Oral Manifestation of a Systemic Bleeding Diathesis with Fatal Outcome: A Holistic Approach to Assessment
Article Information
Raphael Figueroa, Mahnaz Fatahzadeh*
Department of Diagnostic Sciences, Rutgers School of Dental Medicine, Newark, NJ-USA
*Corresponding Author: Mahnaz Fatahzadeh, Department of Diagnostic Sciences, Rutgers School of Dental Medicine, 110 Bergen Street Newark, NJ-USA
Received: 19 September 2019; Accepted: 01 October 2019; Published: 04 October 2019
Citation: Raphael Figueroa, Mahnaz Fatahzadeh. Oral Manifestation of a Systemic Bleeding Diathesis with Fatal Outcome: A Holistic Approach to Assessment. Dental Research and Oral Health 2 (2019): 047-052.
View / Download Pdf Share at FacebookAbstract
Oral cavity is the mirror of body health and disease and the relationship between oral and systemic health is multi-faceted and reciprocal. In fact, many systemic conditions could manifest in the oral region, sometimes prior to their diagnosis. Dentists are physicians of the oral cavity and a holistic approach to patient assessment can guide dental providers in differentiating between oral abnormalities of local and systemic origin and deciding on appropriate management.
Keywords
History; Physical exam; Holistic; Oral-systemic connection; Bleeding
History articles, Physical exam articles, Holistic articles, Oral-systemic connection articles, Bleeding articles
History articles History Research articles History review articles History PubMed articles History PubMed Central articles History 2023 articles History 2024 articles History Scopus articles History impact factor journals History Scopus journals History PubMed journals History medical journals History free journals History best journals History top journals History free medical journals History famous journals History Google Scholar indexed journals Physical exam articles Physical exam Research articles Physical exam review articles Physical exam PubMed articles Physical exam PubMed Central articles Physical exam 2023 articles Physical exam 2024 articles Physical exam Scopus articles Physical exam impact factor journals Physical exam Scopus journals Physical exam PubMed journals Physical exam medical journals Physical exam free journals Physical exam best journals Physical exam top journals Physical exam free medical journals Physical exam famous journals Physical exam Google Scholar indexed journals Holistic articles Holistic Research articles Holistic review articles Holistic PubMed articles Holistic PubMed Central articles Holistic 2023 articles Holistic 2024 articles Holistic Scopus articles Holistic impact factor journals Holistic Scopus journals Holistic PubMed journals Holistic medical journals Holistic free journals Holistic best journals Holistic top journals Holistic free medical journals Holistic famous journals Holistic Google Scholar indexed journals Oral-systemic connection articles Oral-systemic connection Research articles Oral-systemic connection review articles Oral-systemic connection PubMed articles Oral-systemic connection PubMed Central articles Oral-systemic connection 2023 articles Oral-systemic connection 2024 articles Oral-systemic connection Scopus articles Oral-systemic connection impact factor journals Oral-systemic connection Scopus journals Oral-systemic connection PubMed journals Oral-systemic connection medical journals Oral-systemic connection free journals Oral-systemic connection best journals Oral-systemic connection top journals Oral-systemic connection free medical journals Oral-systemic connection famous journals Oral-systemic connection Google Scholar indexed journals Bleeding articles Bleeding Research articles Bleeding review articles Bleeding PubMed articles Bleeding PubMed Central articles Bleeding 2023 articles Bleeding 2024 articles Bleeding Scopus articles Bleeding impact factor journals Bleeding Scopus journals Bleeding PubMed journals Bleeding medical journals Bleeding free journals Bleeding best journals Bleeding top journals Bleeding free medical journals Bleeding famous journals Bleeding Google Scholar indexed journals oral cavity articles oral cavity Research articles oral cavity review articles oral cavity PubMed articles oral cavity PubMed Central articles oral cavity 2023 articles oral cavity 2024 articles oral cavity Scopus articles oral cavity impact factor journals oral cavity Scopus journals oral cavity PubMed journals oral cavity medical journals oral cavity free journals oral cavity best journals oral cavity top journals oral cavity free medical journals oral cavity famous journals oral cavity Google Scholar indexed journals thrombocytopenia articles thrombocytopenia Research articles thrombocytopenia review articles thrombocytopenia PubMed articles thrombocytopenia PubMed Central articles thrombocytopenia 2023 articles thrombocytopenia 2024 articles thrombocytopenia Scopus articles thrombocytopenia impact factor journals thrombocytopenia Scopus journals thrombocytopenia PubMed journals thrombocytopenia medical journals thrombocytopenia free journals thrombocytopenia best journals thrombocytopenia top journals thrombocytopenia free medical journals thrombocytopenia famous journals thrombocytopenia Google Scholar indexed journals Dentists articles Dentists Research articles Dentists review articles Dentists PubMed articles Dentists PubMed Central articles Dentists 2023 articles Dentists 2024 articles Dentists Scopus articles Dentists impact factor journals Dentists Scopus journals Dentists PubMed journals Dentists medical journals Dentists free journals Dentists best journals Dentists top journals Dentists free medical journals Dentists famous journals Dentists Google Scholar indexed journals
Article Details
1. Introduction
Sir William Osler, the father of modern medicine, revolutionized medical education by incorporating bedside teaching and his emphasis on diagnostic skills [1]. This clinical approach is reflected in his well-known quotes such as “Listen to your patients, they are telling you the diagnosis”, “one finger in the throat and one finger in the rectum makes a good diagnostician” and The good physician treats the disease; the great physician treats the patient who has the disease. [2-4]. These simple yet profound statements sum up the value of holistic approach to patient assessment as a foundation for diagnosis and prioritizing care-an art which should not be overlooked by clinicians burdened by the daily stressors of private practice. The diagnostic process relies on the ability of a clinician to synthesize patient’s past medical history, presenting symptoms, risk factors and physical signs to develop a prioritized list of differential diagnoses. The latter would be narrowed down by gathering additional information or diagnostic testing until a definitive diagnosis is established [5]. A thorough history is not only the oldest, but also the most reliable element in the diagnostic work up [5-7]. An astute clinician is not only an active listener capable of eliciting pertinent information, but also observant of non-verbal clues critical to diagnosis during the medical interview [6, 7]. The review of systems, an important component of the medical interview, also helps clinicians identify health issues not yet diagnosed but potentially related to the current or future complaints [5] In a landmark study evaluating the relative importance of the medical history, the physical exam and diagnostic tests, physicians were able to predict accurately diagnosis in 66 of the 80 patients only after taking the medication history [7, 8].
A thorough physical exam starts with observing the patient for general appearance, symmetry, posture and nutritional status which is often reflective of physical and psychological health and disease [5]. The clinician then proceeds to visual inspection of exposed and non-exposed skin, nail and hair, palpation and percussion of body surfaces and auscultation of appropriate organs [5]. Clinical exam can often identify a pivotal clue which narrows down differential diagnoses, help select appropriate tests, and expedite accurate diagnosis without burdening patients with costly, unnecessary diagnostics [6, 7] In an observational study, Reily et al. Reported that a skilled physical exam offered a critical clue in 26% of patients which changed the diagnosis the medical diagnosis [9]. Although the scope of practice in dentistry differs from medicine, diagnostic approach is essentially the same. Dentists are skilled at taking histories, performing focused physical exams and chairside diagnostic tests when providing dental care. Since the relationship between oral and systemic health is reciprocal and multi-faceted, a holistic approach to patient assessment can also guide dental providers differentiate between oral abnormalities of local and systemic origin and decide on appropriate management. Recognition of an occult systemic pathosis by an astute oral physician could expedite diagnosis, reduce suffering and help improve medical outcomes. We report a patient in whom the onset of extra and intraoral purpuras raised the suspicion of a systemic disease and prompted medical referral. Unfortunately; however, the patient did not survive.
2. Case Report
A 93-year-old male presented to his private dentist reporting two-day onset of asymptomatic oral lesions which he attributed to traumatic biting while eating. He denied other jaw or facial trauma. The patient’s past medical history was significant for hypertension, diabetes, rheumatoid arthritis, thyroid disease, Coronary artery disease, cardiac stent placement and distant prostate cancer successfully treated with radiation. His medications included Glipizide, Atenolol, Clopidogrel, and Aspirin. He was allergic to sulfa drugs. He reported his last medical visit was three months prior to this presentation. Focused review of systems was positive for recent onset of multiple cutaneous and conjunctival discolorations. Extraoral exam revealed scleral hemorrhage in the left eye (Figure 1) and multiple hematomas affecting his arms, legs and upper lip. The patient related his skin bruises to everyday trauma and old age. He had seen an eye specialist regarding the conjunctival bleeding and been reassured it is likely related to a broken blood vessel which is more frequent in the elderly particularly in the context of therapy with antiplatelet agents. Noted intraorally were ecchymosis involving the floor of the mouth, tongue, labial and buccal mucosa (Figure 2). Focal areas of gingival oozing were also present. Radiographic exam was non-contributory.
Clinical impression was that mucocutaneous findings may be a manifestation of an underlying coagulopathy or a hematological disorder. The patient was advised to rinse with chilled saline to reduce gingival oozing and referred to his primary doctor for immediate evaluation and blood work. While awaiting the result of work up, the patient developed intracranial hemorrhage and expired shortly after. Although a definitive diagnosis remains undetermined, blood work revealed profound thrombocytopenia (platelet count=7000 cells/mm3) -a finding consistent with the patient’s clinical presentation.

Figure 1: Clinical photo of the patient’s left eye with subconjunctival hemorrhage.
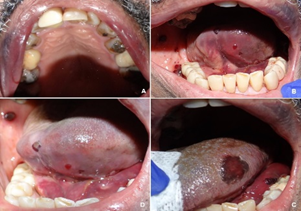
Figure 2: Clinical photo of the oral cavity illustrating multiple ecchymosis affecting the patient’s upper vermilion and labial mucosa, ventral tongue, left dorsolateral tongue, floor of mouth and right buccal mucosa.
3. Discussion
A broad spectrum of conditions such as hereditary, coagulopathic, and hematologic disorders may lead to impairment of hemostasis and a variety of manifestations in the orofacial region. Therefore; a working knowledge of pathological basis of various bleeding conditions, together with history, physical and blood work is necessary for determining the underlying etiology. Disorders of hemostasis may present as mucocutaneous pallor, jaundice, cyanosis, petechiae, telangiectasia, spider angiomas, ecchymoses, subconjunctival hemorrhage, epistaxis gingival bleeding, and prolonged bleeding following trauma or surgical procedures [10]. Signs and symptoms of bleeding diathesis in the oral cavity may occur spontaneously, provoked with minimal trauma such as mastication and tooth brushing or follow invasive procedures such as scaling or extractions. In this context, a bleeding episode lasting more than 12 hours, causing soft tissue ecchymosis/hematomas or requiring blood product support leading to an emergency visit or follow up care, may be considered clinically significant [10].
Potential causes of bleeding disorders include vascular anomalies, disorders of platelet number (thrombocytopenia) or function (thrombocytopathy), coagulation defects and fibrinolytic disorders, each of which give rise to specific clinical findings [10]. Vascular disorders such as scurvy or hereditary hemorrhagic telangiectasia are uncommon and are characterized by easy bruising and spontaneous bleeding from small vessels [10, 11]. Platelet disorders may be quantitative (affect the number) or qualitative (affect the function). Thrombocytopenia, a quantitative platelet disorder, may arise from decreased platelet production (e.g. Bone marrow failure, leukemia), or platelet destruction (e.g. idiopathic thrombocytopenia) [10]. Thrombocytopathy (altered platelet function) may
be hereditary (e.g. Von Willebrand disease) [11], drug- induced (e.g. ASA, clopidogrel) or related to a systemic condition (e.g. uremia in renal failure) [10]. Typical manifestations of platelet disorders include superficial petechiae, ecchymosis, spontaneous gingival hemorrhage, epistaxis [10-12] and immediate onset bleeding after surgical procedures [11].
Coagulation disorders may also be familial (e.g. hemophilia) [11], medication-induced (Coumadin, dabigatran, etc.) or related to an underlying liver disease (e.g. cirrhosis). Clinically, coagulation disorders often manifest with late bleeding, large ecchymosis, deep hematomas, and hemarthrosis [10, 11] Fibrinolytic defects could also impair the hemostatic process. Fibrinolytic defects may follow therapeutic interventions with drugs such as streptokinase or conditions causing fibrin depletion such as disseminated intravascular coagulation (DIC) [10]. When indicated, laboratory investigations such as complete blood count (CBC) and coagulation profile (PT, PTT, INR) help screen patients for deficiency of platelets or clotting factors, respectively. In general, in the absence of other complicating factors, routine and incremental oral surgery may be safely performed with platelet count > 50,000 /mm3, INR < 3.5 or PT/PTT within the normal range. Consultation with the patient’s physician is necessary when surgical procedures are planned and the above blood work is outside the acceptable limits.
Proper assessment of patients for bleeding tendencies starts with the medical interview inquiring about the family history, medications, prior experiences with trauma and surgical procedures (Table 1). It is important to question patients specifically about their use of over the counter vitamins and supplements [13]. Depending on the type and dose, these products may impair hemostasis directly or enhance the antiplatelet or anticoagulant action of prescription medications [13]. In this context, the inspection of oral mucosa, conjunctiva and the exposed skin could provide clues to the presence and nature of an underlying bleeding diathesis and help prioritize the diagnostic work up [11]. Initial recognition of a bleeding diathesis may, in fact, occur in a dental setting [11,12,14] and should prompt referral for medical evaluation.
This patient was an elderly with multiple medical problems and undergoing treatment with two antiplatelet agents. Nevertheless, the rapid and wide spread onset of mucocutaneous findings were disproportionate to possible trauma from daily functions and out of character for bleeding caused by his daily medications raising the suspicion of a faulty internal process. This case exemplifies the holistic approach to assessment of a patient with oral complaints which required interface with a medical counterpart for urgent management. Unfortunately, despite expedited referral to his internist, the serious nature of underlying condition led to the patient’s demise before medical evaluation could be completed. The explosion of our understanding of oral-systemic health connection in recent years provides an opportunity for dental professionals to play an even more integral role in holistic patient assessment and care. Dentists are well-positioned to help improve medical outcome by screening patients at risk for many systemic diseases or monitoring those already diagnosed during the dental visit [15]. This fits well with the recent shift in health care paradigm favoring delivery of comprehensive, quality and efficient patient-centered care through inter-professional communication and collaborative practice.
|
PERTINENT QUESTIONS |
RELEVANCE TO HEMOSTASIS |
|
Bleeding episodes following traumatic |
· Fall, cuts, scratches · Extractions, periodontal procedures |
|
Spontaneous bleeding episodes? |
· Gingival bleeding in severe thrombocytopenia (< 20,000 cells/mm3), |
|
Location & appearance of bleeding/bruising?
|
· Platelet disorders often manifest with petechia and small superficial |
|
Timing of bleeding? |
· Platelet disorders often cause Immediate post-op bleeding; |
|
Family history of bleeding disorders
|
· Identify hereditary bleeding tendencies such as |
|
Social history (alcoholism, IVDA)? |
· Risk of Hepatitis C-induced liver disease, risk of alcoholic liver disease |
|
Systemic diseases? |
· Identify bleeding tendencies caused by hepatic, renal or hematological disorders) |
|
Medications? |
· Anticoagulants (e.g. Coumadin) or antiplatelet agents (eg. Plavix) |
|
Herbal supplements (Ginko biloba, Garlic, etc.) |
· Supplements can affect platelet function, coumadin metabolism, etc. |
|
Malabsorption or nutritional problems? |
· Vitamin K or C deficiency may impair hemostasis |
|
Broad spectrum antibiotics |
· Destroy gut flora producing vitamin K |
|
Current or recent chemotherapy? |
· bone marrow suppression & thrombocytopenia? |
Table 1: A summary of pertinent questions which may help identify potential impairments in hemostasis during the medical interview [10.11.13].
4. Conclusion
A correct clinical impression is integral to initiation of an appropriate management as exemplified in this patient. Dental providers should perform a holistic patient assessment, maintain a high index of suspicion for an occult systemic etiology and expedite referral for medical evaluation when a patient presents with signs and symptoms affecting oral and extra-oral sites. At times, timely consideration of this possibility could be life-saving.
References
- Profiles in Science. US National Library of Medicine.
- 10 Osler-isms to Remember in Your Daily Practice (2014).
- Centor RM. To be a great physician, you must understand the whole story. Med Gen Med 9 (2007): 59.
- Pitkin RM. Listen to the patient. BMJ 316 (1998): 1252.
- Rakel RE. Diagnostic Medicine.
- Sanders L. Every Patient Tells a Story. New York: Broadway Books (2009): 6-91.
- Muhrer Jill. The importance of the history and physical in diagnosis. The Nurse Practitioner 39 (2014): 30-35.
- Hampton JR, Harrison MJ, Mitchell JR, Prichard JS, Seymour C. Relative contributions of history-taking, physical exam, and lab investigation to diagnosis and management of medical outpatients. Br Med J 2 (1975): 486-489.
- Reilly BM. Physical examination in the care of medical inpatients: an observational study. Lancet 362 (2003): 1100-1105
- Gupta A, Epstein J, Cabay R. Bleeding Disorders of Importance in Dental Care and Related Patient Management. JCDA 73 (2007): 77-83.
- Adeyemo TA, Adeyemo WL, Adediran A, Akinbami AA, Akanmu AS. Orofacial manifestations of hematological disorders: Anemia and hemostatic disorders. Indian J Dent Res 22 (2017): 454-61.
- Martini MZ, Lopez JS Jr, Gendler JL, da Fonseca EV, Soares HA, et al. Idiopathic Thrombocytopenic Purpura Presenting as Post-extraction Hemorrhage. J Contempt Dent Pac 8 (2007): 43-49.
- Wong W, Gabriel A, Maxwell P, and Gupta S. Bleeding Risks of Herbal, Homeopathic, and Dietary Supplements: A Hidden Nightmare for Plastic Surgeons? Aesthetic Surg Journal 32 (2012): 332-346.
- Bal MV, Koyuncuoglu JZ, Saygun I. Immune Thrombocytopenic Purpura Presenting as Unprovoked Gingival Hemorrhage: A Case Report. The Open Dentistry Journal 8 (2014): 164-167.
- Branch-mays GL, Mays KA. Achieving Patient-centered Care through Interprofessional Collaborative Practice.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 