Arthroscopic Removal of Shoulder Joint Embedded Gunshot Bullet: A Case Report
Article Information
Joseph E Nassar1, Yehia Tfayli2, Mohamad Issa1, Akram Al Ramlawi1, Ahmad Naja1*
1Orthopaedic Surgery Department, American University of Beirut Medical Center, Beirut, Lebanon
2Jefferson Health Northeast 3B Orthopaedics, Philadelphia PA, USA
*Corresponding Author: Ahmad Naja, Orthopaedic Surgery Department, American University of Beirut Medical Center, Beirut, Lebanon.
Received: 14 February 2023; Accepted: 28 February 2023; Published: 16 March 2023
Citation:
Joseph E Nassar, Yehia Tfayli, Mohamad Issa, Akram Al Ramlawi, Ahmad Naja. Arthroscopic Removal of Shoulder Joint Embedded Gunshot Bullet: A Case Report. Archives of Clinical and Medical Case Reports. 7 (2023): 129-132.
View / Download Pdf Share at FacebookAbstract
Joint related gunshot injuries encompass significant morbidity if left untreated. Open and arthroscopic procedures are the main stay treatment for removal of foreign body. Nevertheless, there is no definitive management due to the scarcity of cases in the literature. We report the case of a white Arab 38-years-old man with a high velocity gunshot wound leading to bullet dislodgement in the left glenohumeral joint. The patient’s wound was treated with arthroscopy, extensive debridement, and decompression of subacromial space with partial acromioplasty.
Keywords
Arthroplasty; Case Report; Gunshot; Glenohumeral Joint; Rochester-Pean Forceps
Arthroplasty articles; Case Report articles; Gunshot articles; Glenohumeral Joint articles; Rochester-Pean Forceps articles
Article Details
Abbreviations:
GSW- Gunshot wound; GS- Gunshot
1. Introduction
Around 30,000 patients are being hospitalized in the US due to gunshot wounds (GSW) and 2500 die due its wound complications [1]. Shoulder gunshot (GS) injuries are around 9% of gunshot injuries [2]. No clear consensus is present in current literature regarding the definitive management of joint affected gunshot injuries. Few case reports tackled GS injuries by arthroscopic debridement, antibiotic therapy, and tetanus prophylaxis. Joint affected GS injuries encompass several complications mainly because of possible retained intra-articular foreign bodies that might affect joint mechanics resulting in early onset arthritis [3, 4]. With that being said, arthroscopic washout and removal of foreign bodies are important to prevent GS injuries related complications. We report a case of high velocity gunshot wound leading to bullet dislodgement in the left glenohumeral joint associated with minimally displaced proximal humeral head fracture. The patient’s wound was treated with arthroscopy, extensive debridement, and decompression of subacromial space with partial acromioplasty. Consent regarding the submission and publication of this case report has been provided by the concerned patient.
2. Case Report
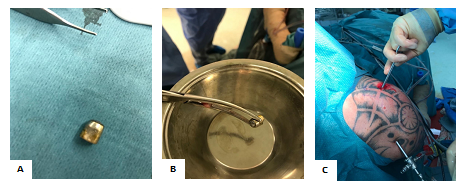
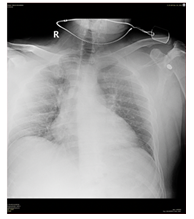
A 39-year-old Lebanese male presented conscious to the emergency room on the 19th of December 2021, with a single gunshot wound at his lateral upper chest, close to the axilla and with no exit wound, leaving a 1.6 cm metallic bullet ‘Figure 1A’. The incident was due to a high velocity gunshot fired at approximately 30 cm. On the physical exam, the patient’s range of motion was limited due to pain and with an open wound of 2.5 cm. Also, the patient was neurovascular intact. He had limited active shoulder flexion, abduction and no external or internal rotation. Any passive movement was eliciting pain. The CT angio-chest revealed an intra-minimally displaced fracture of the left humeral head, with the largest bone fragment measuring 2.8 cm in the infraglenoid region with a small associated joint effusion. The bullet was lodged deep in the upper joint with no fracture of the glenoid ‘Figure 2’. There was no pneumothorax or hemothorax with no evidence of vessel injury ‘Figures 3A, 3B, 3C, 3D’.
Figures 1A: Intra-operative photograph of the removed 1.6 cm metallic bullet. 1B: Intra-operative photograph showing the bullet retrieval using Rochester-Pean forceps. 1C: Intra-operative photograph showing the removal of the bullet through the posterior and anterosuperior portal with the patient in beach-chair position.
The patient was taken down to the OR for shoulder debridement synovectomy and for removal of the foreign body. The bullet was embedded deep in the upper part of the shoulder joint between the glenoid and the humeral head without any evidence of fracture. The bullet was retrieved using Rochester-Pean forceps ‘Figure 1B’ through the posterior and anterosuperior portal. We had to increase the size of the portal to reach the bullet fragment while keeping the shoulder under traction. Postoperative care was uneventful ‘Figure 1C’. On postoperative day 1, the patient’s range of motion improved mainly upon active flexion up to 70 degrees (20 degrees preoperation). Abduction also improved to 60 degrees (almost zero degrees preoperation). A follow-up with the patient 10 days after the incident showed improved pain with recovered forward elevation but limited external rotation. His wounds were clean after the debridement. The patient underwent 15 sessions of physiotherapy. At postoperative day 64, the patient had 90% recovery of the range of motion ‘Figure 4’. 2 years follow-up with the patient showed almost complete recovery of active and passive shoulder range of motions with adequate strength and negative examination of impingement syndrome.
3. Discussion
Arthroscopy for the management of gunshot wounds involving the shoulder decreases the potential operative morbidity compared to traditional surgical exposures [5, 6]. Moreover, it is important to highlight the significance of the surgical tools that aid in the removal of the foreign body in view of the limited inaccessibility of the entire joint in arthroscopy compared to open procedure. The Rochester-Pean forceps were used in our case due to its adequate size in entering the portal while being wide enough to catch the bullet fragment. The locking system of the former secured rigid fixation to the bullet due its protruding teeth and allowed a forceful traction to dislodge the bullet. Galland et al, reported a case of bullet extraction in the supraspinatus compartment by arthroscopy that was removed using a grasper [7]. Mahirogullari et al, again, demonstrated the role of shoulder arthroscopy for bullet removal. The typical posterior portal was used for shoulder arthroscopy same as in our case, in addition to the anterolateral portal. Postoperative care involved active and passive strengthening exercises and range of motion [8]. In some cases, patients present with impingement pain and functional limitation due to the uncomfortable settling position of the bullet in the subacromial space. In a case report, by Otero et al., the bullet caused pain and impingement by tearing the rotator cuff and embedding itself in the inferior surface of the acromion. The rotator cuff was arthroscopically reconstructed after the bullet was extracted. The patient reported total pain alleviation and increased range of motion [9]. Tarkin et al, and Guevara et al, reported cases of a retained bullet in the glenohumeral joint that was removed using the same procedure and without any complications [10, 11]. With the aid of instruments, like the laparoscopic graspers, shoulder arthroscopy can be used to successfully remove larger entrapped bullets or foreign bodies. This case report fortifies the available literature and emphasizes the importance of shoulder arthroscopy in removing lodge bullet injuries without the need for an open procedure. The used tools are important because they will facilitate the extraction method through the arthroscopy portals.
4. Conclusion
To conclude, joint placed bullet injuries associated with non-surgical proximal humerus fracture can be managed by arthroscopic debridement with or without a subacromial decompression. The type of graspers used is important in view of the limited exposure and the small size of the portals to access the entire joint. However, shoulder arthroscopy would allow retrieval of the foreign bodies without the morbidity associated with open procedures. More case reports with different presentations are needed to fortify the efficacy of shoulder arthroscopy compared to open procedure.
Declarations
Acknowledgements
Not applicable.
Author Contributions
J.N.—writing the manuscript. A.N.—editing. A.R., M.I., Y.T.—literature review. A.N. — corresponding author. All authors read and approved the final manuscript.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Availability of Data and Materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
Written informed consent was obtained from the patient’s legal guardian for participation in the study. The study was approved by the ethical committee at the American University of Beirut Medical Center.
Consent for Publication
Written informed consent was obtained from the patient’s legal guardian or next of kin for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Cook A, Osler T, Hosmer D, et al. Gunshot wounds resulting in hospitalization in the United States: 2004-2013. Injury 48 (2017): 621-627.
- Ordog GJ, Wasserberger J, Balasubramanium S, et al. Civilian gunshot wounds--outpatient management. J Trauma 36 (1994): 106-111.
- Haspl M, Bojanic I, Pecina M. Arthroscopic retrieval of metal foreign bodies from the knee joint after war wounds. Injury 27 (1996): 177-179.
- Hartford JM, Gorczyca JT. Late arthroscopic debridement of metal fragments and synovectomy after penetrating knee joint injury by low-velocity missile: a report of two cases. J Orthop Trauma 15 (2001): 222-224.
- de Araújo GC, Mourão NT, Pinheiro IN, et al. Lead Toxicity Risks in Gunshot Victims. PLoS One 10 (2015): e0140220.
- Cantrell C, Gerlach E, Butler B, et al. The role of arthroscopy in bullet removal: A systematic review of the literature. J Orthop 22 (2020): 442-448.
- Galland A, Lunebourg A, Airaudi S, et al. A bullet in the supraspinatus compartment successfully removed by arthroscopy: case report and review of the literature. Case Rep Orthop 2015 (2015): 806735.
- Mahirogullari M, Cilli F, Akmaz I, et al. Acute arthroscopic removal of a bullet from the shoulder. Arthroscopy 23 (2007): 676.e1-3.
- Otero F, Cuartas E. Arthroscopic removal of bullet fragments from the subacromial space of the shoulder. Arthroscopy 20 (2004): 754-756.
- Tarkin IS, Hatzidakis A, Hoxie SC, et al. Arthroscopic treatment of gunshot wounds to the shoulder. Arthroscopy 19 (2003): 85-89.
- Guevara J, Chinnakkannu K, Raju S. Acute Arthroscopic Removal of a Bullet Embedded in the Glenoid: A Case Report. J Orthop Case Rep 11 (2021): 59-62.




 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
