Indexing of Left Atrial Volume by Body Surface Area and Height in a Brazilian Population without Previous Heart Disease and with a Normal Heart on Echocardiography. Behavior in Obese and Overweight Patients
Article Information
Edmundo J. Nassri Camara1,2, Flávia R. do Prado Valladares2, Ng Kin Key2, Paloma Fonseca Santana2, Jun Ramos Kawaoka2, Thais Harada Campos2, Marcus Ribeiro de O. Santana2, Alex Costa Cunha2, Danilo Sousa Sampaio2, Gustavo Pinheiro Santana2, Luis Gustavo S. Brito2, Narjara de O. Cardoso Dourado2, Saulo Jende Nascimento2, Alice Povoa A. L. Lira2, Naily N. do Nascimento2, Romeu Pacheco F. dos Santos2, Sérgio Rodrigo F. Rocha2, Thaise Gordiano Machado2
1Federal University of Bahia, Brazil
2Hospital Ana Nery, Salvador – Bahia, Brasil
*Corresponding author: Edmundo J Nassri Camara, Federal University of Bahia, Brazil.
Received: 13 January 2023; Accepted: 20 January 2023; Published: 29 January 2023
Citation:
Edmundo J. Nassri Camara, Flávia R. do Prado Valladares, Ng Kin Key, Paloma Fonseca Santana, Jun Ramos Kawaoka, Thais Harada Campos, Marcus Ribeiro de O. Santana, Alex Costa Cunha, Danilo Sousa Sampaio, Gustavo Pinheiro Santana, Luis Gustavo S. Brito, Narjara de O. Cardoso Dourado, Saulo Jende Nascimento, Alice Povoa A. L. Lira, Naily N. do Nascimento, Romeu Pacheco F. dos Santos, Sérgio Rodrigo F. Rocha, Thaise Gordiano Machado. Indexing of Left Atrial Volume by Body Surface Area and Height in a Brazilian Population without Previous Heart Disease and with a Normal Heart on Echocardiography. Behavior in Obese and Overweight Patients. Cardiology and Cardiovascular Medicine 7 (2023): 25-31.
View / Download Pdf Share at FacebookAbstract
Background: Left atrial (LA) volume indexing for body surface area (BSA) may underestimate LA size in obese and overweight people. Since LA volume is a risk marker for some cardiovascular events, it is suggested that indexing for height would be an alternative more appropriate method. The aims of this study were to find normal and the best cutoff values for LA volume indexed for height in our population.
Methods: Echocardiograms from 2018 to 2021 were reviewed and patients without known cardiac disease and completely normal echocardiograms that had the left atrial volume (LAvol) measured by biplane Simpson’s method were included. LAvol was indexed by BSA (ml/m²), by height (LAvol/m), by height raised to exponent 2.7 (ml/ m2.7) and by height squared (ml/h²).
Results: A total of 545 patients, 50.5 ± 13.4 y., 335 females (61,5%) were analyzed. There were 145 normal weight (26.6%), 215 overweight (39.4%), 154 obese (28.3%) and 31 low weight (5.7%) patients. To establish normal values we included only the normal weight group and considered normal values from 2SD below to 2SD above the mean. Mean and normal values were: LAvol/h 26.0 ±4.5, 17 – 35 ml/m, LAvol/ht² 16 ± 2.8, 10.4 - 21.6 ml/ ht² and LAvol/ht2.7 11.4 ± 2.2, 7.0 - 15.8 ml/m2.7. The normal LAvol/ht2.7 differed between male and female (11.4 ± 2.4 and 12.8 ± 2.6, p < 0.001). LA diameter, LAvol, LAvol/h, LAvol/h² and LAvol/ht2.7 increased progressively from low-weight, normal weight, overweight and obese patients (p<0.0001), but not LAvol/BSA. When indexing LAvol for height, for height² and for height2.7 20.8%, 22.7% and 21.4% of the obese patients, respectively, were reclassified as enlarged LA, and 7.4%, 8.8% and 8.4% of the overweight patients as well. Using ROC curve ana
Keywords
Cardiac Disease; Echocardiograms; Increased Left Atrial
Cardiac Disease articles; Echocardiograms articles; Increased Left Atrial articles
Article Details
1. Introduction
Increased left atrial (LA) volume is a risk marker for atrial fibrillation, stroke, and heart failure, and it has been correlated with increased cardiovascular mortality [1–7]. International guidelines and clinical practice recommend that LA volume be indexed to body surface (B.S.A.) [8,9]. However, in obese individuals there is a tendency to underestimate these values, often placing individuals with an enlarged left atrium as normal, after indexing by a high B.S.A.. This is an important problem, because obesity is associated with atrial fibrillation [10] and it appears to be mediated by left atrial dilatation [11]. The prevalence of obesity is increasing, it is likely that prevalence of obesity- related AF will increase as well. B.S.A. is an isometric measure, which assumes that LA size has a linear relationship to body size. However, organ size (i.e., heart size) and body size do not grow proportionally; in other words, their relationship is nonlinear [12]. Many parameters can be indexed for height, especially in obese individuals. Alternative forms of scaling, including allometric size variable such as height raised to an exponent, may help address this issue [12,13]. The normal values and how the left atrial volume indexed for height behaves in obese and overweight individuals under normal conditions of cardiovascular health is not well explained in the literature, especially in a Brazilian population. The current work aims to clarify these questions.
2. Methods
This is a pilot, observational, descriptive, retrospective study. Echocardiographic data, age, sex, weight, height and body surface were obtained from the data file of the echocardiography service of Hospital Ana Nery, from 2018-2021. Patients with normal echocardiograms, in sinus rhythm, with no history or evident cardiovascular disease (mild systemic arterial hypertension and non-insulin dependent diabetes without target organs involvement), were included independent of any other factor. In all patients, in addition to LA volume, LA and LV dimensions, wall thickness, left ventricular mass, LV ejection fraction, and aortic root diameter were also recorded. Left atrial volumes were obtained by the Simpson’s biplane method of disks using apical four chamber and two chamber views at ventricular end-systole. The data of each patient were reviewed to verify there was no missing data and to be sure that the exam was normal, with special attention to LV diastolic dysfunction parameters, such as the E' waves of the medial and lateral mitral annulus. Exclusion criteria: any parameter of abnormality such as LA maximum diameter at the parasternal long axis > 40mm, indexed LA volume > 34ml/m², left ventricular wall relative thickness > 0.42, increased left ventricular indexed mass, ejection fraction less than 55%, any change suggesting LV diastolic dysfunction such as reduced medial (< 7cm/s) or lateral (<10cm/s) and mitral regurgitation more than minimal. A total of 645 charts reported as normal echocardiograms were reviewed, and 545 patients were included in the study. The protocol of the study was approved by the Research Ethics Committee of the Hospital Ana Nery (HAN/SESAB), Salvador-BA, which waived the need to obtain written informed consent.
The LA volume were than indexed for B.S.A., height, height² and height2.7 in four groups of patients:
- Group I, low weight (B.M.I. < 20 kg/m²)
- Group II, normal weight (B.M.I. ≥ 20 kg/m² and < 25 kg/m²),
- Group III, overweight (B.M.I. ≥ 25 kg/m² and < 30 kg/m²),
- Group IV, obese (B.M.I. ≥ 30 kg/m²).
3. Data Analysis
Quantitative data are described as mean ± standard deviation and IC 95%. Categorical data are described as an absolute number and percentage. The means, standard deviations (SD) and 95% confidence intervals (CI) of the quantitative variables were obtained for the total of patients and for the subgroups. To comparisons, we considered normal indexed left atrial volume for height, height² and height2.7 the interval from 2 SD below and 2 SD above the mean of the normal weight group (B.M.I. ≥ 20 kg/m² and < 25 kg/m²). Student's t test was used to compare means between two independent groups, and the ANOVA test of variance for comparisons between the three groups according to B.M.I. (normal, overweight, and obese) with the Bonferroni test for post hoc analysis between pairs of groups. The chi-square test was used to compare categorical variables. Receiver operating characteristic (ROC) curve analysis was used to identify the indexation method that best predicted increased LA. Statistical analysis were performed with IBM SPSS statistics version 21. Statistical significance was considered as P < 0.05 two-tailed.
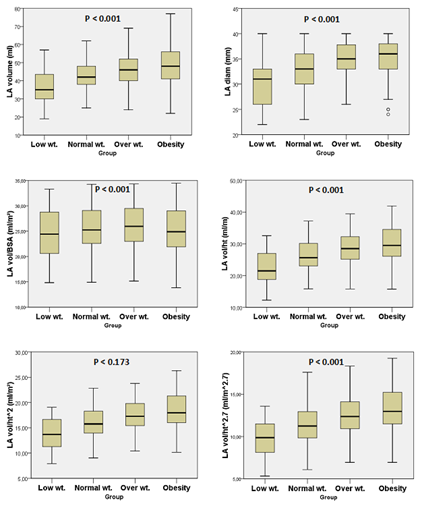
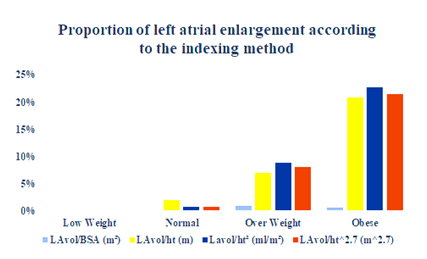
4. Results
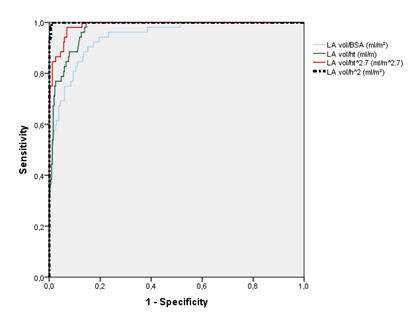
A total of 545 patients, mean age 50.5 ± 13.4 y., 335 females (61,5%) and 210 males (38.5%) were analyzed. The anthropometric measurements are detailed in table I. There were 145 normal weight (26.6%), 215 overweight (39.4%), 154 obese (28.3%) and 31 low weight (5.7%) patients. Obesity was more commonly seem in females (75%) just as there was a trend towards more overweight in women (59%). The LA diameter and volume progressively increased from low-weight (Low-wt), normal, overweight (Over-wt) and obese groups (table II and figure 1). When indexed by BSA the LA volume did not differ between groups. Otherwise, when indexing by height, height2 and height2.7, we observed a progressive and statistically significant increase in the volume of the left atrium (figure 1). The normal values of LA volume according to height, height2.7 and height² (allometric measurements) were obtained by the mean ± 2 standart deviations (SD) in the normal weight group. For height the normal values varied from 17.0 to 35.0 ml/m (mean ± SD 26.0 ±4.5). For height² the normal values of LA volume varied from 10.4 to 21.6 (mean ± SD 16.0 ± 2.8). For height2.7 the normal values varied from 7.0 to 15.8 ml/m2.7 (mean ± SD 11.4 ± 2.2). The normal LA volume for height2.7 differed between male and female (11.4 ± 2.4 and 12.8 ± 2.6, p < 0.001). Table III describes the normal values and the maximum limit of normality for indexing the left atrium by height, height² and height2.7. Sixteen of 215 (7.4%) of overweight patients and 32 of 154 (20.8%) obese patients were reclassified from normal to dilated left atrium when indexed by height, 19 of 215 (8.8%) and 35 of 154 (22.7%), respectively, when indexed by height2, and 18 of 215 (8.4%) and 33 of 154 (21.4%), respectively, when indexed by height2.7 according to gender (figure 2). In the normal weight group, only one patient was reclassified as enlarged LA when indexed by height2 or by height2.7 and 3 patients were reclassified when indexed by height. No low-weight patients were reclassified as enlarged LA when indexed by height, using any one of the three methods. The results of ROC analyses for the best cutoff values to identify LA enlargement in obese or overweight patients are shown in Figure 3 and Table IV. LA was considered enlarged if at least two of the three indexation methods by height were above normal values. LA volume indexation by height² had the highest area under curve (AUC 1.0, 95% CI 0.999-1.0) followed by LAvol/ht2.7 (AUC 0.989, 95% CI 0.98-0.997), LAvol/h (AUC 0.972, 95% CI 0.957-0.987) and LAvol/BSA (AUC 0.943, 95% CI 0.914-0.973). Operational cutoff values with corresponding predictive characteristics for obese or overweight patients are presented in Table IV. Interestingly, we found 29.2 ml/m² the best cutoff value if we use LAvol/BSA to the diagnosis of LA enlargement in obese or overweight patients.
|
Total |
Low-wt |
Normal |
Over-wt |
Obese |
||||
|
Min |
Max |
P |
||||||
|
Age |
50.5 13.4) |
17 |
83 |
45.4 17.5) |
51.6 (14.4) |
51.1 12.7) |
49.8 12.2) |
0.096 |
|
Weight (Kg) |
73.4 (15.7) |
27 |
139 |
49 (8.2) |
62 (7.7) |
73.4 (8.8) |
89.1 14.3) |
<0.001 |
|
Height (cm) |
163.1 (9.4) |
135 |
192 |
164.5 (9.1) |
163.5 (9.2) |
163.6 9.6) |
161.8 9.3) |
0.214 |
|
B.S.A. (m²) |
1.79 (0.21) |
1.1 |
2.5 |
1.52 0.17) |
1.67 (0.15) |
1.80 (0.16) |
1.93 0.19) |
<0.001 |
|
m2.7 |
3.78 (0.59) |
2.25 |
5.82 |
3.9 (0.57) |
3.8 (0.59) |
3.8 (0.61) |
3.7 (0.57) |
0.224 |
|
m² |
2.67 (0.31) |
1.82 |
3.69 |
2.71 0.30) |
2.68 (0.31) |
2.68 (0.32) |
2.63 (0.30) |
0.220 |
|
B.M.I. Kg/m²) |
27.6 (5.3) |
11.2 |
53.4 |
18.0 (1.8) |
23.1 (1.3) |
27.4 (1.3) |
33.95 3.9) |
<0.001 |
Table I: Anthropometric data on the total number of patients and in the normal weight, underweight, overweight, and obese groups.
|
Total |
Low-wt |
Normal |
Over-wt |
Obese |
P |
|
|
LA diam (mm) |
34.2 (3.7) |
30.4 (4.8)* |
33.0 (3.6) |
34.9 (3.2)* |
35.3 (3.3)* |
<0.001 |
|
LAvol (ml) |
45.5 (9.3) |
37.4 (9.6)a |
42.6 (7.9) |
46.6 (8.6)* |
48.3 (9.8)* |
<0.001 |
|
LAvol/B.S.A. |
25.5 (4.5) |
24.6 (5.2) |
25.6 (4.3) |
26.0 (4.4) |
25.1 (4.8) |
0.173 |
|
LAvol/ht |
27.9 (5.4) |
22.7 (5.3)* |
26.0 (4.5) |
28.5 (4.8)* |
29.9 (5.7)*x |
<0.001 |
|
LAvol/ht2.7 |
12.2 (2.6) |
9.8 (2.2)* |
11.4 (2.2) |
12.4 (2.3)* |
13.3 (2.8)*+ |
<0.001 |
|
LAvol/ht² |
17.1 (3.4) |
13.8 (3.1)* |
16.0 (2.8) |
17.4 (3.0)* |
18.5 (3.6)*+ |
<0.001 |
Table II: Left atrium sizing and indexing by body surface area between normal weight, low weight, overweight and obese patients.
* P<0.01 comparing to normal weight; a P<0.02 versus normal weight; + P<0.01 obese versus overweight; x P=0.055 obese versus overweight
|
Normal |
Maximum normal |
|
|
LAvol/B.S.A. |
25.6 ± 4.3 |
34.2 |
|
LAvol/ht (ml/m) |
26.0 ±4.5 |
35.0 |
|
LAvol/ht² (ml/ m²) |
16 ± 2.8 |
21.6 |
|
LAvol/ht2.7 (ml/ m2.7) male female |
11.4 ± 2.2 11.4 ± 2.4 12.8 ± 2.6 |
15.8 16.2 18.0 |
Table III: Normal values and the maximum normal for left atrium indexing by height, height² and height2.7.
|
Variables |
Optimal cutoff value |
||||
|
AUC |
95% CI |
Sensitivity |
Specificity |
||
|
LAvol/BSA (ml/m²) |
,943 |
0.914-0.973 |
29.2 |
90.40% |
84.90% |
|
LAvol/ht (ml/m) |
,972 |
0.957-0.987 |
34.4 |
84.60% |
93.40% |
|
LAvol/ht^2.7 (ml/m2.7) |
,989 |
0.980-0.997 |
15 |
98.10% |
93.10% |
|
LAvol/ht^2 (ml/ht2) |
1,000 |
0.999-1.000 |
21.5 |
100% |
99.10% |
Table IV: Results of ROC analyses to identify LA enlargement* in obese or overweight patients.
*LA enlargement was defined if at least two of the three indexation methods by height were above normal values.
Figure 3: Receiver operating characteristic (ROC) curve analysis for prediction of enlarged LA in obese or overweight patients. Enlarged LA was defined as at least two abnormal of the three methods of volume indexation by height. BSA, body surface area; ht, height; m^2.7, meters raised to exponent 2.7; m^2, meters squared.
|
N |
Normal |
Maximum normal |
P |
|
|
LAvol/B.S.A. male female |
69 76 |
25.6 ± 4.3 25.4 ± 4.4 25.7 ± 4.3 |
34.2 34.2 34.3 |
0.73 |
|
LAvol/ht (ml/m) male female |
69 76 |
26.0 ±4.5 26.4 ± 4.6 25.7 ± 4.4 |
35.0 35.6 34.5 |
0.32 |
|
LAvol/ht² (ml/ m²) male female |
69 76 |
16 ± 2.8 15.6 ± 2.9 16.3 ± 2.8 |
21.6 21.4 21.9 |
0.175 |
|
LAvol/ht2.7 (ml/ m2.7) male female |
69 76 |
11.4 ± 2.2 11.4 ± 2.4 12.8 ± 2.6 |
15.8 16.2 18.0 |
0.005 |
Supplementary Table I: Normal values and the maximum normal (mean + 2 SD) for left atrium indexing by height, height² and height2.7 and by sex.
5. Discussion
Our study shows the normality for left atrial volume when indexing for height instead of indexing for body surface area. We used three different methods: volume/height (meters), volume/m2 (meters squared) and volume/height2.7 (meters raised to exponent 2.7), the last two are allometric measures. The LA volume indexed by BSA did not differ between groups and in obese patients it was even slightly smaller than in normal or overweight patients. When indexed by any of the three methods using height, LA volume increased progressively and linearly from the underweight, normal, overweight, and obese groups. A higher prevalence of atrial fibrillation and heart failure with preserved ejection fraction is recognized in obese patients, and it may be mediated by left atrial enlargement [10,11,14]. However, indexing LA size in obese or overweight patients is a challenging, and there are important limitations [9]. In this study, we found that 21 to 23% of obese patients and 7 to 9% of overweight patients with normal LA size when indexed by the BSA already had LA enlargement when indexed by height, using any of the three methods. It has been recognized that indexing many echocardiographic parameters for body size in obese patients is a challenging. Singh et al. recommend using height-based indexing instead of BSA in obesity [9]. They proposed the LA volume to be indexed for height² and using the cutoffs proposed by the The European Society of Cardiology (ESC). The ESC guidelines on management of arterial hypertension in adults recommend using LA volume indexed to height2 to define normal LA size (≤18.5 mL/m² for men; ≤16.5 mL/m² for women) [15]. In our population we found different cutoffs for normality of LA volume by height2 (maximum limit 21.6ml/m²), and it was not different for men or women. Applying the limits proposed by the ESC, we would make the diagnosis of dilated LA in 53% of our overweight patients and in 62% of the obese patients, and even in 36% of eutrophic patients and normal heart on echocardiography. So, it doesn't seem like we should use these cutoffs in our population, and we suggest to review this limit in other populations as well. However, an important point of our work is that we uniformly measured LA volume by Simpson's biplane method, which is recommended by echocardiography societies, while the method used for that ESC recommendation was the ellipsoid, which may explain differences. All three methods of height indexing for LA volume proved to be excellent predictors of enlarged LA in obese or overweight patients, with height squared indexing (LAvol/h²) being the strongest of them. Interestingly, we found 29.2 ml/m² the best cutoff value if we use LAvol/BSA to the diagnosis of LA enlargement in obese or overweight patients instead of 34ml/m² as universally used. In this work we show normal values of left atrial volume according to height using three different methods in eutrophic patients (normal weight, normal BMI) and it is suggested to improve LA size classification in obese and overweight patients. It seems likely that it can be used as well, without prejudice, across the entire weight and body mass index range. We have some limitations in this work. Initially, this is a single-center, retrospective study. It is still necessary to validate these data in other populations and with a larger sample. It was not possible to verify inter and intra observer variability. It was not possible to correlate these data with survival or clinical and cardiovascular events. We are already investigating these findings in pathological conditions, to observe the impact of reclassify the LA size and the severity of dilatation in obese and overweight patients.
References
- Kizer JR, Bella JN, Palmieri V, et al. Left atrial diameter as an independent predictor of first clinical cardiovascular events in middle-aged and elderly adults: The Strong Heart Study (SHS). Am Heart J 151 (2006): 412-418.
- Armstrong AC, Liu K, Lewis CE, et al. Left atrial dimension and traditional cardiovascular risk factors predict 20-year clinical cardiovascular events in young healthy adults: the CARDIA study (2014).
- Bombelli M, Facchetti R, Cuspidi C, et al. Prognostic Significance of Left Atrial Enlargement in a General Population Results of the PAMELA Study Epidemiology/Population. (2014).
- Gardin JM, McClelland R, Kitzman D, et al. M-Mode echocardiographic predictors of six- to seven-year incidence of coronary heart disease, stroke, congestive heart failure, and mortality in an elderly cohort (The Cardiovascular Health Study). Am J Cardiol 87 (2001): 1051-1057.
- Laukkanen JA, Kurl S, Eränen J, et al. Left Atrium Size and the Risk of Cardiovascular Death in Middle-Aged Men. Arch Intern Med. 165 (2005):1788-1793.
- Baumgartner H, Hung J, Bermejo J, et al. Recommendations on the Echocardiographic Assessment of Aortic Valve Stenosis: A Focused Update from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. J Am Soc Echocardiogr 30 (2017): 372-392.
- Fernandes LP, Barreto ATF, Neto MG, et al. Prognostic power of conventional echocardiography in individuals without history of cardiovascular diseases: A systematic review and meta-analysis. Clinics 76 (2021): 1-12.
- Lang RM, Badano LP, Victor MA, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28 (2015): 1-39.e14.
- Singh M, Sethi A, Mishra AK, et al. Echocardiographic Imaging Challenges in Obesity: Guideline Recommendations and Limitations of Adjusting to Body Size (2020).
- Zia I, Johnson L, Memarian E, et al. Anthropometric measures and the risk of developing atrial fibrillation: a Swedish Cohort Study. BMC Cardiovasc Disord 21 (2021): 1-10.
- Wang TJ, Parise H, Levy D, et al. Obesity and the Risk of New-Onset Atrial Fibrillation. JAMA 292 (2004): 2471-2477.
- Jeyaprakash P, Moussad A, Pathan S, et al. A Systematic Review of Scaling Left Atrial Size: Are Alternative Indexation Methods Required for an Increasingly Obese Population? J Am Soc Echocardiogr 34 (2021): 1067-1076.e3.
- Davis EF, Crousillat DR, He W, et al. Indexing Left Atrial Volumes. JACC Cardiovasc Imaging 15 (2022).
- Abed HS, Samuel CS, Lau DH, et al. Obesity results in progressive atrial structural and electrical remodeling: Implications for atrial fibrillation. Hear Rhythm 112 (2012).
- Laurent S, Lip GY, McManus R, et al. ESC/ESH Guidelines for the management of arterial hypertension (2018).


 Impact Factor: * 3.5
Impact Factor: * 3.5 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 14.80%
Acceptance Rate: 14.80%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 