Recurrent Acute Pericarditis Triggered by COVID-19 Disease
Article Information
Maham Akbar Waheed1*, Geurys Rojas-Marte2,3
1Department of Medicine, Maimonides Medical Center, Brooklyn, New York, USA
2Department of Cardiology, Maimonides Medical Center, Brooklyn, New York, USA
3Donald and Barbara Zucker School of Medicine at Hosftra/Northwell, Staten Island, NY, USA
*Corresponding Author: Maham Akbar Waheed, MD, Department of Medicine, Maimonides Medical Center, 4802 10th Ave, Brooklyn, New York, USA
Received: 22 February 2021; Accepted: 05 March 2021; Published: 22 March 2021
Citation: Maham Akbar Waheed, Geurys Rojas-Marte. Recurrent Acute Pericarditis Triggered by COVID-19 Disease. Cardiology and Cardiovascular Medicine 5 (2021): 218-223.
View / Download Pdf Share at FacebookAbstract
A 37-year-old woman presented with persistent chest pain and shortness of breath since four weeks prior to admission. Outpatient ECG was suggestive of acute pericarditis, however her symptoms persisted despite treatment with colchicine and NSAIDs. Serology revealed presence of COVID IgG antibodies. We discuss the case of late presenting, recurrent acute pericarditis in the context of COVID disease.
Keywords
COVID-19; Pericarditis; Pericardial effusion; Colchicine
COVID-19 articles; Pericarditis articles; Pericardial effusion articles; Colchicine articles
Article Details
Abbreviations:
COVID-19: Coronavirus disease 2019; TTE: Transthoracic echocardiography; CMR: Cardiac magnetic resonance imaging; CTA: Computed tomography angiogram; LGE: Late gadolinium enhancement; ECMO: Extra-corporal membrane oxygenation
1. Learning Objectives
- To explore the cardiovascular manifestations of covid-19 and to identify late onset covid-19 related pericardial disease.
- To use multimodality imaging strategies for improving diagnostic accuracy and identification of cardiac disease.
- The role of colchicine and steroid therapy in patients affected with covid-19 related pericarditis.
2. Clinical Case
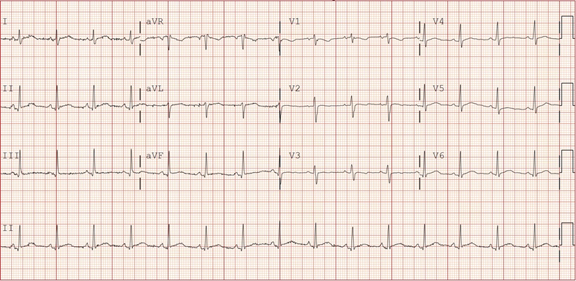
A 37-year-old woman presented to the emergency department (ED) with complaint of intermittent, left sided, sub-sternal chest pain. The pain started four weeks earlier and was initially associated with cough and shortness of breath. No fever or sick contacts were reported. After three weeks of no significant improvement with ibuprofen, she presented to her cardiologist’s office where an electrocardiogram (ECG) showed ST-segment elevation in leads I, II, and V4-V6 with diffuse non-specific T wave changes (Figure 1). The patient was prescribed colchicine for possible pericarditis. As the pain persisted, she decided to go to the ED.
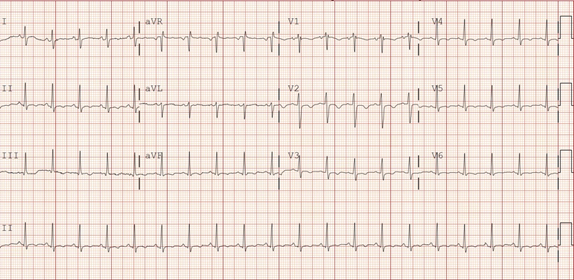
On presentation to the ED, the patient was afebrile, blood pressure was 114/68 mmHg, heart rate 128 beats/min, respiratory rate 39 beats/minute and oxygen saturation was 100 percent on room air. Lung examination was significant for decreased air entry on the bases bilaterally. Cardiovascular examination was significant for tachycardia and a pericardial friction rub; no murmurs, jugular venous distention or pedal edema were noted. Pulses were 2+ in all four extremities. Past medical history was significant for two episodes of acute pericarditis in 2016 (four months apart). During both episodes, the patient’s only complaint was chest pain of mild intensity, which resolved within a week with NSAIDs and colchicine. An ECG showed sinus tachycardia at 125 beats per minute and diffuse T wave inversions (Figure 2).
Laboratory work revealed white blood cell count of 22.9 K/UL, lactate dehydrogenase (LDH) 225 IU/L, erythrocyte sedimentation rate (ESR) 95, D-dimer 783 ng/mL, Ferritin 375.2 ng/ml, C- reactive protein(CRP) 38.041mg/dl, creatine phosphokinase (CPK) 18 IU/L, troponin 0.01, creatine kinase-MB (CK-MB) 0.5 ng/ml, brain natriuretic peptide (BNP) 250 pg/ml. Nasopharyngeal swab for COVID-19 (rRT-PCR) was negative but serum COVID IgG was reactive. Autoimmune workup with serum anti-nuclear antibody (ANA), anti-neutrophilic cytoplasmic antibodies (ANCA), rheumatoid factor (RF), anti-double stranded DNA (anti-dsDNA) was negative. Quantiferon gold testing was negative.
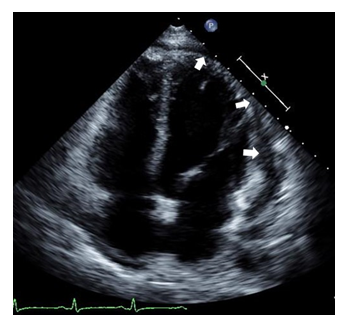
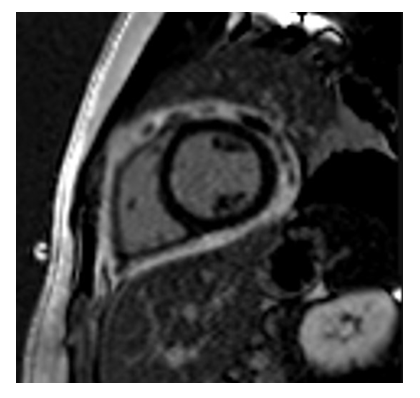
Transthoracic echocardiography (TTE) revealed left ventricular ejection fraction of 50-55 percent and small to moderate pericardial effusion (Video 1 and Figure 3). A computed tomography angiogram (CTA) evidenced small to moderate pericardial effusion and small bilateral pleural effusions; there was no evidence of acute pulmonary embolism. Cardiac magnetic resonance imaging (CMR) showed small pericardial effusion with foci of late gadolinium enhancement (LGE) in pericardium suggestive of pericarditis (Figure 4). Septal wall motion abnormality was also seen.
The patient was admitted to the hospital for symptomatic management. She was treated with ibuprofen and colchicine with improvement of her symptoms within 5 days. A repeat TTE did not show any enlargement of the pericardial effusion. Patient was discharged on oral prednisone. Follow up call a month later revealed that the symptoms had gradually resolved.
3. Discussion
Herein we present a case of recurrent acute pericarditis triggered by COVID-19. The disease caused by SARS-CoV-2 virus can result in severe cardiac complications including myocardial infarction, stress-induced cardiomyopathy, non-ischemic cardiomyopathy, coronary vasospasm as well as myocarditis simulating STEMI [1]. Decompensated heart failure as well as cardiogenic shock requiring urgent treatment, including mechanical circulatory support with ECMO have also been reported [2].
Myopericarditis and acute pericardial involvement causing acute pericarditis, pericardial effusion or cardiac tamponade have been found to occur during the acute phase of COVID-19 disease [2, 3]. Serum troponin levels are found to be elevated in 35-50% of such patients. This is thought to be secondary to epicardial inflammation [4]. The exact mechanisms by which COVID-19 attacks the cardiovascular system remain unknown. It has been proposed that the interaction between the viral spike (S protein) protein and angiotensin-converting enzyme 2 triggers the entry of viral particles into host cells resulting in many of the cardiovascular manifestations of COVID-19 [5].
Most patients affected with pericarditis present with worsening chest pain and difficulty breathing [4]. COVID-19 related pericarditis usually presents in a similar fashion [6, 7] and can have hemodynamic compromise, leading to cardiac tamponade [3]. In the case we describe, although the patient reported SOB and chest pain, which persisted for several weeks, she remained hemodynamically stable. Serum troponin levels were negative which ruled out the possibility of myocardial involvement. This was confirmed by CMR.
A German study consisting of 100 patients recently recovered from COVID-19, demonstrated cardiac involvement in 78% of cases. This was independent of pre-existing conditions, severity of acute illness or time from initial diagnosis [8]. LGE was found in 32% of patients, while pericardial enhancement was found in 22% with pericardial effusion in 20% of patients. This highlights the persistence of ongoing cardiac inflammation in patients post recovery from COVID-19 [8]. Analysis of aspirated pericardial fluid sampled from patients with COVID-19 related pericardial effusion has been negative for SARS-CoV-2 [6]. In contrast, one Italian study did detect the presence of SARS-COV-2 RNA within the pericardial fluid of a patient with COVID-19 related cardiac tamponade [7]. However, only one of the three genes was positive, suggesting low viral load.
Lastly, the different ECG stages of pericarditis can be observed in our patient. The first ECG was consistent with a transition from stage I (ST segment elevation and PR segment depression) to II and her second ECG (presentation to the hospital) is consistent with stage III (widespread T wave inversion).
So far, no guidelines have been established for the treatment of COVID-19 related pericarditis. Many studies [9] have proposed the use of corticosteroids to decrease the inflammation associated with the cytokine storm seen in patients with COVID-19. Colchicine is well known therapeutic agent used in patients with acute pericarditis [10] and shows promising results in treating patients with COVID-19 related pericarditis.
4. Limitations
Given the history of two prior episodes of acute pericarditis, idiopathic recurrent acute pericarditis (IRAP) could be considered as an alternative explanation for our patient’s symptoms. However, our patient’s presentation was completely different this time. She presented during the peak of the pandemic. Her pain lasted for almost 4 weeks and was associated with cough and shortness of breath. She reported her symptoms to be of severe intensity as compared to her prior mild episodes. Having cough and SOB at the begininig of her symptoms prior to presentation as well as positive serology for IgG antibodies against SARS-Cov-2 and inflammatory markers elevation to the degree of COVID-19 patients with severe disease was highly suggestive of her recent exposure to the disease.
5. Conclusion
The myriad of complications that COVID-19 brings with it are complex. Our case highlights the importance of recognizing late-presenting pericarditis and pericardial effusion in patients with active or recent history of COVID-19 disease and negative viral and autoimmune workup. CMR can be a great diagnostic tool in these cases. It is important to note that our patient had bare minimum improvement of her symptoms on oral NSAIDs; however the addition of colchicine and oral prednisone brought about a great therapeutic effect
Conflict of Interest
The authors declare no conflict of interest.
References
- Mahmud E, Dauerman HL, Welt FG, et al. Management of acute myocardial infarction during the COVID-19 pandemic. Catheter Cardiovasc Interv 96 (2020): 336-345.
- Fried JA, Ramasubbu K, Bhatt R, et al. The variety of cardiovascular presentations of COVID-19. Circulation 141 (2020): 1930-1936.
- Dabbagh MF, Aurora L, D’Souza P, et al. Cardiac tamponade secondary to COVID-19. JACC Case Rep 2 (2020): 1326-1330.
- Lange RA, Hillis LD. Acute pericarditis. N Engl J Med 351 (2004): 2195-2202.
- Nishiga M, Wang DW, Han Y, et al. COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives. Nat Rev Cardiol 17 (2020): 543-558.
- Fox K, Prokup JA, Butson K, et al. Acute Effusive Pericarditis: A Late Complication of COVID-19. Cureus 12 (2020): e9074.
- Farina A, Uccello G, Spreafico M, et al. SARS-CoV-2 detection in the pericardial fluid of a patient with cardiac tamponade. Eur J Intern Med 76 (2020): 100-101.
- Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol 5 (2020): 1265-1273.
- Atri D, Siddiqi HK, Lang J, et al. COVID-19 for the cardiologist: a current review of the virology, clinical epidemiology, cardiac and other clinical manifestations and potential therapeutic strategies. JACC Basic Transl Sci 5 (2020): 518-536.
- Imazio M, Brucato A, Cemin R, et al. A randomized trial of colchicine for acute pericarditis. N Engl J M 369 (2013): 1522-1528.


 Impact Factor: * 3.5
Impact Factor: * 3.5 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 14.80%
Acceptance Rate: 14.80%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 