation using a HFNO canula in these patients.
Conflict of Interest and Declarations
- There was no conflict of interest while writing this case report.
- Ethics approval and consent to participate: N/A
- Consent to publish: The patient’s written consent to publish was obtained. Patient confidentiality was respected when writing the article. All photos have been appropriately de-identified.
- Availability of data and materials: All data and materials related to the case report can be accessed by the editors by contacting the corresponding author.
- The authors declare that they have no financial or non-financial competing interests.
- The was no funding and no sponsors while writing this case report.
- Authors’ Contributions: RN is the patient’s attending physician. He is the main author of the article.
- Acknowledgements: N/A
References
- de leyn P, Dooms C, Kuzdzal J, et al. Revised ests guidelines for preoperative mediastinal lymph node staging for non-small-cell lung cancer. European Journal of Cardio-thoracic Surgery 45 (2014): 787-798.
- Chandra S, Nehra M, Agarwal D, et al. Diagnostic accuracy of endobronchial ultrasound-guided transbronchial needle biopsy in mediastinal lymphadenopathy: a systematic review and meta-analysis. Respiratory care [Internet] 57 (2012): 384-391.
- Adams K, Shah PL, Edmonds L, et al. Test performance of endobronchial ultrasound and transbronchial needle aspiration biopsy for mediastinal staging in patients with lung cancer: systematic review and meta-analysis. Thorax [Internet] 64 (2009): 757-762.
- Gu P, Zhao YZ, Jiang LY, et al. Endobronchial ultrasound-guided transbronchial needle aspiration for staging of lung cancer: a systematic review and meta-analysis. European journal of cancer (Oxford, England?: 1990) [Internet] 45 (2009):1389-1396.
- Rossi Figueiredo V, Francisco Guerreiro Cardoso P, Jacomelli M, et al. EBUS-TBNA versus surgical mediastinoscopy for mediastinal lymph node staging in potentially operable non-small cell lung cancer: a systematic review and meta-analysis. J Bras Pneumol 46 (2020): e20190221.
- Um SW, Kim HK, Jung SH, et al. Endobronchial ultrasound versus mediastinoscopy for mediastinal nodal staging of non-small-cell lung cancer. Journal of thoracic oncology?: official publication of the International Association for the Study of Lung Cancer [Internet] 10 (2015): 331-337.
- Yarmus LB, Akulian JA, Gilbert C, et al. Comparison of moderate versus deep sedation for endobronchial ultrasound transbronchial needle aspiration. Annals of the American Thoracic Society [Internet] 10 (2013):121-126.
- Casal RF, Lazarus DR, Kuhl K, et al. Randomized trial of endobronchial ultrasound-guided transbronchial needle aspiration under general anesthesia versus moderate sedation. American journal of respiratory and critical care medicine [Internet] 191 (2015): 796-803.
- Jeyabalan A, Medford ARL. Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration: Patient Satisfaction under Light Conscious Sedation. Respiration [Internet] 88 (2014): 244-250.
- Conte SC, Spagnol G, Confalonieri M, et al. Deep sedation versus minimal sedation during endobronchial ultrasound transbronchial needle aspiration. Monaldi archives for chest disease = Archivio Monaldi per le malattie del torace [Internet] 88 (2018): 22-26.
- Fernandes MGO, Santos VF, Martins N, et al. Endobronchial Ultrasound under Moderate Sedation versus General Anesthesia. Journal of clinical medicine [Internet] 7 (2018).
- Takakuwa O, Oguri T, Asano T, et al. Prevention of hypoxemia during endobronchial ultrasound-guided transbronchial needle aspiration: Usefulness of high-flow nasal cannula. Respiratory investigation [Internet] 56 (2018): 418-423.
- Ucar EY, Araz Ö, Kerget B, et al. Comparison of high-flow and conventional nasal cannula oxygen in patients undergoing endobronchial ultrasonography. Intern Med J 51 (2021): 1935-1939.



 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
