Urethral-Sparing Robot-Assisted Simple Prostatectomy: Case Series of the Initial Experience of a Brazilian Surgical Center
Article Information
João Pádua Manzano1,3, João Henrique Sendrete de Pinho2*, Thainã de Oliveira Azambuja3, Davi Souza Constantin3, Vinicius Meneguette Gomes de Souza3, Ricardo Luis Vita Nunes3, Jaime Comar Filho3, Frederico Teixeira Barbosa3
1Department of Surgery, Federal University of Sao Paulo, Sao Paulo, Brazil
2Faculty of Medicine, Federal University of Juiz de Fora, Minas Gerais, Brazil
3Moriah Hospital - Sao Paulo, Brazil
*Corresponding Author: João Henrique Sendrete de Pinho, Faculty of Medicine, Federal University of Juiz de Fora, Minas Gerais, Brazil.
Received: 20 April 2023; Accepted: 03 May 2023; Published: 12 May 2023
Citation: João Pádua Manzano, João Henrique Sendrete de Pinho, Thainã de Oliveira Azambuja, Davi Souza Constantin, Vinicius Meneguette Gomes de Souza, Ricardo Luis Vita Nunes, Jaime Comar Filho, Frederico Teixeira Barbosa. Urethral-Sparing Robot-Assisted Simple Prostatectomy: Case Series of the Initial Experience of a Brazilian Surgical Center. Archives of Clinical and Medical Case Reports 7 (2023): 200-208.
View / Download Pdf Share at FacebookAbstract
Benign prostatic hyperplasia (BPH) is a common condition among older men that causes lower urinary tract symptoms. Although pharmacological treatments are available, surgery is often required. The development of surgical techniques has progressed, with robotic simple prostatectomy (RASP) being one of the minimally invasive techniques for larger prostates. However, ejaculatory dysfunction remains a common postoperative problem of BPH surgery, significantly impacting patients' quality of life. In 1990, Dixon et al. were the first to describe the urethral-sparing approach, which maintained anterograde ejaculation. Recently, Wang et al. performed the first urethral-sparing RASP (USRASP). We present a case series from the initial experience of US-RASP in a high-volume Brazilian surgical center with an experienced robotic surgeon. Three patients underwent US-RASP at our center in 2022 were included. The mean age and prostate volume were, respectively, 67.7 years (42-89) and 88.9ml (85.6-92). None of the patients had a median lobe. Total preservation of the urethra was achieved in all patients, with no US-RASP failures and conversion to standard RASP. The average operative time of US-RASP was 98min (86-118). There were no intraoperative complications. Two of the three patients maintained anterograde ejaculation (66.7%), but with reduced volume. There were no postoperative complications and the patients are still being followed up to assess the long-term results. Therefore, our results suggest that USRASP can be implemented with good rates of preservation of the urethra and anterograde ejaculation, since performed by an experienced robotic surgeon.
Keywords
Benign prostatic hyperplasia; Madigan prostatectomy; Urethral-sparing robot-assisted simple prostatectomy; Ejaculation preserving; Case series
Benign prostatic hyperplasia articles; Madigan prostatectomy articles; Urethral-sparing robot-assisted simple prostatectomy articles; Ejaculation preserving articles; Case series articles
Article Details
1. Introduction
Benign Prostatic Hyperplasia (BPH) is a prevalent diagnosis among older men, contributing to Lower Urinary Tract Symptoms (LUTS) such as urgency, frequency, nocturia, weak urinary stream, and incomplete bladder emptying [1]. Epidemiological studies showed that 50% of men in their fifties will have BPH symptoms [2], and the incidence of LUTS in this age group is estimated as high as 25% in some studies [2,3]. Despite the different pharmacological drugs available to treat BPH or LUTS, the surgical approach is often required [4,5]. Surgical reports for BPH disease date back to the early 1900s, when Freyer proposed digital enucleation of the adenoma through a transvesical approach [6], and later Millin described a transcapsular technique [7]. Since then, technological advancements have led to the development of several surgical techniques over the past few decades, including robotic surgery for accessing larger size prostates [8-11]. According to European Association of Urology (EAU) guidelines, for patients affected by significant bladder outlet obstruction or LUTS not responsive to medical therapy secondary to BPH, endoscopic techniques represent the first choice [5]. Currently, simple prostatectomy and HoLEP are the preferred techniques for prostates larger than 80ml [5]. Open Simple Prostatectomy (OSP) is the gold standard approach for simple prostatectomy [6,7,12], but in recent years, minimally invasive techniques have gained popularity, with interesting results [13]. Robotic-Assisted Simple Prostatectomy (RASP) has become the new standard minimally invasive technique for large prostates, with studies showing improvements in peri-operative outcomes without compromising functional outcomes. Despite recent technical innovations, several postoperative problems are still unresolved. Among them, retrograde ejaculation is one of the most frequent problems, with a major impact on patients’ quality of life [14,15]. To address this issue, a technique called urethral-sparing simple prostatectomy has gained popularity. This approach preserves the urethra and aims to maintain anterograde ejaculation [16-18]. The concept of preservation of the prostatic urethra (Madigan technique) was initially described by Dixon et al. in OSP but has not been widely used due to technical complexity [14]. However, the era of robot-assisted surgery that allows for better visualization, dissection, and suturing, a wider use of urethral-sparing techniques has been proposed with significant advantages in terms of less residual adenoma, shorter catheterization time, and better preservation of ejaculate function [8,16-18]. We present a case series of urethral-sparing RASP (US-RASP) performed in patients with BPH, in a Brazilian high-volume surgical center with an experienced robotic surgeon.
2. Materials and Methods
2.1 Study design
This is a retrospective, observational, case-series study of patients with massive BPH (prostate volume > 80 ml) and with indication for surgical treatment, submitted to US-RASP in a Brazilian center with high surgical volume. All surgeries were performed by an experienced robotic surgeon who has performed over 500 RARP and 32 RASP (JPM). The main objective of this study was to evaluate the US-RASP reproducibility in our center, analyzing the level of preservation of the urethra and the postoperative results, mainly the preservation of the anterograde ejaculation.
2.2 Surgical technique
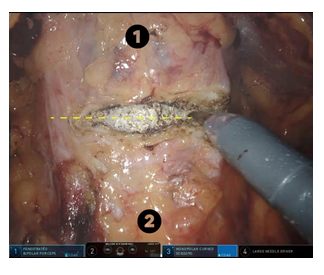
All adenomectomies were performed using a Da Vinci Xi Surgical System (Intuitive Surgical, Sunnyvale, CA, USA) following the step by step described by Porpiglia et al [18]. Under general anesthesia, the patient is prepared and positioned in a slight Trendelenburg position (27°). Pneumoperitoneum is achieved using a Veress needle inserted in the periumbilical area. After the establishment of pneumoperitoneum through puncture with a Veress needle in the periumbilical region. The five ports (four 8mm trocars for the Da Vinci Xi system and one 5mm for the assistant surgeon) are placed in a classic fan configuration and the robot is docked. After incising the parietal peritoneum for retropubic access and removing the periprostatic fat, an anterior transverse incision is made halfway between the dorsal venous complex and the bladder neck (Figure 1).
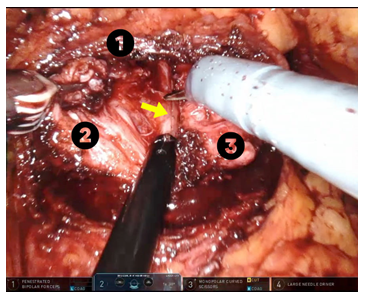
The cleavage plane between the capsule and the adenoma is identified anteriorly and gently dissected into the apex of the prostate bilaterally (Figure 2).
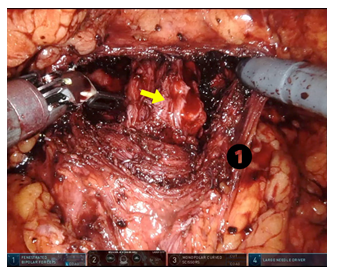
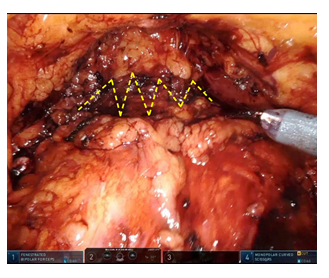
Basically, enucleation of the adenoma is performed in the avascular plane of the capsule, starting in the left lobe. Dissection is performed from the apex of the prostate bilaterally to the left lateral aspect of the adenoma, then cranially into the bladder neck, using bipolar forceps to control possible bleeding from perforating blood vessels. At the end of this stage of dissection, the left lobe is mobilized, except for its medial portion, which is still attached to the urethra. Subsequently, a median longitudinal incision is made in the anterior commissure and the urethra is medialized with the aspirator by the assistant and gently dissected from the left lobe of the adenoma. Finally, the posterior aspect of the surgical capsule is reached with a caudocranial dissection, with the left lobe removed. The same steps are performed for right lobe resection. After removing the adenoma (Figure 3), the hydrodistension test is performed, filling the bladder with 150ml of saline solution, to verify the integrity of the urethra and the degree of preservation. Any perforation is sutured with 4-0 absorbable monofilament and any bleeding is controlled.
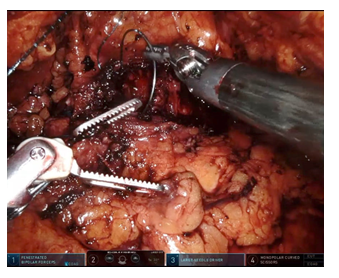
To aid in hemostasis, a thrombin gelatin hemostatic matrix is placed in the prostatic pocket, and the prostatic capsule is finally closed with a continuous two-layer 3-0 barbed suture (Figure 4 and 5).
3. Results
Three patients underwent US-RASP at our center in 2022 and were included in this study. The mean age was 67.7 years (42-89). The mean prostate volume among the three patients was 88.9ml (85.6-92), and none of the patients had a median lobe. Regarding preoperative clinical symptoms, two patients had moderate obstructive LUTS, mainly weak stream, short voiding interval, frequent nocturia and use of dutasteride. The third patient, who was only 42 years old, had severe obstructive symptoms that progressed to acute urinary retention. Two patients were hypertensive, one of them a longtime smoker and with a family history of bladder and colon cancer in first-degree relatives. Regarding previous surgeries, although one patient had a history of orthopedic surgeries and another of angioplasty with stent, none of the patients had undergone abdominal or pelvic surgeries. One of the patients had a large and bilateral inguino-scrotal hernia, and it was decided to repair it in the same procedure. Total preservation of the urethra was achieved in all patients, with no US-RASP failures and conversion to standard RASP. The average operative time of US-RASP was 98min (86-118), disregarding the time used for the repair of the inguino-scrotal hernia in one of the cases. There were no intraoperative complications. Regarding the postoperative functional outcomes reported by the patients, all patients are satisfied with the outcome of the surgery, with a strong stream, voiding interval greater than 2 hours, reduced nocturia and normal erections. Two of the three patients maintained anterograde ejaculation (66.7%), but with reduced volume. There were no postoperative complications and the patients are still being followed up to assess the long-term results.
4. Discussion
BPH surgery aims to relieve urethral obstruction and several endoscopic techniques have been introduced to decrease intraoperative complications and reduce morbidity [8,19]. One of the major complications of BPH surgery is ejaculatory dysfunction, which can significantly affect quality of life, particularly in young and sexually active men [14,15]. Although various techniques have been proposed to decrease postoperative ejaculatory dysfunction rates, mainly retrograde ejaculation [14,16-18]. The exact mechanism involved in the pathogenesis of postoperative ejaculatory dysfunction is still unclear, but contrary to what was thought, the bladder neck closure is not necessary for antegrade ejaculation, as demonstrated during transurethral incision of the prostate [20,21]. An ultrasonographic study on the mechanics of ejaculation in 30 men showed the importance of muscle tissue during ejaculation, with verumontanum playing a crucial role in propelling sperm distally [22]. This "high-pressure ejaculatory area" can still function even with the bladder neck open, as long as the tissues around the verumontanum are not damaged [18]. Recently, with the advent of robotic surgery, the Madigan technique for preserving the urethra has been heavily studied as an alternative for preserving ejaculatory function in patients undergoing RASP [16-18]. In 2018, Wang et al. introduced the first urethra-sparing RASP technique [16]. The procedure involves extraperitoneal access, exposure of the bladder neck junction, and careful dissection between the adenoma and prostatic urethra under the anterior commissure [16]. The prostatic lobe is removed to facilitate the dissection and removal of the contralateral lobe, while avoiding urethral damage [8,16]. The urethral integrity is tested by filling the bladder with saline and inspecting for perforations, with immediate repair performed if needed. Continuous bladder irrigation is not required [8,16]. Posteriorly, Simone et al. described a transperitoneal approach using near-infrared fluorescence imaging to ensure prostatic urethral integrity during the adenoma dissection [17]. An injection of indocyanine green into the bladder helps with visualization during the procedure [17]. Comparing the results of our small series of initial cases with the literature, the rate of total preservation of the urethra is higher than that found in the studies by Simone et al. and Porpiglia et al. (60.86% and 83.4%, respectively), possibly due to the low number of patients in our case series [17,18]. Preservation of anterograde ejaculation was achieved in 66.7% (2/3) of patients, this value is consistent with that found by Porpiglia et al. (63% to 81%, ranging from 1 to 12 months of follow-up) [18]. Regarding surgical time, if we compare it with the findings of Porpiglia et al., the author who described the step-by-step procedure we used in our center, there was a difference of 12 minutes less in our series of cases [18]. This may have happened due to several factors, such as the low number of patients in the case series, the difference in complexity between the cases and the way in which surgical time was measured.
All patients in our study had prostates larger than 80ml, with a mean prostate volume of 88.9ml, a value lower than that found in the studies by Simone et al. and Porpiglia et al. (102 and 140, respectively) [17,18]. Another important difference is that, contrary to previous studies, none of the patients in our case series had a median lobe. Both the absence of the median lobe and the smaller size of the prostate reveal fewer complex cases in our case series, which is compatible with the better urethral preservation rate and the shorter surgical time found. This study has some limitations: (a) the retrospective and observational design; (b) the low number of patients included; and (c) the short postoperative follow-up, which made it impossible to carry out a statistical analysis. Although it is a small case series, our study represents the initial result of US-RASP implantation in a South American center, showing good rates of total preservation of the urethra and preservation of anterograde ejaculation, without complications.
5. Conclusion
Therefore, our results suggest that US-RASP can be implemented with good rates of preservation of the urethra and anterograde ejaculation, since performed by an experienced robotic surgeon and in well-selected cases.
Acknowledgements
The authors would like to thank Hospital Moriah, São Paulo, Brazil, for the support and high-tech infrastructure offered to patients.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of Interest
The authors declare no conflicts of interest.
Consent
Written informed consent was obtained from patients for publication of this case series. A copy of the written consent is available for review by the Editor-in-Chief of this journal upon request.
References
- Irwin DE, Kopp ZS, Agatep B, et al. Worldwide prevalence estimates of lower urinary tract symptoms, overactive bladder, urinary incontinence and bladder outlet obstruction. BJU Int 108 (2011): 1132-1138.
- Vuichoud C, Loughlin KR. Benign prostatic hyperplasia: epidemiology, economics and evaluation. Can J Urol 1 (2015): 1-6.
- Rosen R, Altwein J, Boyle P, et al. Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7). Eur Urol 44 (2003): 637-649.
- Van Asseldonk B, Barkin J, Elterman DS. Medical therapy for benign prostatic hyperplasia: a review. Can J Urol 1 (2015): 7-17.
- Gratzke C, Bachmann A, Descazeaud A, et al. EAU Guidelines on the Assessment of Non-neurogenic Male Lower Urinary Tract Symptoms including Benign Prostatic Obstruction. Eur Urol 67 (2015): 1099-1109.
- Freyer PJ. A New Method of Performing Perineal Prostatectomy. Br Med J 1 (1900): 698-699.
- Millin T. The surgery of prostatic obstructions. Ir J Med Sci 257 (1947): 185-189.
- Moschovas MC, Timóteo F, Lins L, et al. Robotic surgery techniques to approach benign prostatic hyperplasia disease: A comprehensive literature review and the state of art. Asian J Urol 8 (2021): 81-88.
- Kordan Y, Canda AE, Köseoglu E, et al. Robotic-Assisted Simple Prostatectomy: A Systematic Review. J Clin Med 9 (2020): 1798.
- John H, Wagner C, Padevit C, et al. From open simple to robotic-assisted simple prostatectomy (RASP) for large benign prostate hyperplasia: the time has come. World J Urol 39 (2021): 2329-2336.
- Ng BHS, Chung E. A state-of-art review on the preservation of sexual function among various minimally invasive surgical treatments for benign prostatic hyperplasia: Impact on erectile and ejaculatory domains. Investig Clin Urol 62 (2021): 148-158.
- DE Nunzio C, Lombardo R, Nacchia A, et al. Young Academic Urologists’ benign prostatic obstruction nomogram predicts clinical outcome in patients treated with transurethral resection of prostate: an Italian cohort study. Minerva Urol Nefrol 70 (2018): 211-217.
- Autorino R, Zargar H, Mariano MB, et al. Perioperative Outcomes of Robotic and Laparoscopic Simple Prostatectomy: A European-American Multi-institutional Analysis. Eur Urol 68 (2015): 86-94.
- Dixon AR, Lord PH, Madigan MR. The Madigan prostatectomy. J Urol 144 (1990): 1401-1403.
- Rowland D, McMahon CG, Abdo C, et al. Disorders of orgasm and ejaculation in men. J Sex Med 7 (2010): 1668-1686.
- Wang P, Xia D, Ye S, et al. Robotic-assisted Urethra-sparing Simple Prostatectomy Via an Extraperitoneal Approach. Urology 119 (2018): 85-90.
- Simone G, Misuraca L, Anceschi U, et al. Urethra and Ejaculation Preserving Robot-assisted Simple Prostatectomy: Near-infrared Fluorescence Imaging-guided Madigan Technique. Eur Urol 75 (2019): 492-497.
- Porpiglia F, Checcucci E, Amparore D, et al. Urethral-sparing Robot-assisted Simple Prostatectomy: An Innovative Technique to Preserve Ejaculatory Function Overcoming the Limitation of the Standard Millin Approach. Eur Urol 80 (2021): 222-233.
- Pandolfo SD, Del Giudice F, Chung BI, et al. Robotic assisted simple prostatectomy versus other treatment modalities for large benign prostatic hyperplasia: a systematic review and meta-analysis of over 6500 cases. Prostate Cancer Prostatic Dis (2022).
- Hedlund H, Ek A. Ejaculation and sexual function after endoscopic bladder neck incision. Br J Urol 57 (1985): 164-167.
- Yang SSD, Tsai YC, Chen JJ, et al. Modified transurethral incision of the bladder neck treating primary bladder neck obstruction in young men: a method to improve voiding function and to preserve antegrade ejaculation. Urol Int 80 (2008): 26-30.
- Gil-Vernet JM, Alvarez-Vijande R, Gil-Vernet A, et al. Ejaculation in men: a dynamic endorectal ultrasonographical study. Br J Urol 73 (1994): 442-448.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
