Distribution of Treatments by Age of Patients at an Academic Dental Center
Article Information
Kadhium VS*, Sharma P, Josan NK, Mhay S, Dault J, Nalliah RP
University of Michigan School of Dentistry, USA
*Corresponding Author: Viyan Sabah Kadhium, University of Michigan School of Dentistry, 1011 N. University, Ann Arbor, MI, 48109, USA
Received: 04 May 2022; Accepted 12 May 2022; Published: 19 May 2022
Citation: Kadhium VS, Sharma P, Josan NK, Mhay S, Dault J, Nalliah RP. Distribution of Treatments by Age of Patients at an Academic Dental Center. Dental Research and Oral Health 5 (2022): 011-020.
View / Download Pdf Share at FacebookAbstract
Objective
To identify the most common dental treatments in each age group at the University of Michigan School of Dentistry by evaluating electronic health record data at the University of Michigan School of Dentistry clinics.
Methods
All American Dental Association Code on Dental Procedures and Nomenclature data were extracted from the electronic health record at the University of Michigan School of Dentistry for the period 2014-2020.
Results
Comprehensive oral examination (D0150) and periodic oral evaluation (D0120) were the most common procedures for age bracket 0-9 years at 1,497 and 1,786 per 10,000 patients respectively. Ages 30-39 experienced a surge in extractions (D7140) (4,680 extractions per 10,000 patients). In age 50-59, adult prophylaxis (D1110) is highest with 9,124 per 10,000 patients
Conclusions
With proper care and treatment at every stage of life, teeth can stay healthy and strong for a lifetime.
Keywords
Lifespan, Epidemiology, Public Health, Access
Lifespan articles; Epidemiology articles; Public Health articles; Access articles
Lifespan articles Lifespan Research articles Lifespan review articles Lifespan PubMed articles Lifespan PubMed Central articles Lifespan 2023 articles Lifespan 2024 articles Lifespan Scopus articles Lifespan impact factor journals Lifespan Scopus journals Lifespan PubMed journals Lifespan medical journals Lifespan free journals Lifespan best journals Lifespan top journals Lifespan free medical journals Lifespan famous journals Lifespan Google Scholar indexed journals Epidemiology articles Epidemiology Research articles Epidemiology review articles Epidemiology PubMed articles Epidemiology PubMed Central articles Epidemiology 2023 articles Epidemiology 2024 articles Epidemiology Scopus articles Epidemiology impact factor journals Epidemiology Scopus journals Epidemiology PubMed journals Epidemiology medical journals Epidemiology free journals Epidemiology best journals Epidemiology top journals Epidemiology free medical journals Epidemiology famous journals Epidemiology Google Scholar indexed journals Public Health articles Public Health Research articles Public Health review articles Public Health PubMed articles Public Health PubMed Central articles Public Health 2023 articles Public Health 2024 articles Public Health Scopus articles Public Health impact factor journals Public Health Scopus journals Public Health PubMed journals Public Health medical journals Public Health free journals Public Health best journals Public Health top journals Public Health free medical journals Public Health famous journals Public Health Google Scholar indexed journals Dental articles Dental Research articles Dental review articles Dental PubMed articles Dental PubMed Central articles Dental 2023 articles Dental 2024 articles Dental Scopus articles Dental impact factor journals Dental Scopus journals Dental PubMed journals Dental medical journals Dental free journals Dental best journals Dental top journals Dental free medical journals Dental famous journals Dental Google Scholar indexed journals Dentistry articles Dentistry Research articles Dentistry review articles Dentistry PubMed articles Dentistry PubMed Central articles Dentistry 2023 articles Dentistry 2024 articles Dentistry Scopus articles Dentistry impact factor journals Dentistry Scopus journals Dentistry PubMed journals Dentistry medical journals Dentistry free journals Dentistry best journals Dentistry top journals Dentistry free medical journals Dentistry famous journals Dentistry Google Scholar indexed journals oral health articles oral health Research articles oral health review articles oral health PubMed articles oral health PubMed Central articles oral health 2023 articles oral health 2024 articles oral health Scopus articles oral health impact factor journals oral health Scopus journals oral health PubMed journals oral health medical journals oral health free journals oral health best journals oral health top journals oral health free medical journals oral health famous journals oral health Google Scholar indexed journals oral examination articles oral examination Research articles oral examination review articles oral examination PubMed articles oral examination PubMed Central articles oral examination 2023 articles oral examination 2024 articles oral examination Scopus articles oral examination impact factor journals oral examination Scopus journals oral examination PubMed journals oral examination medical journals oral examination free journals oral examination best journals oral examination top journals oral examination free medical journals oral examination famous journals oral examination Google Scholar indexed journals Periodontal maintenance articles Periodontal maintenance Research articles Periodontal maintenance review articles Periodontal maintenance PubMed articles Periodontal maintenance PubMed Central articles Periodontal maintenance 2023 articles Periodontal maintenance 2024 articles Periodontal maintenance Scopus articles Periodontal maintenance impact factor journals Periodontal maintenance Scopus journals Periodontal maintenance PubMed journals Periodontal maintenance medical journals Periodontal maintenance free journals Periodontal maintenance best journals Periodontal maintenance top journals Periodontal maintenance free medical journals Periodontal maintenance famous journals Periodontal maintenance Google Scholar indexed journals orthodontic treatment articles orthodontic treatment Research articles orthodontic treatment review articles orthodontic treatment PubMed articles orthodontic treatment PubMed Central articles orthodontic treatment 2023 articles orthodontic treatment 2024 articles orthodontic treatment Scopus articles orthodontic treatment impact factor journals orthodontic treatment Scopus journals orthodontic treatment PubMed journals orthodontic treatment medical journals orthodontic treatment free journals orthodontic treatment best journals orthodontic treatment top journals orthodontic treatment free medical journals orthodontic treatment famous journals orthodontic treatment Google Scholar indexed journals
Article Details
1. Introduction
Most individuals have two sets of teeth in their life: primary (baby) and permanent (adult) teeth. In a baby’s first year of life there are many firsts- a first step, first words and first teeth. A baby’s first tooth usually appears around 6 months of age (primary central incisor) [1] and the American Dental Association (ADA) [2] and the American Academy of Pediatric Dentistry (AAPD) [3] currently recommend that all children have their first dental visit after the eruption of their first tooth (6 months) and no later than 12 months. Because cariogenic bacteria (especially mutans streptococci) are transmitted soon after the eruption of the first tooth making primary teeth more susceptible to decay as soon as they appear in the mouth [2,3]. A study showed that the timing of initial detection of mutans streptococci varies between 7 and 36 months [4], and studies have linked mutans streptococci detection to the time period coinciding with the eruption of the primary teeth [5,6]. One of the most common misconceptions about primary teeth is that they are irrelevant to child’s future oral health. Primary teeth may be temporary, but they play an important role for the eruption and health of their permanent successors [7,8] and in the function of mastication and phonation9 and can even instill a sense of confidence. In an 8-year prospective study [10] done in China, the epidemiology of caries in children was observed and they found 94% of the children with carious primary teeth also exhibited carious lesions in their permanent teeth, while 83% of the children with a caries- free primary dentition remained caries-free in the permanent dentition. Early childhood caries (ECC) is a major oral health concern, mainly in socially disadvantaged populations with a prevalence of 85% according to one reported [11]. The main risk factors in the development of ECC can be categorized as microbiological, dietary, and environmental risk factors. The major contributing factors for the high prevalence of ECC are improper feeding practices, familial socioeconomic background, lack of parental education and lack of access to dental care. ECC/dental caries is one of the most prevalent chronic dental diseases in children younger than 6 years old [12,13], in children aged 6 to 11 years old and adolescents aged 12 to 19 years old [14]. Research has stated and proven the same notion, that poor oral health and dental disease often continue into adulthood [15,16]. According to the Centers for Disease Control (CDC), 26% of adults in the United States (U.S.) have untreated tooth decay, and 46% of all adults aged 30 years or older show signs of gum disease; severe gum disease affects about 9% of adults [17]. Just as oral health conditions change with age, so do the risk factors- social and physical. Dental benefits coverage varies by age. Medicaid and the Children’s Health Insurance Program (CHIP) play a vital role in providing American children with health insurance and enrollment varies state to state. In 2017, 46.3 million children were either enrolled in Medicaid or CHIP and as of July 2020, 36.6 million children were enrolled in Medicaid or CHIP [18]. Despite coverage by Medicaid and the Affordable Care Act (ACA) expansion, which covers children’s dental care but not adults, access to dental care still poses an issue for children from low-income, minority, and rural communities. In 2014, More than 18 million low-income children went without dental care [19]. In Adults, dental benefits are optional under Medicaid. According to the Health Policy Institute, 59.0% have private dental benefits, 7.4% have dental benefits through Medicaid, and 33.6% do not have dental benefits [20]. Low-income or uninsured adults are twice as likely to have one to three untreated cavities and three times as likely to have four or more untreated cavities as adults with higher incomes or private insurance [21]. Access to care is also an issue across all age groups. As of 2019, only about 43% of dentists in the U.S. accept Medicaid or CHIP [22]. More people are unable to afford dental care than any other types of health care [23]. Older Americans with poorest oral health tend to be those who are economically disadvantaged, lack insurance and are members of ethnic and racial minorities. Being disabled, homebound or institutionalized (e.g., seniors who live in nursing homes) also increase the risk of poor health. Finally, adults 50 years or more who smoke are less likely to get dental care than people who do not smoke [24]. Another risk factor is underlying chronic conditions that occur with age. About 80% of older adults have at least one chronic condition and 77% have at least two [25]. Diabetes is one of the most common chronic conditions found in adults. In 2018, 34.2 million Americans had diabetes and of those 7.3 million were undiagnosed [26]. There is a bi-directional relationship between diabetes and periodontitis. Diabetes is a major risk factor for periodontal disease and severe periodontal disease also can increase the risk of developing diabetes [27]. Other oral manifestations include- xerostomia; burning sensation in the mouth; impaired/delayed wound healing; and increased incidence and severity of infections [28]. There is evidence that demonstrates a relationship between general health and oral health of patients with diabetes [28,29]. Emerging evidence suggests that poor oral health influences the initiation and/or progression of diseases such as atherosclerosis (with sequelae including myocardial infarction and stroke), neurodegenerative disease (such as Alzheimer’s disease, rheumatoid arthritis, and others) [30]. Aspiration of oropharyngeal (including periodontal) bacteria can cause pneumonia, especially in hospitalized patients and the elderly [31]. In 2000, the first Surgeon General’s Report on oral health (the second is in progress) made clear that oral health is part of overall health and well- being [30]. Good oral health is critical for effective eating, speaking, smiling, and quality of life. Oral and general health go hand in hand and it’s important for patients with chronic conditions to get regular dental visits to prevent negative oral health outcomes. The primary goal of this study is to highlight the most common treatments among different age groups at the University of Michigan School of Dentistry (UOMSOD). By identifying the most common treatments in each age range, our goal is to determine focused early interventions in earlier age ranges in order to prevent poor oral health outcomes in later age ranges.
2. Materials and Methods
This is, primarily, a quasi-experimental evaluation and the overarching goal was to determine the most common treatments in each area and consider opportunities and synergies for optimizing the care of patients in each age group in the U.S. University of Michigan School of Dentistry uses Axium electronic health records which is an Exan product [32]. We extracted all de-identified data of procedures (as documented by ADA CDT treatment codes) delivered between January 2014 to July 2020 in the University of Michigan School of Dentistry clinics. We identified the seven most common treatments in each age bracket 0-9; 10-19; 20-29; 30-39; 40-49; 50-59; 60-69; 70-79; 80-89; 90-99. We did not use any patient identifying data. Our goal is to identify the most common treatments delivered to each age group. The Committee on Human Subjects research evaluated the research proposal and deemed this study as IRB exempt (HUM00188624).
3. Results
We summed the total number of visits, ages, and treatments from 2014-2020 to identify the most common treatments in each age range at the University of Michigan School of Dentistry. From 0-9 years of age comprehensive oral examination (D0150) (Figure 1) and periodic oral evaluation (D0120) (Figure 1) were the top procedures at 1,497 and 1,786 per 10,000 patients respectively. For ages 10-19, periodic orthodontic treatment visits (D8670) (figure 2) were the highest with 6,936 visits per 10,000 patients followed by the 20-29 years age group at 631per 10,000 patients. For 20-29 years of age, a comprehensive oral exam (D0150)) was the most common treatment (1,134 per 10,000 patients) (Figure 1). Ages 30-39 experienced a surge in extractions (D7140) (Figure 2), there were 4,680 extractions per 10,000 patients which all seemed unrelated to orthodontics or wisdom tooth removal. The following age group 40-49 years had 2,530 extractions per 10,000 patients also unrelated to orthodontics or wisdom tooth removal (Figure 2). In ages 50-59, adult prophylaxis (D1110) (Figure 2) was the highest with 9,124 per 10,000 patients. Periodontal maintenance (D4910) (Figure 2) was the most common for ages 60-69 with 525 per 10,000 patients, 70-79 years at 616 per 10,000 patients and 80-89 years at 627 per 10,000 patients. For ages 90-99, extractions (Figure 2) were the most common treatment at a rate of 2,139 extractions per 10,000 patients.
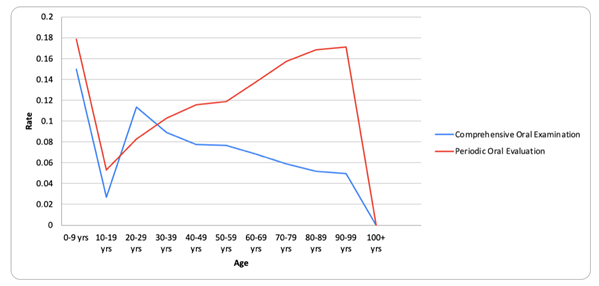
Figure 1: Oral examination
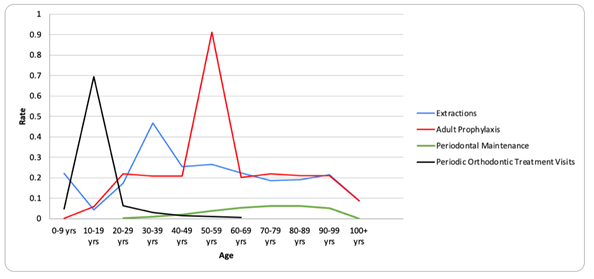
Figure 2: Treatments
4. Discussion
Dental school clinics play a very important role in patient care. According to a 2020-21 ADA report [33], dental students in the US provided 2,349,841 patient visits, 330,656 of which were extramural clinics. The UOMSOD provided the second-highest number of patient visits (100,968) among all U.S. universities. Furthermore, UOMSOD serves 82 of the 83 counties in Michigan [34] and accepts most major dental insurances. Lastly, UOMSOD provides every specialty and has a special care clinic as well as a community health center [35]. UOMSOD, therefore, plays a vital role in the oral health of Michigan. For this reason, our goal was to understand whether we could identify common issues in certain age groups and address them before they arise. Parents play a big role in oral healthcare among children [36]. Furthermore, regular dental visits are important not only to help children create good oral health habits but also to help detect oral health problems early [37,38]. Our study found that for age group 0-9 years of age, comprehensive oral examination and periodic oral evaluation were the top procedures at 1,497 and 1,786 per 10,000 patients, respectively. A 2021 study [39], that looked at patient attendance, failure, and cancellation at the UOMSOD found that children aged under 12 had significantly better attendance compared to other age groups. One reason for this could be linked to the current generation of parents- millennials [40]. Millennial parents are more likely to invest in their children’s oral healthcare compared to their boomer parents [41]. According to a survey done by the AAPD, 29% of millennial parents are more likely to take their child to the dentist by age 1 than any other generation [42]. Another reason could be because of insurance. Under the ACA, all children under the age of 19 must be covered by dental insurance, it one of the ten essential health benefits [43]. Lastly, Michigan and a few other states are now requiring parents to provide some form of certification of a dental screening, examination, or assessment prior to elementary and/or high school [44,45]. Our study found that the most common treatment for 20-29 years of age was a comprehensive oral exam at a rate of 1,134 per 10,000 patients. One possible reason for this low rate could be due to insurance and income. According to the Michigan Household Survey on Health Insurance [46], adults aged 20-29 have the highest rate of lack of insurance (26%), and more than a quarter of the uninsured live below the poverty line. While the UOMSOD does provide dental services at a lower cost compared to market prices [47], like most dental schools [48], and has a check-up clinic that offers basic cleaning and x-rays for $102 [49], the minimum wage in the state of Michigan is $9.87 [50]. Even these prices, therefore, can be expensive for low-income individuals. According to one study, two of the top three reasons for not visiting a dentist for adults ages 18-34, were cost and lack of time to get a dentist; 35.7%, and 28.4%, respectively [51]. Furthermore, in Michigan’s Medicaid plan, adult dental benefits are limited [52], which could explain why the most common treatment was a comprehensive oral exam, which is included in the plan. This can be a problem because untreated oral health problems, such as caries and periodontitis, may lead to tooth loss [53]. Interestingly, we found that adults aged 30-39 and 40-49 experienced a surge in routine extractions that were unrelated to orthodontics or wisdom tooth removal: 4,680 extractions per 10,000 patients and 2,530 extractions per 10,000 patients, respectively. According to one study done in 1997 and most likely still hold true to today, most patients receiving care at dental schools are low-income [54]. In 2020, 13% of Michigan residents lived below the poverty line [55]. The high rate of extractions among this age group could thus be due to the relationship between income and tooth loss, which many studies have shown [56,57]. Another reason could be untreated tooth decay, given that, as previously stated, the rate of comprehensive oral exams was low among those aged 20-29, and untreated tooth decay can lead to tooth loss [58]. Gingivitis is the most basic form of gum disease and is treatable through periodontal maintenance which includes personal and professional care. But, if left untreated can advance to periodontitis, the more severe form of gum disease [59]. Regular dental check-ups help to prevent or control the disease. Our study showed that adult prophylaxis (D1110) was the highest in ages 50–59, with 9,124 per 10,000 patients. Periodontal maintenance (D4910) was most common among those aged 60–69, 70–79, and 80–89, with 525 per 10,000 patients, 616 per 10,000 patients, and 627 per 10,000 patients, respectively. This high rate of adult prophylaxis for ages 50–59 may be a result of the fact that this age group is still covered by Medicaid, which provides prophylaxis twice a year in Michigan. The low rates of periodontal maintenance from ages 60 to 89 could be due to the lack of dental insurance for those aged 65 or older. Medicare only covers medically necessary dental procedures [60] and according to a report done by the National Poll on Healthy Aging, just 53% of people over the age of 65 have dental coverage, while the other half have no dental coverage [61]. A possible reason for periodontal maintenance being the top procedure among those aged 55–64 could be that periodontal disease tends to relate to age. According to the CDC, 70.1% of adults aged 65 or older have periodontal disease [62]. One study that estimated the prevalence, severity, and extent of periodontitis in the USA found that 47.2% of residents have mild, moderate, or severe periodontitis and that the prevalence rates increase to 70.1% for adults aged 65 or older [63]. Furthermore, older patients are more likely to develop chronic conditions [64] that can affect their periodontal health, like diabetes, a weakened immune system, neurodegenerative disease, and heredity increases the risk of developing periodontal disease as they age [65]. Lastly, another reason could be lack of regular dental visits. Rosén et al. [66] found that patients who didn’t visit a dentist at least once annually were more susceptible to periodontal progression. In severe cases, periodontitis can lead to tooth loss [67]. In our study, we found that extractions were the most common treatment for ages 90-99, at a rate of 2,139 extractions per 10,000 patients. A contributing factor for tooth loss in this age group is medication, which commonly causes xerostomia [68]. About 89% adults 65 and older report they are currently taking prescription medicine [69] and more than 400 commonly used drugs have xerostomia as one of their side effects [70]. Findings of a 2013 screening done on senior citizens living in Michigan showed that 17% of seniors suffered from severe dry mouth (xerostomia), 17% had untreated tooth decay, and 13% had root fragments. Lastly, a decline in cognitive function (e.g., Alzheimer’s) may be another reason. According to the Alzheimer’s association, Alzheimer’s is a growing public health crisis in Michigan - 190,000 people aged 65 and older have Alzheimer’s disease in Michigan. There are many studies showing the link between dementia and tooth loss.
5. Conclusion
Poor oral health is largely preventable through regular annual dental visits to help maintain teeth. Interventions that enhance access to prevention in the 20-29 age group could improve oral health outcomes and tooth preservation. Similarly, enhanced access to periodontal specific preventive care in ages 50-59 may reduce or delay the onset of periodontal disease which also has implications for systemic health. With proper care and treatment at every stage of life, teeth can stay healthy and strong for a lifetime. Proper maintenance of oral health is very important and should be started young because it influences future oral health conditions.
Conflict of interest
All authors agree to no conflict of interest.
References
- ADA Division of Communications, Journal of the American Dental Association, ADA Council on Scientific Affairs. For the dental patient. Tooth eruption: The primary teeth. J Am Dent Assoc 136 (2005): 16-19.
- American Dental Association. Statement on Early Childhood Caries (2020).
- American Academy of Pediatrics. Recommendations for Preventive Pediatric Health Care (2020).
- Law V, Seow WK, Townsend G. Factors influencing oral colonization of mutans streptococci in young children.Aust Dent J 52 (2007): 93-159.
- Carlsson J, Grahnén H, Jonsson G. Lactobacilli and streptococci in the mouth of children.Caries Res 9 (1975): 333-339.
- Xu H, Hao W, Zhou Q, et al. Plaque bacterial microbiome diversity in children younger than 30 months with or without caries prior to eruption of second primary molars.PLoS One 9 (2014): e89269.
- American Academy of Pediatric Dentistry. Management of the Developing Dentition and Occlusion in Pediatric Dentistry. The Reference Manual of Pediatric Dentistry. American Academy of Pediatric Dentistry 12 (2020): 393-409.
- ADA Division of Communications, Journal of the American Dental Association, ADA Council on Scientific Affairs. For the dental patient. Tooth eruption: the permanent teeth.J Am Dent Assoc 137 (2006): 127.
- Zimmerman B, Jenzer AC. Physiology, Tooth. In:StatPearls. Treasure Island (FL): StatPearls (2018).
- Li Y, Wang W. Predicting caries in permanent teeth from caries in primary teeth: an eight-year cohort study.J Dent Res 81 (2002): 561-566.
- Anil S, Anand PS. Early Childhood Caries: Prevalence, Risk Factors, and Prevention.Front Pediatr 5 (2017): 157.
- Meyer F, Enax J. Early Childhood Caries: Epidemiology, Aetiology, and Prevention.Int J Dent 12 (2018): 1415873.
- Beil H, Rozier RG, Preisser JS, et al. Effect of early preventive dental visits on subsequent dental treatment and expenditures.Med Care 50 (2012): 749-756.
- Dentistry Today. CDC Releases Latest Childhood Caries Report (2017).
- Jordan AR, Becker N, Jöhren HP, et al. Early Childhood Caries and Caries Experience in Permanent Dentition: A 15-year Cohort Study.Swiss Dent J 126 (2016): 114-119.
- Broadbent JM, Foster Page LA, Thomson WM, et al. Permanent dentition caries through the first half of life.Br Dent J 215 (2013): E12.
- Centers for Disease Control and Prevention. Adult Oral Health (2020).
- Kaiser Family Foundation. Monthly Child Enrollment in Medicaid and CHIP (2021).
- Grant J, Peters A. Children’s Dental Health Disparities (2021).
- American Public Health Association. A Call for Adult Dental Benefits in Medicaid and Medicare (2020).
- Williams S, Wei L, Griffin SO, et al. Untreated caries among US working-aged adults and association with reporting need for oral health care.J Am Dent Assoc 152 (2021): 55-64.
- American Dental Association. Dental Benefits and Medicaid (2021).
- Vujicic M, Buchmueller T, Klein R. Dental Care Presents The Highest Level Of Financial Barriers, Compared To Other Types Of Health Care Services.Health Aff (Millwood) 35 (2016): 2176-2182.
- Patel N, Fils-Aime R, Li CH, et al. Prevalence of Past-Year Dental Visit Among US Adults Aged 50 Years or Older, With Selected Chronic Diseases, 2018.Prev Chronic Dis 18 (2021): E40.
- National Council on Aging. The Top 10 Most Common Chronic Conditions in Older Adults (2021).
- American Diabetes Association. Statistics About Diabetes (2021).
- American Dental Hygienists’ Association. Oral Health-Total Health: Know the Connection (2021).
- Lamster IB, Lalla E, Borgnakke WS, et al. The relationship between oral health and diabetes mellitus.J Am Dent Assoc 139 (2008): 19-24.
- Kane SF. The effects of oral health on systemic health.Gen Dent 65 (2017): 30-34.
- US Department of Health and Human Services. Oral health in America: a report of the Surgeon General (2020).
- Scannapieco FA, Cantos A. Oral inflammation and infection, and chronic medical diseases: implications for the elderly.Periodontol 72 (2016): 153-175.
- Exan software company website (2021).
- University of Michigan School of Dentistry website. Quick Facts (2022).
- American Academy of Pediatric Dentistry. Periodicity of examination, preventive dental services, anticipatory guidance/ counseling, and oral treatment for infants, children, and adolescents. American Academy of Pediatric Dentistry 16 (2021): 241-251.
- Hale KJ. American Academy of Pediatrics Section on Pediatric Dentistry. Oral health risk assessment timing and establishment of the dental home.Pediatrics 111 (2003): 1113-1116.
- Weber K, DaSilva AF, Dault JT, et al. Using business intelligence and data visualization to understand the characteristics of failed appointments in dental school clinics.J Dent Educ 85 (2021): 521-530.
- Livingston G. More than a million Millennials are becoming moms each year (2018).
- Sanger RG. Selling Pediatric dental treatment to millennial parents (2017).
- New Survey by America's Pediatric Dentists Highlights Gaps in Oral Health Knowledge and Generational Differences in Caring for Little Teeth (2018).
- Norris L. Is pediatric dental coverage included in exchange plans? (2021).
- Children's Dental Health Project, Association of State and Territorial Dental Directors. State Laws on Dental “Screening” for School-Aged Children (2021).
- House Fiscal Agency. Dental screening of children (2021).
- State of Michigan. Who Are the Uninsured in Michigan? (2022).
- University of Michigan School of Dentistry website. Patient Care (2022).
- Weaver RG, Valachovic RW. ADEA survey of clinic fees and revenue: 2003-04 academic year.J Dent Educ 70 (2006): 448-462.
- University of Michigan School of Dentistry website. Checkup Clinic (2022).
- Yarbrough C, Nasseh,K, Vujicic M. Why adults forgo dental care: Evidence from a new national survey (2021).
- Delta Dental. Health Michigan Dental Plan- Handbook (2021).
- Griffin SO, Jones JA, Brunson D, et al. Burden of oral disease among older adults and implications for public health priorities.Am J Public Health 102 (2012): 411-418.
- Damiano PC, Warren JJ. A profile of patients in six dental school clinics and implications for the future.J Dent Educ 59 (1995): 1084-1090.
- Talk poverty. Michigan (2022).
- Seerig LM, Nascimento GG, Peres MA, et al. Tooth loss in adults and income: Systematic review and meta-analysis.J Dent 43 (2015): 1051-1059.
- Bernabé E, Marcenes W. Income inequality and tooth loss in the United States.J Dent Res 90 (2011): 724-729.
- Elani HW, Harper S, Thomson WM, et al. Social inequalities in tooth loss: A multinational comparison.Community Dent Oral Epidemiol 45 (2017): 266-274.
- Rosen PS, American Academy of Periodontology-Research, Scicence and therapy Committee. Treatment of plaque-induced gingivitis, chronic periodontitis, and clinical conditions.Pediatr Dent 30 (2008): 253-262.
- Dental services (2021).
- Gavin K. With Half of Adults Over 65 Lacking Dental Insurance, Poll Finds Strong Support for Universal Medicare Dental Benefit. M Health Lab (2020).
- Centers for Disease Control and Prevention. Periodontal Disease (2021).
- Eke PI, Dye BA, Wei L, et al. Prevalence of periodontitis in adults in the United States: 2009 and 2010.J Dent Res 91 (2012): 914-920.
- Atella V, Piano MA, Kopinska J, et al. Trends in age-related disease burden and healthcare utilization.Aging Cell 18 (2019): e12861.
- Miricescu D, Totan A, Stanescu LL, et al. Periodontal Disease and Systemic Health. Ro Med J 66 (2019): 197-201.
- Rosén B, Olavi G, Badersten A, et al. Effect of different frequencies of preventive maintenance treatment on periodontal conditions. 5-Year observations in general dentistry patients.J Clin Periodontol 26 (1999): 225-233.
- Meyer MS, Joshipura K, Giovannucci E, et al. A review of the relationship between tooth loss, periodontal disease, and cancer.Cancer Causes Control 19 (2008): 895-907.
- Enoki K, Matsuda KI, Ikebe K, et al. Influence of xerostomia on oral health-related quality of life in the elderly: a 5-year longitudinal study.Oral Surg Oral Med Oral Pathol Oral Radiol 117 (2014): 716-721.
- Kirzinger A, Neuman T, Cubanski J, et al. Data Note: Prescription Drugs and Older Adults (2019).
- The Oral Cancer Foundation. Xerostomia (2021).
- Van Beek M, Davidson J. Dental Therapists: A Proposal to Expand Access to Dental Care in Michigan (2016).
- Alzheimer’s Association. Michigan (2022).
- Chen X, Shuman SK, Hodges JS, et al. Patterns of tooth loss in older adults with and without dementia: a retrospective study based on a Minnesota cohort.J Am Geriatr Soc 58 (2010): 2300-2307.
- Thomson WM, Barak Y. Tooth Loss and Dementia: A Critical Examination.J Dent Res 100 (2021): 226-231.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 