Splenic Infarct Following Roux-en-Y Gastric Bypass Surgery: A Case Report
Article Information
Khurram Arshad MD1*, Rabia Latif MBBS2*, Yazan Alamro MBBS1, Farman Ali MD1, Antoine Egbe MD1, Ahmed subahi MBBS1, Ali Akram Khan MBBS2
1Internal Medicine department Corewell Health East Dearborn
2Internal Medicine Department Mclaren Flint Hospital
3Cardiology Department Mclaren Flint Hospital
*Corresponding author: Khurram Arshad MD, Internal Medicine department Corewell Health East Dearborn.
Received: 14 February 2024; Accepted: 26 February 2024; Published: 06 April 2024
Citation: Khurram Arshad MD, Rabia Latif MBBS, Yazan Alamro MBBS, Farman Ali MD, Antoine Egbe MD, Ahmed subahi MBBS, Ali Akram Khan MBBS. Splenic Infarct Following Roux-en-Y Gastric Bypass Surgery: A Case Report. Archives of Internal Medicine Research. 7 (2024): 71-72.
View / Download Pdf Share at FacebookAbstract
We are presenting a case of a 31-year-old female with morbid obesity who underwent Roux-en-Y gastric bypass (RYGB) six weeks ago. The patient complained of acute abdominal pain, nausea, and weight loss. After a diagnostic evaluation, it was discovered that the patient had small bowel obstruction with post-surgical changes and a concurrent splenic infarct. This case highlights the importance of recognizing and managing potential complications, such as vascular injury and infarction, following RYGB.
Keywords
Splenic Infarct; Roux-en-Y gastric bypass (RYGB)
Article Details
Introduction:
Roux-en-Y gastric bypass (RYGB) is a standard surgical procedure used to treat morbid obesity. Although RYGB is generally considered safe, it's essential to remain vigilant in identifying and addressing rare complications such as splenic infarction. Splenic infarction is a primarily silent condition, and because many cases go undiagnosed, the exact incidence of the condition is obscure and likely underestimated. Similarly, the incidence and severity of this rare condition in the postoperative period for bariatric surgeries are still unknown.
Case Presentation:
A 31-year-old female with morbid obesity underwent RYGB six weeks prior to presentation with acute abdominal pain, nausea, and a 15 lb weight loss since surgery. The pain, located in the middle of the abdomen and radiating to the back and the shoulder, had progressively worsened overnight. The patient denied alleviation of pain with bowel movements and reported no vomiting. Vitals were stable.
Clinical Findings:
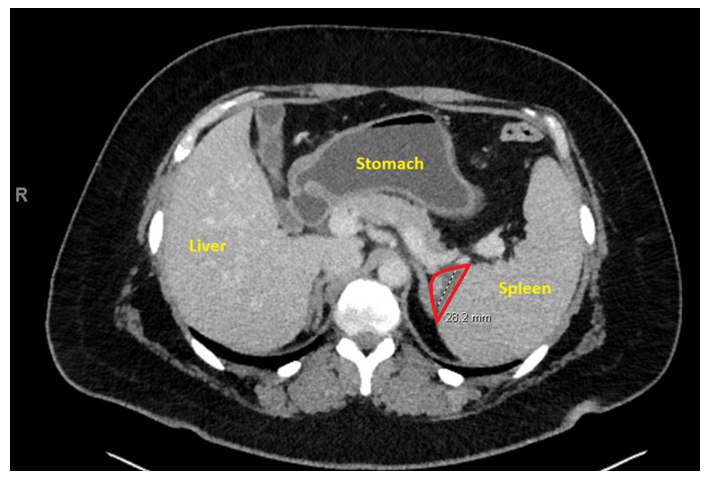
Patient labs revealed chronic microcytic anemia; other parameters, including WBC, PLT, amylase, lipase, and electrolytes, were unremarkable. A CT abdomen/pelvis showed small bowel dilatation involving proximal small bowel loops with post-surgical changes, indicative of small bowel obstruction. Additionally, a small wedge-shaped hypodensity within the spleen was suggestive of a small splenic infarct (Figure 1).
Discussion:
Splenic infarction is a severe and uncommon complication that is often associated with hematological disorders, trauma, and vascular interventions [1]. It is characterized by ischemia and necrosis of the splenic parenchyma. Postoperative splenic infarction has been reported, particularly in cases related to laparoscopic procedures and the use of energy vessel sealing devices. Excessive use of tissue sealing systems may increase the risk of splenic injury [2,3]. Preventing frequent mobilization of connective tissue around vascular structures is key to avoiding this complication. Although there is a lack of available data regarding the frequency and seriousness of splenic infarction in individuals undergoing Roux-en-Y esophagojejunostomy, diagnosis is often incidental to CT scans [4].
Most cases are asymptomatic, but complications requiring surgical intervention, such as hemorrhage, rupture, or abscess, can occur. Splenic infarction, by itself, does not necessarily require surgery. If postoperative splenic infarction is diagnosed, a nonoperative approach requires careful monitoring, with surgery recommended for persistent symptoms or the presence of complications. Patients undergoing bariatric surgery should be aware of the possibility of splenic infarction when sudden abdominal pain arises, mainly if it radiates from the left upper quadrant to the left shoulder. Uncomplicated cases of splenic infarction typically resolve without intervention within 7-14 days [5,6,7].
Treatment for patients with sickle cell hemoglobinopathies may be necessary to address hypoxia and acidosis, while those with septic emboli may require intravenous antibiotics and additional cardiac evaluation. Consultation with hematology, oncology, or rheumatology specialists may be necessary for patients with underlying hematologic or autoimmune conditions. However, for traumatic splenic injury, abnormal vascular structures, or hemodynamic instability, surgical assessment may be necessary.
Conclusion:
This case highlights the need for increased awareness of potential vascular complications, such as splenic infarction, in patients undergoing RYGB. Timely recognition and intervention are crucial for optimal patient outcomes. Surgeons should exercise caution, particularly in the use of tissue sealing systems, to prevent unnecessary mobilization of connective tissue around vascular structures. Further research is required to determine the incidence and severity of visceral infarction in patients undergoing bariatric surgeries.
Acknowledgments:
We express gratitude to the patient for granting consent to publish this case report and appreciate the collaborative efforts of the healthcare team involved.
Funding sources:
Self-Funded
Conflict of Interest:
The authors declare no conflicts of interest.
References
- Antopolsky, N. Hiller, S. Salameh, et al., Splenic infarction: 10 years of experience, Am. J. Emerg. Med. 27 (2009): 262–265.
- Ring, E. Stein, J. Stern, Splenic infarct – an unusual complication of gastrectomy for cardia carcinoma, Internet J. Surg. 21 (2009): 1.
- W. Wilkinson, K. Edwards, E.D. Adams, Splenic infarction following laparoscopic nissen fundoplication: management strategies, JSLS 7 (2003): 359–365.
- Tung, F.C. Chen, C.J. Lo, Splenic abscess: an easily overlooked disease, Am. Surg. 72 (4) (2006) 322–325.
- Mamoun C, Houda F. [Splenic infarction revealing infectious endocarditis in a pregnant woman: about a case and brief literature review]. Pan Afr Med J 30 (2018): 184.
- Pereda MA, Isaac J, Zhang Y, et al. Massive Splenic Infarction in a Child With Sickle Cell Disease on Chronic Transfusion Therapy. J Pediatr Hematol Oncol 41 (2019): e79-e82.
- Blackwood B, Binder W. Unusual Complications From Babesia Infection: Splenic Infarction and Splenic Rupture in Two Separate Patients. J Emerg Med 55 (2018): e113-e117.


 Impact Factor: * 3.6
Impact Factor: * 3.6 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 