Comparison of PEEK vs 3D printed titanium cage for ACDF- Is there any difference in subsidence?
Article Information
Dr. Harshadkumar A. Patel, MD1, Francine Zeng, MD2, Dr. Hardeep Singh, MD3, Dr. Scott S. Mallozzi, MD3, Mark Cote, P.T4, Dr. Isaac L. Moss, MD5*
1Assistant Professor, Department of Orthopedic surgery, Westchester Medical Center, New York Medical College, Valhalla, NY
2University of Connecticut, Farmington, CT
3Assistant professor, Department of Orthopedics surgery, Comprehensive Spine Center, University of Connecticut, Farmington, CT
4Biostatistician, Director of outcomes, research and quality, Department of orthopedic surgery, University of Connecticut, Farmington, CT
5Associate professor, Department of Orthopedics surgery, Comprehensive Spine Center, University of Connecticut, Farmington, CT
*Corresponding Author: Dr. Isaac L. Moss, MD, Chair and Associate professor, Department of Orthopedic Surgery, Comprehensive Spine Center, University of Connecticut, 263 Farmington Avenue, Farmington, CT 06030.
Received: 11 July 2023; Accepted: 17 July 2023; Published: 27 July 2023
Citation: Dr. Harshadkumar A. Patel, MD, Francine Zeng, MD, Dr. Hardeep Singh, MD, Dr. Scott S. Mallozzi, MD, Mark Cote, P.T, Dr. Isaac L. Moss, MD. Comparison of PEEK vs 3D printed titanium cage for ACDF- Is there any difference in subsidence? Journal of Spine Research and Surgery 5 (2023): 69-75
View / Download Pdf Share at FacebookAbstract
Objectives:
To compare the subsidence between PEEK vs new 3D printed titanium cage(3DTC) for ACDF surgery.
Design:
Retrospective cohort study Setting: Single academic spine center.
Methods/Outcome Measures:
All patients underwent a standard ACDF surgery with respective PEEK and 3DTC interbodies. Cage subsidence was measured as the change in adjusted intervertebral height (aIVH) in immediate post-operative and subsequent follow-up neutral radiographs at 6 months and ≥1-year visits. Severe subsidence was defined as ≥3 mm of aIVH loss on follow up. Basic demographic information and post-operative complications were also measured. Mixed effects linear models were constructed to evaluate difference in subsidence. A total of 26 patients (44 levels) in the PEEK group and 31 patients (48 levels) in the 3DTC group were available for review at minimum 6 months follow up.
Results:
There was no difference in demographic variables, including Charleston co-morbidity index, BMI and smoking status between groups. The overall average subsidence was 1.17 mm (95% CI : 0.82 – 1.51, p<0.001) at 6 months and 1.42 mm (95% CI: 1.07- 1.78, p<0.001) at 1-year follow up. The 3DTC group had significantly lower subsidence compared to the PEEK group at 6 months (0.84 mm vs 1.59 mm, p <0.05) and at 1 year (0.85 mm vs 1.92 mm, p<0.05). Severe subsidence rates were 9.37% for 3DTC group versus 19.04% for the PEEK group at 1 year.(P>0.05)
Conclusions:
3DTC leads to overall minor, but significant reduction in subsidence compared to PEEK cages in ACDF surgery. 3DTC has comparable severe subsidence rate to PEEK cage
Keywords
Cervical spine; Spondylosis; Anterior Cervical Discectomy and Fusion; Interbody Cages; PEEK; Titanium
articles about Cervical spine Research articles about Cervical spine review articles about Cervical spineCervical spine PubMed articles Cervical spine PubMed Central articles Cervical spine 2024 articles Cervical spine 2025 articles Cervical spine Scopus articles Cervical spine impact factor journals Cervical spine Scopus journals Cervical spine PubMed journals Cervical spine medical journals Cervical spine free journals Cervical spine best journals Cervical spine top journals Cervical spine free medical journals Cervical spine famous journals Cervical spine Google Scholar indexed journals articles about Spondylosis Research articles about Spondylosis review articles about SpondylosisSpondylosis PubMed articles Spondylosis PubMed Central articles Spondylosis 2025 articles Spondylosis 2026 articles Spondylosis Scopus articles Spondylosis impact factor journals Spondylosis Scopus journals Spondylosis PubMed journals Spondylosis medical journals Spondylosis free journals Spondylosis best journals Spondylosis top journals Spondylosis free medical journals Spondylosis famous journals Spondylosis Google Scholar indexed journals articles about Anterior Cervical Discectomy and Fusion Research articles about Anterior Cervical Discectomy and Fusion review articles about Anterior Cervical Discectomy and FusionAnterior Cervical Discectomy and Fusion PubMed articles Anterior Cervical Discectomy and Fusion PubMed Central articles Anterior Cervical Discectomy and Fusion 2026 articles Anterior Cervical Discectomy and Fusion 2027 articles Anterior Cervical Discectomy and Fusion Scopus articles Anterior Cervical Discectomy and Fusion impact factor journals Anterior Cervical Discectomy and Fusion Scopus journals Anterior Cervical Discectomy and Fusion PubMed journals Anterior Cervical Discectomy and Fusion medical journals Anterior Cervical Discectomy and Fusion free journals Anterior Cervical Discectomy and Fusion best journals Anterior Cervical Discectomy and Fusion top journals Anterior Cervical Discectomy and Fusion free medical journals Anterior Cervical Discectomy and Fusion famous journals Anterior Cervical Discectomy and Fusion Google Scholar indexed journals articles about Interbody Cages Research articles about Interbody Cages review articles about Interbody CagesInterbody Cages PubMed articles Interbody Cages PubMed Central articles Interbody Cages 2027 articles Interbody Cages 2028 articles Interbody Cages Scopus articles Interbody Cages impact factor journals Interbody Cages Scopus journals Interbody Cages PubMed journals Interbody Cages medical journals Interbody Cages free journals Interbody Cages best journals Interbody Cages top journals Interbody Cages free medical journals Interbody Cages famous journals Interbody Cages Google Scholar indexed journals articles about PEEK Research articles about PEEK review articles about PEEKPEEK PubMed articles PEEK PubMed Central articles PEEK 2028 articles PEEK 2029 articles PEEK Scopus articles PEEK impact factor journals PEEK Scopus journals PEEK PubMed journals PEEK medical journals PEEK free journals PEEK best journals PEEK top journals PEEK free medical journals PEEK famous journals PEEK Google Scholar indexed journals articles about Titanium Research articles about Titanium review articles about TitaniumTitanium PubMed articles Titanium PubMed Central articles Titanium 2029 articles Titanium 2030 articles Titanium Scopus articles Titanium impact factor journals Titanium Scopus journals Titanium PubMed journals Titanium medical journals Titanium free journals Titanium best journals Titanium top journals Titanium free medical journals Titanium famous journals Titanium Google Scholar indexed journals articles about Spine surgery Research articles about Spine surgery review articles about Spine surgerySpine surgery PubMed articles Spine surgery PubMed Central articles Spine surgery 2030 articles Spine surgery 2031 articles Spine surgery Scopus articles Spine surgery impact factor journals Spine surgery Scopus journals Spine surgery PubMed journals Spine surgery medical journals Spine surgery free journals Spine surgery best journals Spine surgery top journals Spine surgery free medical journals Spine surgery famous journals Spine surgery Google Scholar indexed journals articles about osseointegration Research articles about osseointegration review articles about osseointegrationosseointegration PubMed articles osseointegration PubMed Central articles osseointegration 2031 articles osseointegration 2032 articles osseointegration Scopus articles osseointegration impact factor journals osseointegration Scopus journals osseointegration PubMed journals osseointegration medical journals osseointegration free journals osseointegration best journals osseointegration top journals osseointegration free medical journals osseointegration famous journals osseointegration Google Scholar indexed journals articles about Spine surgeon Research articles about Spine surgeon review articles about Spine surgeonSpine surgeon PubMed articles Spine surgeon PubMed Central articles Spine surgeon 2032 articles Spine surgeon 2033 articles Spine surgeon Scopus articles Spine surgeon impact factor journals Spine surgeon Scopus journals Spine surgeon PubMed journals Spine surgeon medical journals Spine surgeon free journals Spine surgeon best journals Spine surgeon top journals Spine surgeon free medical journals Spine surgeon famous journals Spine surgeon Google Scholar indexed journals
Article Details
Introduction
Since its first introduction by Cloward[1] and Smith and Robinson[2], anterior cervical discectomy and fusion (ACDF) has become the gold standard of surgical treatment for patients with persistent symptomatic disc herniations, cervical myelopathy, or axial neck pain secondary to severe cervical spondylotic changes. After discectomy, a structural graft helps to achieve both patency of the neuroforamina and a solid fusion, as well as improvement of lordosis, if needed.
The traditional gold standard autologous iliac bone graft was associated with significant donor site morbidity, nonunion, and graft collapse[3,4] while allograft demonstrated slower incorporation and increased likelihood of collapse compared to autografts[5,6]. This has led to the development of interbody devices consisting of synthetic materials, with Titanium and Polyether-ether-ketone (PEEK) cages being most common[7]. Both Titanium and PEEK interbody cages have demonstrated favorable results when compared with allografts and autografts[8-10]. Titanium interbody devices offer immediate stability and osseointegration, with numerous studies revealing successful results after implantation[9,11,12]. However, these devices have been criticized for an increased risk of subsidence, likely secondary to the high modulus of elasticity of titanium relative to bone. Solid titanium cages have demonstrated subsidence rates of 13-45%, compared to 8-15% with PEEK interbodies[13]. Chou et al. have even concluded that Titanium cages have lower fusion rates and higher complication rates compared to both PEEK and autografts[14]. PEEK has a modulus of elasticity similar to cortical bone, which theoretically leads to improved load sharing and better stress distribution. So, PEEK cage likely leads to less subsidence and a possible reduction in associated complications [10,14]. However, PEEK surfaces have been found to be less hospitable for osteogenesis and bio-incorporation compared with titanium[15,16].
The new generation of 3D Printed Titanium cages (3DTC) are highly porous with reduced stiffness compared to the original solid titanium cages[17,18]. Theoretically, these implants could reduce the risk of subsidence while maintaining the ability to distract the disc space and enhance osseointegration. Although there are multiple studies comparing functional outcomes between PEEK and the conventional Titanium cage, there is a paucity of data comparing outcomes of the PEEK cage and 3DTC with anterior plate fixation. Apart from material properties, subsidence is affected by many aspects of surgical technique, including endplate preparation, area of interbody contact and over-distraction. In this retrospective study, we compared the radiological outcome of one/ two level PEEK cages vs 3DTC in ACDF, all performed by a single surgeon. A single surgeon case series was evaluated in order to control for factors related to surgical technique. We hypothesized that 3DTC cages will have comparable or perhaps even less subsidence compared to PEEK cages.
Material and Methods
A retrospective chart review was performed after approval from the hospital Institutional Review Board. The electronic medical record was queried for patients who underwent ACDF surgery based on the clinical procedural codes (CPT) codes (22551) between December 2014 and December 2019. Patients over the age of 18 years who underwent one/two level ACDF surgery by the single senior surgeon (IM) with the use of PEEK cage (Stryker AVS AS PEEK cage, Allendale, NJ) or 3D printed titanium cage (3DCT) (Stryker Tritanium C; Kalamazoo, MI) and an anterior plate were included. Patients with corpectomy, standalone cage ACDF, multilevel (≥3 levels) ACDF and combined anterior and posterior procedures were excluded.
The senior surgeon started using synthetic material cages for ACDF surgeries in December 2014. PEEK cages were used in consecutive patients from December 2014 to December 2017 and 3DTCs were used for all consecutive patients from December 2017 to December 2019. All patients meeting inclusion criteria were included in the study to limit selection bias. Demographic variables, including age, sex, body mass index (BMI), Charleston comorbidity index (CCI), smoking status and operative variables, including interbody type, size, and follow up data were collected. Radiographic evaluation was performed on immediate post-operative x-rays and then compared with post-operative x-rays at 6 months and at least 1 year. All patients underwent the standard Smith-Robinson surgical approach to the cervical spine, standard discectomy, preparation of endplates, cage placement with supplemental demineralized bone matrix (DBM) bone graft, and instrumentation using the same anterior cervical plating system. A total of 26 patients (44 levels) in the PEEK group and 31 patients (48 levels) in the 3DTC group were found to have ≥6 months of follow-up (Figure 1).
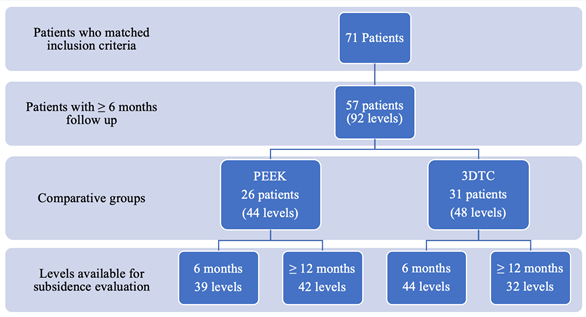
Figure 1: Patient selection flow chart
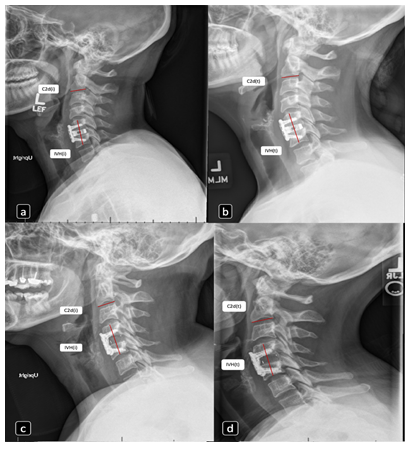
Figure 2: Subsidence measurement. (a and b): immediate post op and 1 year follow up neutral lateral x-ray of patient with one level ACDF with 3DTC; (c and d): immediate post op and 1 year follow up neutral lateral x-ray of patient with one level ACDF with PEEK; IVH(i): IVH on immediate post-operative x-ray; C2d(i): C2 inferior endplate depth on immediate post-operative x-ray; IVH(t): IVH at follow up; C2d(t): C2 inferior endplate depth at follow up)
Cage subsidence was measured as the change in the adjusted intervertebral height (IVH) between immediate post-operative and subsequent follow-up neutral position lateral radiographs[19]. IVH was measured from the midpoint of the superior endplate of the cephalad vertebrae to the midpoint of the inferior endplate of the caudal vertebrae. IVH was adjusted using the inferior endplate C2 vertebral body depth to account for magnification using the depicted formula (Figure 2).
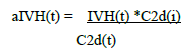
[aIVH(t): adjusted IVH at follow up, IVH(t): IVH at follow up, C2d(t): C2 inferior endplate depth at follow up, C2d(i): C2 inferior endplate depth on immediate post-operative x-ray]
This technique was selected to avoid potential measurement errors from x-ray magnification. All the radiographic measurements were performed by single orthopedic spine surgeon. Severe subsidence was defined as the ≥ 3 mm of change in the aIVH at follow up, when compared to immediate postoperative radiographs[13,20].
Results
There was no significant difference noted in patients’ age, sex, BMI, smoking status and CCI between groups (Table 1). No statistical difference was noted between groups with regards to the various operative variables collected, including number of levels, cage size and cage heights (Table 1). The most commonly fused level was C5-C6 (Table 2). Overall, subsidence was 1.17 mm (95% CI: 0.82 – 1.51, p<0.001) at 6 months and 1.42 mm (95% CI: 1.07- 1.78, p<0.001) at 1-year follow up. The 3DTC group had significantly lower subsidence compared to the PEEK group at 6 months (0.84 mm vs 1.59 mm, p <0.05) and at 1 year (0.85 mm vs 1.92 mm, p<0.05) (Table 3, Figure 3 and 4). Overall, severe subsidence rates were 9.37% for 3DTC group versus 19.04% for the PEEK group at 1 year. There was no significant difference in the subsidence between cage sizes within both groups. Follow up rate at 6 months was 80.0% and at 1 year was 64.2%. Only 1 patient in the PEEK group had a superficial infection at 2 weeks which was managed with oral antibiotics. There was no significant difference in complications between groups (p<0.05) (Table 4).
|
Cage type |
P value |
|||||
|
PEEK |
3DTC |
|||||
|
Total patients N |
26 |
31 |
- |
|||
|
1 level |
8 (30.8%) |
14 (45.1%) |
0.266 |
|||
|
2 level |
18 (69.2%) |
17 (54.8%) |
||||
|
Total Levels N(%) |
44 (48.8%) |
48 (52.2%) |
- |
|||
|
Age* |
50.9± 10.3 |
52.7 ± 10.9 |
0.516 |
|||
|
Sex† M:F, N(%) |
07:09 |
11:20 |
0.489 |
|||
|
(26.9%: 73.1%) |
(35.5%: 64.5%) |
|||||
|
Current smoker* |
3 (11.5%) |
8 (25.8%) |
0.174 |
|||
|
BMI† |
28.6 ± 8.3 |
30.0 ± 6.6 |
0.493 |
|||
|
CCI* N (%) |
0 |
8 (30.8%) |
7 (22.6%) |
0.651 |
||
|
1 |
6 (23.1%) |
5 (16.1%) |
||||
|
2 |
8 (30.77%) |
8 (25.81%) |
||||
|
3 |
4 (15.38%) |
8 (25.81%) |
||||
|
4 |
0 (0%) |
2 (6.45%) |
||||
|
5 |
0 (0%) |
1 (3.2%) |
||||
|
Cage size ‡ |
06:37 |
11:36 |
0.253 |
|||
|
(Small: Large) |
(14.0%: 86.0%) |
(23.4%: 76.6%) |
||||
|
Cage height(mm)¥ |
5 |
2 (4.5%) |
3 (6.4%) |
0.612 |
||
|
6 |
25 (56.8%) |
22 (46.8%) |
||||
|
7 |
1 7(38.6%) |
22 (46.8%) |
||||
* Analysis conducted using Fisher’s Exact test
† Analysis conducted using student’s t-test
‡ Cage size information was missing for 1 level in each group
¥ Cage height information was missing for 1 level in titanium group
Table 1: Basic demographic variable distribution between two groups
|
Cage type |
||
|
PEEK |
3DTC |
|
|
C2-C3 |
1 |
0 |
|
C3-C4 |
2 |
4 |
|
C4-C5 |
4 |
10 |
|
C5-C6 |
20 |
21 |
|
C6-C7 |
17 |
12 |
|
C7-T1 |
0 |
1 |
Table 2: Distribution of fused levels
|
Cage type |
P- value |
|||
|
PEEK (N levels) |
3DTC (N levels) |
Mean difference (Δ) in subsidence (95% CI) |
||
|
At 6 months |
1.53 (39) |
0.84 (44) |
0.69 (0.04 - 1.34) |
0.037* |
|
At ≥ 1 year |
1.92 (42) |
0.85 (32) |
1.07 (0.39 – 1.76) |
0.002* |
|
Severe subsidence (≥ 3 mm) (N levels) |
||||
|
At 6 months |
4/39 (10.35%) |
1/44 (2.27%) |
- |
0.182 |
|
At ≥ 1 year |
8/42 (19.04%) |
3/32 (9.37%) |
- |
0.331 |
*P-value is statistically significant
Table 3: Mean difference in subsidence and severe subsidence rate at 6 months and at 1 year
|
Cage type |
P- value |
||
|
PEEK (26 patients) |
3DTC (31 patients) |
||
|
Dysphagia* |
9 (34.6%) |
9 (29%) |
0.651 |
|
Infection |
1 (3.8%) |
0 |
- |
|
Neurologic complication |
0 |
0 |
- |
*Analysis conducted using chi2 test
Table 4: Comparison of complications between the groups
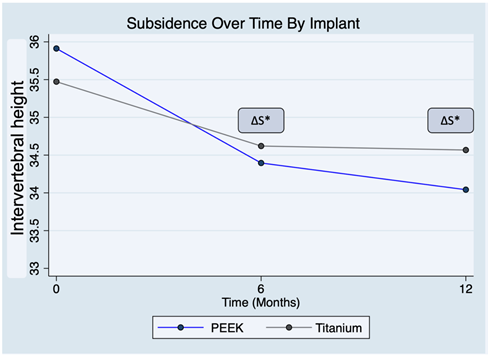
Figure 3: Subsidence over time. ΔS : Mean difference in subsidence at particular time point , * P-value is significant
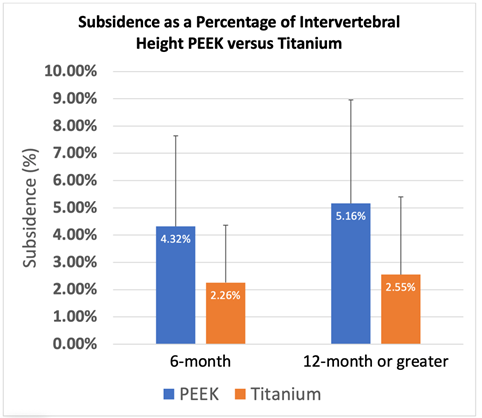
Figure 4: Subsidence is presented as a percentage of intervertebral height. PEEK had significantly higher subsidence compared to titanium at 6 month and 12 months follow-up. (P<0.05)
Discussion
The ideal interbody cage should provide immediate stability and promote osseointegration in order to achieve bony fusion and maintain indirect decompression through disc space distraction. Cage subsidence reduces foraminal height, possibly leading to malalignment, recurrence of radiculopathy and poor functional outcomes after ACDF surgery[20]. The rate of cage subsidence has been used as an outcome measure for success and compared between different types of interbody devices in the past. Prior studies have demonstrated that titanium induces greater osteoblast differentiation from stem cells compared to PEEK, leading to a more favorable bone-implant contact surface and superior osseointegration with surrounding bone[21]. This inherent characteristic leads to improved fusion rates compared to PEEK, but at the cost of increased subsidence from high modulus of elasticity[22].
Additive manufacturing (i.e. 3D printing) with titanium allows the creation of open cellular lattices with different densities to modulate implant stiffness, with the goal of more closely approximating the properties of spinal bone[23]. The highly porous architecture also mimics cancellous bone, leading to a reduction of stress shielding at the bone-implant interface. Along with this added benefit, 3D printing also allows the feature of “in growth” topologies and pores that specifically encourage osseointegration and increases bone bonding[18]. Therefore, 3D printing technology can increase, or at least maintains, the fusion ability characteristic of the standard titanium, with a potential added advantage of subsidence reduction[17]. Our study found that 3DTC has 1.07 mm (95% CI 0.39 – 1.76) less subsidence compared to PEEK cages at 1 year follow up (p<0.05). Brecevich et al. previously demonstrated 95.37% fusion rates in their 108 ACDF levels with 3DTC, without incidence of severe subsidence (≥3 mm) or cage migration. However, they did not present actual subsidence numbers regarding each fusion level[17]. Despite our study revealing a minor, but statistically significant reduction in subsidence with 3DTC, there is no available literature to suggest the clinical significance of this minor subsidence.
In general, ACDF surgery leads to significant improvement in postoperative outcomes for all primary diagnoses over long term follow up, but several studies have shown lower patient satisfaction and outcome scores in patients with severe subsidence (≥ 3mm)[24]. Cabraja et al. evaluated subsidence in 86 single level ACDF patients and noted that solid titanium group had 20.5% subsidence while PEEK group had 14.3% subsidence[25]. Overall, severe subsidence rate was higher in PEEK (19.04%) compared to 3DTC (9.37%) in our study at ≥1 year follow up, but the difference was not statistically significant. Post-hoc analysis showed that a new study would need a sample of 204 in each group to be powered at 80% with an alpha level of 0.05. In other words, our study revealed that severe subsidence rates in 3DTC is likely comparable to PEEK, which was a drawback to the traditional solid titanium cage.
Literature has been regionally biased due to the fact that European and Asian studies predominantly report results of standalone cages without any screws while, while studies performed in the United States have predominantly reported outcomes of cage/screw combinations (standalone with screw(s) or cage with anterior plate and screws). Noordhoek et al. systematically compiled seventy-one studies and reported subsidence for different cage types and cage-screw combinations (CSC) [20]. They found that cage-screw combination has significantly lower subsidence rates, followed by PEEK, titanium and PMMA cages (15.1%, 23.5%, 24.9% and 30.2%, respectively; p<0.001) [20]. Our overall subsidence rate (14.86%) was similar to the CSC subsidence rate. Anterior plates for vertebral body fixation lead to stress shielding and likely reduces the degree of subsidence. Therefore, anterior plating or standalone cage with screws, which is a nearly universal ACDF technique in the United States provides inherent protection against subsidence, irrespective of the cage material.
The strength of this study includes the involvement of a single surgeon, which provides consistency in surgical technique- especially endplate preparation, the consistent use of same design PEEK cages and 3DTC, and a relatively large number of levels in both groups. The limitations of this study include its nature of being a retrospective cohort study, which has its inherent flaws and biases. There is also a lack of associated patient reported outcomes or satisfaction score to further elucidate the clinical effect of the subsidence difference. Even though, study has reported 1 year follow-up, it would be ideal to have at least 2 years follow-up. As this study only focus on subsidence and most subsidence occur during initial bone-resorption stage of bony healing, there is less likelihood that further longer follow up would change the result. Nearly 35.8% levels did not follow up for 1 year and later visit, which could have led to attrition bias in the result. It is crucial to carefully interpret the final result. Even though, overall study power is small, there were a total of 92 levels available to evaluate the radiological outcome, which is reasonable number considering the single surgeon cohort.
Conclusion
3DCT has a small, but significant reduction in subsidence compared to PEEK cages. Overall, the severe subsidence rate is relatively comparable between 3DTC and PEEK. A large power randomized control trial would be helpful to further evaluate clinically significant severe subsidence and long-term surgical outcomes of newer 3DTC interbody devices.
Funding:
No funding was received for the study.
References
- Cloward R. The anterior approach for removal of ruptured cervical disks. J Neurosurg 15 (1958):602-617.
- Smith G, Robinson R. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 40 (1958): 607-624.
- Young W, Rosenwasser R. An early comparative analysis of the use of fibular allograft versus autologous iliac crest graft for interbody fusion after anterior cervical discectomy. Spine (Phila Pa 1976), 18 (1993): 1123-1124.
- Younger EM, Chapman MW. Morbidity at bone graft donor sites. J Orthop Trauma 3 (1989): 192-195.
- Malloy KM, Hilibrand AS. Autograft versus allograft in degenerative cervical disease. Clin Orthop Related Res 1 (2002): 27-38.
- Zdeblick TA, Ducker TB. The use of freeze-dried allograft bone for anterior cervical fusions. Spine (Phila Pa 1976), 16 (1991): 726-729.
- Chong E, Pelletier MH, Mobbs RJ, et al. The design evolution of interbody cages in anterior cervical discectomy and fusion: a systematic review. BMC Musculoskelet Disord 16 (2015): 99.
- Moreland DB, Asch HL, Clabeaux DE, et al. Anterior cervical discectomy and fusion wtih implantable titanium cage: initial impressions, patient outcomes and comparison to fusion wtih allograft. Spine J 4 (2004):184-191.
- Thome C, Krauss JK, Zevgaridis D. A prospective clinical comparison of rectangular titanium cages and iliac creset autografts in anterior cervical discectomy and fusion. Neurosurg Rev 27 (2004): 34-41.
- Cho DY, Liaeu WR, Liu JT, et al. Preliminary experience using a polyetheretherketone (PEEK) cage in the treatment of cervical disc disease. Neurosurgery 51 (2002): 1343-1350.
- Hwang SL, Hwang YF, Lieu AS, et al. Outcome analyses of interbody titanium cage fusion used in the anterior discectomy for cervical degenerative disc disease. J Spinal Disord Tech 18 (2005): 326-331.
- Hwang SL, Lin CL, Lieu AS, et al. Three-level and four-level anterior cervical discectomies and titanium cage-augmented fusion with and without plate fixation. J Neurosurg Spine 1 (2004): 160-167.
- Chen Y, Wang X, Lu X, et al. Comparison of titanium and polyetheretherketone (PEEK) cages in the surgical treatment of multilevel cervical spondylotic myelopathy: a prospective, randomized, control study with over 7-year follow-up. Eur Spine J 22 (2013): 1539-1546.
- Chou YC, Chen DC, Hseieh WA, et al. Efficacy of anterior cervical fusion: comparison of titanium cages, polyetheretherketone (PEEK) cages and autogenous bone grafts. J Clin Neurosci 15 (2008): 1240-1245.
- Olivares-Navarrete R, Gittens RA, Schneider JM, et al. Osteoblasts exhibit a more differentiated phenotype and increased bone morphogenetic protein production on titanium alloy substrates than on poly-ether-ether-ketone. Spine J 12 (2012): 265-272.
- Iunes EA, Barletta EA, Barba Belsuzarri TA, et al. Correlation between different interbody grafts and pseudoarthrosis after anterior cervical discectomy and fusion compared with control group: systematic review. World Neurosurg 134 (2020): 272-279.
- Brecevich AT, Abjornson C, Cammisa FP. P135. Radiological outcomes of a novel 3-dimensional printed titanium cervical interbody cage following single and multilevel anterior cervical discectomy and fusion: a case series of 108 operated levels. Spine J 19 (2019): S220.
- Choy WJ, Parr WCH, Phan K, et al. 3-dimensional printing for anterior cervical surgery: a review. J Spine Surg 4 (2018): 757-769.
- Wang M, Chou D, Chang CC, et al. Anterior cervical discectomy and fusion performed using structural allograft or polyetheretherketone: pseudoarthrosis and revision surgery rates with minimum 2-year follow-up. J Neurosurg Spine 32 (2019): 562-569.
- Noordhoek I, Koning MT, Jacobs WCH, et al. Incidence and clinical relevance of cage subsidence in anterior cervical discectomy and fusion: a systematic review. Acta Neurochir 160 (2018): 873-880.
- Banik BL, Riley TR, Platt CJ, et al. Human mesenchymal stem cell morphology and migration on microtextured titanium. Front Bioeng Biotechnol 4 (2016): 41.
- Seaman S, Kerezoudis P, Bydon M, et al. Titanium vs. polyetheretherketone (PEEK) interbody fusion: Meta-analysis and review of the literature. J Clin Neurosci 44 (2017): 23-29.
- Murr LE, Gaytan SM, Medina F, et al. Characterization of Ti–6Al–4V open cellular foams fabricated by additive manufacturing using electron beam melting, Mater Sci Eng A 527 (2010): 1861-1868.
- Kast E, Derakhshani S, Bothmann M, et al. Subsidence after anterior cervical inter-body fusion. A randomized prospective clinical trial. Neurosurg Rev 32 (2009): 207-214.
- Cabraja M, Oezdemir S, Koeppen D, et al. Anterior cervical discectomy and fusion: comparison of titanium and polyetheretherketone cages. BMC Musculoskelet Disord 13 (2012):172.


 Impact Factor: * 3.123
Impact Factor: * 3.123 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 14.90%
Acceptance Rate: 14.90%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 