ECG Changes and Their Prognostic Impact in Patients With Takotsubo Syndrome
Article Information
Edita Piackova1,2*#, Christoph C. Kaufmann1,2*#, Valerie Weihs1,2, Abd El-Razek3, Alexander Geppert1,2, Michael Nürnberg1,2, Emil Wessely1,2, Peter Smetana1,2, Thomas Weiss1,2,3, Kurt Huber1,2,3
13rd Department of Medicine, Cardiology and Intensive Care Medicine, Austria
2 Ludwig Boltzmann Institute for Interventional Cardiology and Rhythmology, Austria
3Sigmund Freud University, Medical School, Vienna, Austria
*Corresponding author(s): Edita Piackova, 3rd Medical Department, Cardiology and Intensive Care Medicine, Austria Christoph Clemens Kaufmann, 3rd Medical Department, Cardiology and Intensive Care Medicine, Wilhelminenhospital, Montleartstrasse 37, A-1160 Vienna, Austria.
# - Both of the authors have contributed equally.
Received: 12 November 2019; Accepted: 22 November 2019; Published: 11 December 2019
Citation: Edita Piackova1, Christoph C. Kaufmann, Valerie Weihs, Abd El-Razek, Alexander Geppert, Michael Nürnberg, Emil Wessely, Peter Smetana, Thomas Weiss, Kurt Huber. ECG Changes and Their Prognostic Impact in Patients With Takotsubo Syndrome. Cardiology and Cardiovascular Medicine 3 (2019): 438-449.
View / Download Pdf Share at FacebookAbstract
Aim: Within this study, we investigated ECG changes in acute patients diagnosed with Tako Tsubo syndrome (TTS) and report on the prognostic impact of the respective ECG patterns.
Methods and Results: This single-center study included 101 consecutive patients diagnosed with TTS between 2006 and 2017. Upon 12-lead admission ECG, 59 patients had ST-segment elevation (58%, STEMI), 9 patients had only ST-segment depression (9%, NSTEMI) and 27 T-wave inversion (27%, NSTEMI). Patients who were admitted to the hospital 12 hours after symptom onset were more likely to present with Twave inversion on ECG (T-inversion 47% vs. STelevation 23% ST, p= 0,05). T-wave inversion was also associated with significantly higher values of NT-pro- BNP (p=0,024), while high-sensitive cardiac troponin I (hs-CTnI) and creatine kinase (CK) were comparable between the groups. There was no difference in ECG changes among the different types of TTS (apical, midventricular, apical-midventricular and basal type). In a second step, patients with ST-segment elevation were divided into three groups based on the pattern of STsegment elevation: Group A (concave type, n=35), group B (straight type, n=8) and group C (convex type, n=10), respectively. Straight type ST-segment elevation was associated with a higher incidence of in-hospital MACE (p = 0,002), while patients with convex type STelevation were hospitalized for a longer time (p= 0,010). There was no difference in three-year all-cause mortality based on repolarization abnormalities ((χ2(2) = 0,839, p=0,657) or the pattern of ST-elevation ((χ2(2) = 0,501, p=0,778).
Conclusion: The present study describes typical ECG changes in TTS and highlights their impact on cardiac biomarkers and clinical outcomes. There was no prognostic difference between ST-elevation, STdepression or T-wave inversion at admission ECG, however straight-type pattern of ST-segment elevat
Keywords
TakoTsubo syndrome; ST-segment elevation pattern; ECG; In-hospital complications; MACE; All-cause mortality; NT-pro-BNP; Troponin I
Article Details
Introduction
Takotsubo Syndrome (TTS), commonly referred to as broken-heart syndrome or stress-cardiomyopathy, is defined by transient, circumferential regional wall motion abnormalities in the absence of a culprit coronary artery lesion. Patients, in >90 % postmenopausal women, typically present with a sudden onset of retrosternal chest pain or dyspnea accompanied
by new electrocardiographic abnormalities, and mimicking acute myocardial infarction [1,2]. High prevalence rates of up to 1,2 – 2,0% have been reported among patients presenting as suspected acute coronary syndrome (ACS), making TTS an important differential diagnosis in the evaluation of patients with acute chest pain [3,4].
While TTS was generally considered a benign, reversible condition, there is a justified reason for caution [5]. Substantial rates of in-hospital complications and long-term mortality were observed in this setting. Therefore, tools to predict clinical outcome have been developed in order to stratify patients into low- and high-risk groups. Persistent ST-segment elevation, prolonged QTc-interval and the presence of Q waves have been shown to be associated with an increased risk of in-hospital mortality. Accordingly, an early detection of high-risk patients should be strongly considered [6,7].
Several studies have reported on electrocardiographic findings in patients with TTS. Typical presentation includes ST-segment elevation or T-wave inversion, while the number of patients presenting with ST- depression is comparably low [8–11]. In anterior ST- elevation myocardial infarction (STEMI), the pattern of ST-segment elevation (concave-, straight- or convex- type) serves as a prognostic marker. In acute STEMI non-concave ST-segment elevation is suggestive of worse left ventricular function, larger infarction size and a higher rate of in-hospital complications [12–14]. To our knowledge, there is no data available about the clinical implications of such different ECG patterns in TTS.
The present paper aims to expand the knowledge on typical ECG changes in patients with TTS and to test
the hypothesis that the pattern of ST-segment elevation has an impact on outcome in TTS.
Methods
Study populationThis study retrospectively investigated 136 patients who were hospitalized with TTS at the 3rd Medical Department of Cardiology and Intensive Care Medicine in the Wilhelminenhospital, Vienna, Austria from January 2006 until December 2017. Diagnosis of TTS was based on the criteria of the international expert consensus document on TTS: [1]
- Patients show transient left ventricular dysfunction (hypokinesia, akinesia, or dyskinesia) presenting as apical ballooning or midventricular, basal, or focal wall motion abnormalities. Right ventricular involvement can be Besides these regional wall motion patterns, transitions between all types can exist. The regional wall motion abnormality usually extends beyond a single epicardial vascular distribution; however, rare cases can exist where the regional wall motion abnormality is present in the subtended myocardial territory of a single coronary artery (focal TTS).
- An emotional, physical, or combined trigger can precede the takotsubo syndrome event, but this is not
- Neurologic disorders (e.g. subarachnoid haemorrhage, stroke/transient ischaemic attack, or seizures) as well as pheochromocytoma may serve as triggers for takotsubo
- New ECG abnormalities are present (ST- segment elevation, ST-segment depression, T- wave inversion, and QTc prolongation); however, rare cases exist without any ECG changes.
- Levels of cardiac biomarkers (troponin and creatine kinase) are moderately elevated in most cases; significant elevation of brain natriuretic peptide is
- Significant coronary artery disease is not a contradiction in takotsubo
- Patients have no evidence of infectious myocarditis.
- Postmenopausal women are predominantly affected.
Of the 136 patients in our TTS registry (2006-2017),
101 were included in the study. Thirty-two patients were excluded because of missing records of admission ECGs or confounding factors such as TTS-like presentation associated with myocarditis or hypertrophic cardiomyopathy. Furthermore, patients with pacemaker rhythm (n=2) and patients with known bundle branch block (n=1) were also excluded from further statistical analysis.
Electrocardiogram analysisTwelve-lead ECGs recorded at admission were assessed. The pathological changes, mainly of ST- segment, were investigated. The level of the preceding TP segment was identified as the isoelectric line and ST-segment elevation was defined as a shift from the J point in at least two contiguous leads of ≥ 0.25 mV in men < 40 years, ≥ 0.2 mV in men ≥ 40 years, or ≥ 0.15 mV in women in V2-V3 and/or ≥ 0.1 mV in the other leads. ST-segment depression was defined as a depression of ST-segment from the J point in at least two leads of ≥ 0.1 mV in the limb electrodes or ≥ 0.2 mV in precordial electrodes. T-wave inversion was defined as a symmetric negative T wave in at least two contiguous leads.
The patient’s ECGs were characterized and allocated into groups based on the time delay of onset-of-
Cardiol Cardiovasc Med 2019; 3 (6): 438-449 DOI: 1: 0.26502/fccm.92920094
symptoms to first ECG in two groups: 1. patients with ECG within the first 12 hours after the onset of symptoms (Group Aa) and 2. patients with ECG later than 12 hours after the onset of symptoms (Group Bb). The difference in ECG changes in acute and subacute settings was examined. Furthermore, ECG changes irrespective of time until the first ECG were investigated.
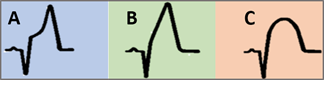
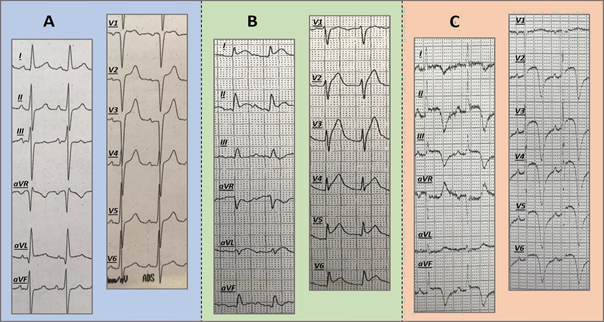
In a second step, patients were divided into three groups according to the pattern of ST-segment elevation in leads representing the anterior heart wall, mainly V2- V4, respectively: Group A (concave-type), group B (straight-type) and group C (convex-type) (Figure 3 and Figure 4). Only patients with a symptom onset of ≤ 12 hours were included in this statistical analysis.
The ECGs were evaluated by two investigators blinded to the patient`s data. If their verdict was in disagreement, a third observer established consensus.
Data collectionPatient’s data were gathered retrospectively from the electronic patient’s database, which holds the data about the patients treated in hospitals of The Vienna Hospital Association and from the local archive of the 3 medical Department of Cardiology and Intensive Care Medicine in Wilhelminenhospital, Vienna.
Medical history, cardiovascular risk factors, laboratory values at admission and complications during hospitalization were collected by reviewing the patient´s data records. In-hospital major adverse cardiovascular events (MACE) were defined as cardiac decompensation, cardiac arrhythmias, and cardiogenic shock during hospitalization for the index event. Complications, not directly linked to the cardiovascular system, were defined as non-cardiovascular complications.
Data monitoring was performed for implausible values and the initial prospective data collection was improved by control, and the addition of missing data for the individual patient. The mortality data were obtained from Statistics Austria, an independent and non-profit- making federal institution under the public law that supports scientific services. The Cause of death was reported using the International Statistical Classification of Disease and Related Health Problems (ICD-10). The data bank was designed and performed according to the Helsinki criteria after evaluation by the local ethics committee (EC Number: 12-255-0213).
Statistical analysisPatient’s characteristics, cardiovascular risk factors, laboratory values, in-hospital complications, and mortality were studied and compared based on the different ECG-characteristics. Parametric variables are presented as the mean ± standard deviation. Non- parametric variables are reported as median with interquartile range. ANOVA and Kruskal-Wallis test were used to evaluate differences in continuous variables, as appropriate. Differences between groups in categorical variables were analyzed using the chi-square test of homogeneity with multiple z-tests of two proportions or Fischer exact Test. Survival curves were generated with the Kaplan-Meier method and compared by use of the log-rank test. For all tests, a p-value of
<0.05 was considered to be statistically significant. All calculations were performed using the SPSS 25 statistical package for Windows (IBM Corp. Released 2017, IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp).
Results
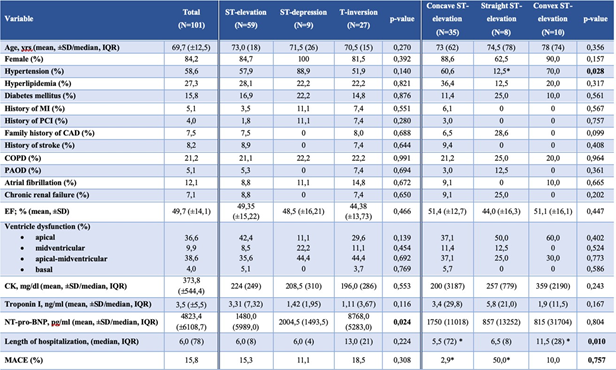
Baseline characteristicsAfter the exclusion of patients mentioned in the methods, a total of 101 TTS patients were included in the study. The mean age among all patients was
approximately 69.7 years (± 12.5) and 85% of patients were female (Table 1). This is in line with previously published data on TTS patients, which are typically postmenopausal women. Additionally, 5.1% of the study population had a previous history of myocardial infarction, 8.2% a history of stroke and COPD was present in 21.2% of cases. The mean value of Troponin I was 3.5 ng/ml and the mean value of NT-pro-BNP was 4823.4 pg/ml, respectively.
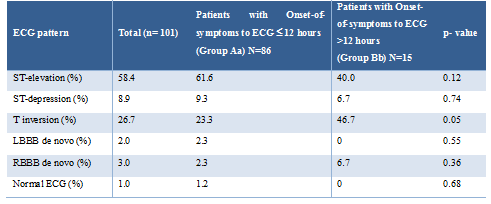
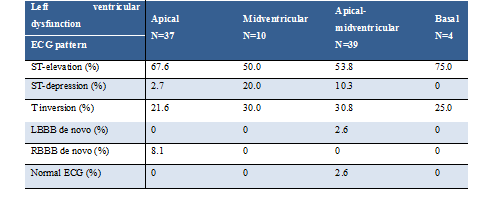
ECG changesECG-changes upon admission were stratified by the time delay of symptom-onset to the recording of the first in-hospital ECG (Table 2). While patients with an onset of symptoms less than 12 hours before admission- ECG (Group Aa), typically presented with ST-segment elevation (61.6% vs. 40.0% in Group Bb), the most common findings among patients with a symptom onset of more than 12 hours were T-wave inversions (46.7% vs. 23.3% in Group Aa). ST-segment depression was an uncommon finding in both acute (≤12 hours) and subacute presentation (>12 hours). Admission ECG changes were consistent among the different types of left ventricular dysfunction in TTS (apical, midventricular, apical-midventricular and basal ventricular dysfunction) with the most common finding being ST-segment elevation (Table 3).
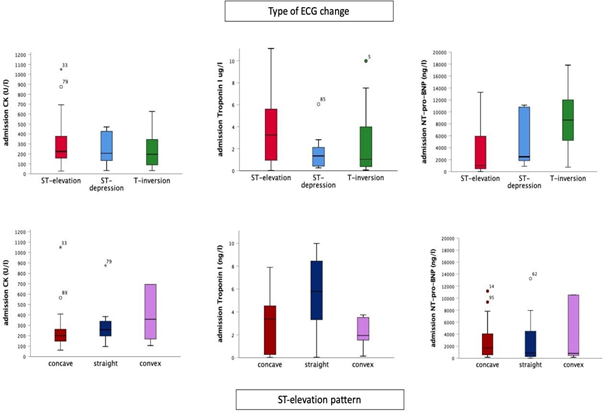
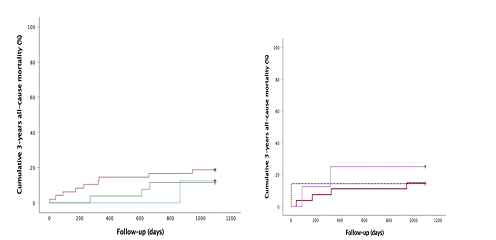
For the assessment of the impact of ECG changes on biomarkers and prognosis, we excluded patients with bundle branch block and normal ECG due to the low incidence. Biomarker analysis showed that patients with T-wave inversions had significantly higher levels of NT-pro-BNP (p=0.024). CK and troponin I values were largely comparable between the groups (Table 1 and Figure 1). Kaplan-Meier analysis did not show any statistically significant difference in three-year all-cause
mortality in patients with ST-elevation, ST-depression or T-inversion (χ2(2) = 0.839, p=0.657) (Figure 2a).
Analysis based on the ST-elevation patternIn a second step, we stratified patients into three groups according to the pattern of ST-segment elevation on admission. Concave ST-shape was present in 35 (66%), straight type in 8 (15%) and convex type in 10 (19%) patients, respectively. Baseline characteristics were largely comparable, except for a lower history of hypertension in the straight type ST-segment elevation group. Cardiac biomarkers, notably CK, high-sensitive cardiac troponin I (hs-CTnI) and NT-pro-BNP values at admission did not differ between groups (p= 0.243; p= 0.167; p= 0.804, respectively). Mean left ventricle ejection fraction (LVEF) at admission was 49.2% (±14.0) without significant difference between groups (p=0.447) (Table 1).
Patients with straight type ST-segment elevation had a significantly higher rate of MACE compared to patients with the concave type in univariate analysis (p= 0.002). However, no statistically significant difference in MACE rate was observed between patients with straight and convex ST-elevation shape (p= 0.118) as well as between concave and convex type (p= 0.399).
Moreover, univariate analysis revealed that patients with convex ST-elevation were hospitalized for a longer time than patients with concave ST-elevation (p= 0.010) but not longer than patients with straight ST-elevation (p= 0.142) (Table 1).
Kaplan-Meier analysis demonstrated no significant difference in three-year all-cause mortality between groups (χ2(2) = 0.501, p=0.778) (Figure 2b).
SD- standard deviation, MI- myocardial infarction, PCI- percutaneous coronary intervention, CAD- coronary artery disease, COPD – chronic obstructive pulmonary disease, PAOD- peripheral arterial occlusive disease, EF- ejection fraction, CK-creatinine kinase, NT-pro-BNP - N-terminal pro brain natriuretic peptide, TTS- Tako Tsubo syndrome
Cardiology and Cardiovascular Medicine Vol. 3 No. 6 – December 2019. [ISSN 2572-9292] 443
Table 3: ECG changes based on the pattern of left ventricular dysfunction LBBB- left bundle branch block, RBBB- right bundle branch block
- (a): Three-years all-cause mortality (Kaplan-Meier analysis) in groups with different repolarization
ST-elevation- red solid line, ST-depression- blue solid line, T-inversion- green solid line, respectively
- (b): Three-years all-cause mortality (Kaplan-Meier analysis) in groups with different ST-elevation
concave ST-elevation- burgundy solid line, straight ST-elevation- blue dotted line, convex ST-elevation- lila solid line, respectively
Discussion
This single-center retrospective study of ECG changes in patients with TTS showed that the most common change on admission ECG of patients who were admitted within the first 12 hours of symptom-onset is ST-elevation. Whereas, in patients who presented later than 12 hours after symptom-onset, the most common finding was T-wave inversion. This is in agreement with other studies, which showed an evolution of ST- elevation and ST-depression into T-wave inversion by 24 to 72 hours after onset of symptoms [8–10,15].
T-wave inversion was also associated with significantly higher levels of NT-pro-BNP. The level of NT-pro-BNP was four times higher than in patients with ST-elevation or ST-depression. There was no significant difference in levels of troponin I and CK between the groups. This may be linked to the time course of electrocardiographic changes in TTS as T-wave inversion on admission ECG suggests a more advanced stage of the disease. While high-sensitive troponin and CK levels tend to peak
within 24 hours after the onset of acute chest pain in patients with TTS, NT-pro-BNP levels keep rising beyond 24-48 hours [16]. The higher levels of NT-pro- BNP, as well as the tendency towards a lower ejection fraction in patients with T-wave inversion had no impact on long-term mortality or in-hospital complications, respectively. We also showed that the pattern of left ventricular dysfunction (apical, midventricular, apical-midventricular and basal type) cannot be predicted by repolarization abnormalities on admission ECG. ST-segment elevation was the most common ECG change in all types of ventricular dysfunction.
In this study, we further analyzed the ST-segment elevation pattern on admission ECG of TTS patients. The results revealed a significantly higher rate of in- hospital MACE, based on univariate analysis, and higher in-hospital mortality in patients with straight- type ST- elevation. Moreover, convex-type ST-
elevation was associated with an extended hospital stay.
Several studies have investigated the prognostic impact of various ECG changes in patients with TTS before [11,15,17,18]. The incidence of prolonged QT time in TTS and its impact on the risk of arrhythmias [17] or the impact of persistent ST-elevation on outcome in TTS patients have been well characterized [18]. This is the first study investigating the prognostic impact of different patterns of ST-segment elevation upon admission ECG.
The underlying pathology for the different shapes of ST-elevation in patients with TTS is not apparent. In STEMI, it has been discussed that the form of ST- elevation changes might be due to ischemia by modification of transmembrane potential, lower amplitude and shorter duration of an action potential, and delayed activation [19,20]. Hence, the shape of ST- elevation could correlate with the severity of the myocardial injury. Studies including patients with anterior STEMI demonstrated higher levels of cardiac biomarkers, worse left ventricular function, higher incidence of severe complications and higher mortality in patients with straight and convex type ST-segment elevation as analyzed by univariate and multivariate regression analysis [12–14]. ST-elevations in ACS patients result from the ischemia triggered by the prolonged occlusion of a major epicardial coronary artery. However, ischemia in TTS patients might among other reasons be the result of short-term vasospasm, microcirculatory impairment or vasoconstriction of coronary arteries due to increased catecholamine levels [18,21]. Although TTS itself and the ischemia in TTS is caused by a different trigger than the ACS, our results seem to correspond with the findings of studies investigating different ST-elevation pattern in ACS patients.
Based on the studies, which have shown that mortality and morbidity rates in TTS are comparable to those of
ACS [22], the recently published international expert consensus paper by the European Society of Cardiology (ESC) stresses the relevance of TTS as a serious condition. Therefore, adequate early management, including both diagnostic, monitoring and therapeutic procedures of patients with TTS is critical in reducing the rate of complications and in-hospital mortality [23].
Although the study population was relatively small, this analysis indicates an association of non-concave ST- shape elevation with worse outcomes. Furthermore, the presence of T-wave inversion at the time of admission was correlated with significantly higher levels of NT- pro-BNP.
Limitations and strengths
Potential limitations of this investigation include the single-center nature of our study, the retrospective design of our research, as well as the relatively small study population, which is not tiny in comparison to other studies in TTS patients. The relatively small study population, however, prohibited the performance of several statistical analyses. Accordingly, this study is mainly hypothesis-generating.
Strengths of our study are the consecutive inclusion of TTS patients, the long median follow-up, and the well- managed database for baseline characteristics and clinical endpoints including cardiovascular and non- cardiovascular complications and in-hospital as well as long-term all-cause mortality for all TTS patients.
Conclusion
The present study confirms the typical findings of previous ECG studies in TTS including ST-elevation or T-wave inversion depending on the timing of admission. The present study also indicates that the pattern of ST- segment elevation, as well described for acute STEMI
patients, especially the straight-type ST elevation, might
also be used for risk stratification in TTS patients. As this study has a pilot phase character, additional studies with larger sample sizes are needed to validate the findings of our study.
References
- Ghadri JR, Wittstein IS, Prasad A, Sharkey S, Dote K, et al. International Expert Consensus Document on Takotsubo Syndrome (Part I): Clinical Characteristics, Diagnostic Criteria, and Eur Heart J 39 (2018): 2032–2046.
- Lyon AR, Bossone E, Schneider B, Sechtem U, Citro R, et al. Current state of knowledge on Takotsubo syndrome: a Position Statement from the Taskforce on Takotsubo Syndrome of the Heart Failure Association of the European Society of Cardiology. European Journal of Heart Failure 18 (2016): 8–27.
- Akashi YJ, Nef HM, Lyon AR. Epidemiology and pathophysiology of Takotsubo syndrome. Nature Reviews Cardiology 12 (2015): 387– 397.
- Previtali M, Repetto A, Panigada S, Camporotondo R, Tavazzi Left ventricular apical ballooning syndrome: prevalence, clinical characteristics and pathogenetic mechanisms in a European population. International Journal of Cardiology 134 (2009): 91–96.
- Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, et al. Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. The New England Journal of Medicine 373 (2015): 929–938.
- Mahmoud AN, Al-Ani M, Saad M, Elgendy AY, Elgendy IY. Development and validation of a simple integer risk score for prediction of in-hospital mortality following Takotsubo syndrome. Heart & Lung: The Journal of Critical Care 45 (2016): 510–514.
- Parodi G, Scudiero F, Citro R, Silverio A, Bellandi B, et al. Risk Stratification Using the CHA2DS2-VASc Score in Takotsubo Syndrome: Data From the Takotsubo Italian Network. Journal of the American Heart Association 6 (2017): 2017.
- Bennett J, Ferdinande B, Kayaert P, Wiyono S, Goetschalkx K, Dubois C, Sinnaeve P, Adriaenssens T, Coosemans M, Desmet W. Time course of electrocardiographic changes in transient left ventricular ballooning syndrome. International Journal of Cardiology 169 (2013): 276–280.
- Guerra F, Rrapaj E, Pongetti G, Fabbrizioli A, Pelizzoni V, Giannini I, Aschieri D, Costantini C, Capucci A. Differences and Similarities of Repolarization Patterns During Hospitalization for Takotsubo Cardiomyopathy and Acute Coronary Syndrome
- Frangieh AH, Obeid S, Ghadri J, Imori Y, D’Ascenzo F, et al. ECG Criteria to Differentiate Between Takotsubo (Stress) Cardiomyopathy and Myocardial Infarction. J Am Heart Assoc 5 2016):
- Weihs V, Szücs D, Fellner B, Eber B, Weihs W, et al. Electrocardiogram changes and wall motion abnormalities in the acute phase of Tako-Tsubo syndrome. European Heart Journal: Acute Cardiovascular Care 5 (2016): 481–488.
- Kosuge M, Kimura K, Ishikawa T, Kuji N, Tochikubo O, Sugiyama M, Ishii M. Value of ST-segment elevation pattern in predicting infarct size and left ventricular function at discharge in patients with reperfused acute anterior myocardial infarction. American heart journal 137 (1999): 522–527.
- Gao YQ, Li ZL, Ding MX, Wu HC, Li GX. [Relation of the ST-segment elevation pattern in acute phase of anterior wall acute myocardial infarction to short-term prognosis]. Di 1 jun yi da xue xue bao = Academic journal of the first medical college of PLA 22 (2002): 156–158.
- Karadede A, Aydinalp O, Temamogullari AV, Toprak N. The relationship of ST segment elevation shape with preserved myocardium and signal-averaged electrocardiography in acute anterior myocardial infarction. Heart and vessels 16 (2012): 146–153.
- Looi JL, Wong CW, Lee M, Khan A, Webster M, Kerr AJ. Usefulness of ECG to differentiate Takotsubo cardiomyopathy from acute coronary syndrome. International Journal of Cardiology 199 (2015): 132–140.
- Fröhlich GM, Schoch B, Schmid F, Keller P, Sudano I, et al. Takotsubo cardiomyopathy has a unique cardiac biomarker profile: NT- proBNP/myoglobin and NT-proBNP/troponin T ratios for the differential diagnosis of acute coronary syndromes and stress induced cardiomyopathy. Int J Cardiol 154 (2012): 328–332.
- Santoro F, Brunetti ND, Tarantino N, Romero J, Guastafierro F, Ferraretti A, Di LFM, Riccardo M, Luigi P, Matteo P, Biase D, Di L. Dynamic changes of QTc interval and prognostic significance in takotsubo (stress) cardiomyopathy 2017: 1116–1122.
- Santoro F, Stiermaier T, Tarantino N, Guastafierro F, Graf T, et al. Impact of persistent ST elevation on outcome in patients with Takotsubo syndrome. Results from the GErman Italian STress Cardiomyopathy (GEIST) registry. International Journal of Cardiology 255 (2018):140–144.
- Martínez Á, Llâcer Á. Segment Elevation. Epidemiology and Community Health 47 (2005): 486–490.
- Downar E, Janse MJ, Durrer D. The effect of acute coronary artery occlusion on subepicardial transmembrane potentials in the intact porcine heart. Circulation 56 (1977): 217–224.
- Kato K, Lyon AR, Ghadri JR, Templin C. Takotsubo syndrome: Aetiology, presentation and treatment. Heart 103 (2017): 1461–1469.
- Redfors B, Vedad R, Angerås O, Råmunddal T, Petursson P, et al. Mortality in takotsubo syndrome is similar to mortality in myocardial infarction - A report from the SWEDEHEART International journal of cardiology 185 (2015): 282–289.
- Ghadri JR, Wittstein IS, Prasad A, Sharkey S, Dote K, et al. International Expert Consensus Document on Takotsubo Syndrome (Part II): Diagnostic Workup, Outcome and Management. European Heart Journal 2018: 1– 16.


 Impact Factor: * 3.5
Impact Factor: * 3.5 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 14.80%
Acceptance Rate: 14.80%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 