Effectiveness of Combined Hysterolaparoscopy on the Quality of Life of Patients with Endometriosis: A Retrospective Review in Hungary
Article Information
Atombosoba Adokiye Ekine1*, István Fülöp1, István Tekse1, Zoltán Kovács1, Pál Siklós1, Ágnes Koppán2, Miklós Koppán M3
1Department of Obstetrics and Gynaecology, Robert Károly Private Hospital, Budapest, Hungary
2Faculty of Health Sciences, University of Pécs, Pécs, Hungary
3Department of Obstetrics & Gynaecology, University of Pécs, Pécs, Hungary
*Corresponding author: Dr. Atombosoba Adokiye Ekine, Department of Obstetrics &Gynaecology, Robert Károly Private Hospital, Budapest, Hungary
Received: 28 February 2020; Accepted: 10 March 2020; Published: 14 March 2020
Citation:
Atombosoba Adokiye Ekine, István Fülöp, István Tekse, Zoltán Kovács, Pál Siklós, Ágnes Koppán, Miklós Koppán M. Effectiveness of Combined Hysterolaparoscopy on the Quality of Life of Patients with Endometriosis: A Retrospective Review in Hungary. Journal of Women’s Health and Development 3 (2020): 032-055.
View / Download Pdf Share at FacebookAbstract
Objectives: Endometriosis degrades the quality of life of women and places an enormous burden on families and the healthcare system. The purpose of including hysteroscopy to laparoscopy, which is the mainstay for the diagnosis and treatment, was to evaluate and treat both the specific and nonspecific abnormalities that can impair fertility and well-being by improving surgical efficacy. This study aimed to highlight the effectiveness of combined hysterolaparoscopy on the quality of life in women.
Materials and Methods: This was a retrospective hospital-based study on 777 women who underwent combined hysterolaparoscopy at the endoscopy department of the hospital, for endometriosis-related symptoms.
Results: All 777 women were diagnosed with endometriosis by surgery and were in the range of stages 1 to 4 by the revised American Society of Reproductive Medicine. The mean age was 34.3 ± 5.1 years; the average age at the onset of symptoms was 29.1 ± 4.3 years. Pregnancy was successful in 81.3% (370/455) of those with infertility, with a live birth rate of 94.2% (327/347). The quality of life improved significantly, with 46% to 49% having moderate to significant improvement, and 35-% to 54% achieving significant complete resolution of symptoms (p<0.0005). Dyspareunia (80%), dysmenorrhea (74%), and infertility (69%) were the most common complaints.
Conclusions: Similar to other previous clinical studies on the quality of life of patients with endometriosis, this study showed significantly satisfactory outcomes of hysterolaparoscopy, regardless of disease stage and severity. Hysterolaparoscopy may be an adaptable treatment model after a thorough evaluation of patients and their desires.
Keywords
Hysterolaparoscopy; Endometriosis
Hysterolaparoscopy articles Hysterolaparoscopy Research articles Hysterolaparoscopy review articles Hysterolaparoscopy PubMed articles Hysterolaparoscopy PubMed Central articles Hysterolaparoscopy 2023 articles Hysterolaparoscopy 2024 articles Hysterolaparoscopy Scopus articles Hysterolaparoscopy impact factor journals Hysterolaparoscopy Scopus journals Hysterolaparoscopy PubMed journals Hysterolaparoscopy medical journals Hysterolaparoscopy free journals Hysterolaparoscopy best journals Hysterolaparoscopy top journals Hysterolaparoscopy free medical journals Hysterolaparoscopy famous journals Hysterolaparoscopy Google Scholar indexed journals Endometriosis articles Endometriosis Research articles Endometriosis review articles Endometriosis PubMed articles Endometriosis PubMed Central articles Endometriosis 2023 articles Endometriosis 2024 articles Endometriosis Scopus articles Endometriosis impact factor journals Endometriosis Scopus journals Endometriosis PubMed journals Endometriosis medical journals Endometriosis free journals Endometriosis best journals Endometriosis top journals Endometriosis free medical journals Endometriosis famous journals Endometriosis Google Scholar indexed journals socioeconomic articles socioeconomic Research articles socioeconomic review articles socioeconomic PubMed articles socioeconomic PubMed Central articles socioeconomic 2023 articles socioeconomic 2024 articles socioeconomic Scopus articles socioeconomic impact factor journals socioeconomic Scopus journals socioeconomic PubMed journals socioeconomic medical journals socioeconomic free journals socioeconomic best journals socioeconomic top journals socioeconomic free medical journals socioeconomic famous journals socioeconomic Google Scholar indexed journals sociocultural articles sociocultural Research articles sociocultural review articles sociocultural PubMed articles sociocultural PubMed Central articles sociocultural 2023 articles sociocultural 2024 articles sociocultural Scopus articles sociocultural impact factor journals sociocultural Scopus journals sociocultural PubMed journals sociocultural medical journals sociocultural free journals sociocultural best journals sociocultural top journals sociocultural free medical journals sociocultural famous journals sociocultural Google Scholar indexed journals hormones articles hormones Research articles hormones review articles hormones PubMed articles hormones PubMed Central articles hormones 2023 articles hormones 2024 articles hormones Scopus articles hormones impact factor journals hormones Scopus journals hormones PubMed journals hormones medical journals hormones free journals hormones best journals hormones top journals hormones free medical journals hormones famous journals hormones Google Scholar indexed journals estrogen articles estrogen Research articles estrogen review articles estrogen PubMed articles estrogen PubMed Central articles estrogen 2023 articles estrogen 2024 articles estrogen Scopus articles estrogen impact factor journals estrogen Scopus journals estrogen PubMed journals estrogen medical journals estrogen free journals estrogen best journals estrogen top journals estrogen free medical journals estrogen famous journals estrogen Google Scholar indexed journals progesterone articles progesterone Research articles progesterone review articles progesterone PubMed articles progesterone PubMed Central articles progesterone 2023 articles progesterone 2024 articles progesterone Scopus articles progesterone impact factor journals progesterone Scopus journals progesterone PubMed journals progesterone medical journals progesterone free journals progesterone best journals progesterone top journals progesterone free medical journals progesterone famous journals progesterone Google Scholar indexed journals endometrial polyps articles endometrial polyps Research articles endometrial polyps review articles endometrial polyps PubMed articles endometrial polyps PubMed Central articles endometrial polyps 2023 articles endometrial polyps 2024 articles endometrial polyps Scopus articles endometrial polyps impact factor journals endometrial polyps Scopus journals endometrial polyps PubMed journals endometrial polyps medical journals endometrial polyps free journals endometrial polyps best journals endometrial polyps top journals endometrial polyps free medical journals endometrial polyps famous journals endometrial polyps Google Scholar indexed journals laparoscopic articles laparoscopic Research articles laparoscopic review articles laparoscopic PubMed articles laparoscopic PubMed Central articles laparoscopic 2023 articles laparoscopic 2024 articles laparoscopic Scopus articles laparoscopic impact factor journals laparoscopic Scopus journals laparoscopic PubMed journals laparoscopic medical journals laparoscopic free journals laparoscopic best journals laparoscopic top journals laparoscopic free medical journals laparoscopic famous journals laparoscopic Google Scholar indexed journals pelvic inflammatory disease articles pelvic inflammatory disease Research articles pelvic inflammatory disease review articles pelvic inflammatory disease PubMed articles pelvic inflammatory disease PubMed Central articles pelvic inflammatory disease 2023 articles pelvic inflammatory disease 2024 articles pelvic inflammatory disease Scopus articles pelvic inflammatory disease impact factor journals pelvic inflammatory disease Scopus journals pelvic inflammatory disease PubMed journals pelvic inflammatory disease medical journals pelvic inflammatory disease free journals pelvic inflammatory disease best journals pelvic inflammatory disease top journals pelvic inflammatory disease free medical journals pelvic inflammatory disease famous journals pelvic inflammatory disease Google Scholar indexed journals
Article Details
1. Introduction
Endometriosis is a chronic cancer-like disease that is characterized by numerous adverse effects on quality of life (QoL). The diagnosis of endometriosis is frequently delayed. In fact, Nnoaham et al. reported that the average duration between onsets to diagnosis was about 6.7 years [1]. Perhaps, the increasing incidence of endometriosis is one of the sources of additional cost for healthcare service providers, families, and the public [2]. Although the exact etiology is unknown, it is one of the most common gynecological diseases, is a poorly understood chronic illness that has a high level of complexity, and is often misdiagnosed [3]. Similar to other studies [2, 4, 5], this study showed that endometriosis is a disease in women in their prime of life, at a mean age of 29.1 ± 4.3 years. With regard to its occurrence, there have been no sociocultural, ethnic, and socioeconomic perspectives [2, 6, 7]. Worldwide, endometriosis was reported to affect at least 10% of women in their reproductive age [6, 7], and literature from various authors has suggested that the rate of endometriosis-related global infertility was close to 22% to 50% and that about 30% to 50% of women with endometriosis were infertile [5, 8]. The symptoms associated with endometriosis vary and are largely dependent on and/or sometimes influenced by localization, spread (stage), individual pain threshold, and patient need [3, 9]. The endometriotic tissues outside the uterine cavity behave like their counterparts in the uterus and are cyclically influenced by the sex hormones namely, estrogen and progesterone [3, 4]. Endometriotic cells/tissues cause chronic inflammatory reactions, which can result in scar tissue formation, adhesions, and eventually, displacement or distortion of lower pelvic reproductive organs [7, 8]. However, according to some scholars, the cause of subfertility or infertility is the increased peritoneal fluid concentration of biochemicals, such as prostaglandins, protease, and cytokines, including the inflammatory cytokines IL1, IL6, and TNFα; the other angiogenic cytokines, such as IL8 and VEGF, are secreted from the distorted reproductive organs from adhesions [8, 10, 11]. This process is the cause of the symptoms and complaints of patients. Sometimes, Endometriosis is associated with mood swings and depression, which can occasionally lead to self-destructive lifestyles. Frequently reported symptoms are chronic pelvic pain, waist pain, infertility, dysmenorrhea, and dyspareunia, whereas the rarely reported symptoms include dysuria and gastrointestinal dysfunction such as bloating and dyschezia [4, 5, 8]. Subsequently, the changes in the anatomical and biochemical milieu can adversely affect the fallopian tubes, embryo, sperm and ovum transport, and functional abilities capable of lead to serious negative effects on fertility [10-12].
The complex nature of endometriosis is evident from both the symptomatology and laparoscopic findings because the symptoms do not always correlate with the disease stage. While some patients with minimal stage I to II disease show devastating pain, others with severe disease in stages III to IV are asymptomatic or have less painful episodes [13]. This high rate of endometriosis-related infertility influenced the inclusion of hysteroscopy for treatment in this study. Some of the benefits of hysteroscopy are the capacity to evaluate and treat all intrauterine abnormalities such as endometrial polyps, adhesions, and septum. The combined surgical procedure was reported by some scholars to be an effective means of fertility evaluation [5, 15]. However, some of the limitations of hysteroscopy are the lack of adequate expertise and cost. Because infertility is very complex and controversial, the essence of combining the hysteroscopy with laparoscopy comes from the hope of improving outcomes. Furthermore, the symptoms associated with endometriosis can negatively affect a patient’s well-being and lead to work productivity and financial losses, including the cost of off the counter painkiller drugs and hospital medical cost, and the likes. This factor has necessitated the development of more radical laparoscopic surgical procedures, especially when infertility is involved; besides, many scholars have also recognized this as a better treatment approach [13, 16-18]. This study aims to validate the postsurgical impact of hysterolaparoscopy on the QoL, including the reproductive performance of patients with endometriosis and infertility problems.
2. Patients and Methods
This retrospective single hospital center study was conducted on 777 women who visited the general gynecological consulting unit and the endoscopic department (endoscopic and IVF unit of the Robert Károly Private Hospital, Budapest) from January 2010 to December 2016 for infertility issues and other endometriosis-associated painful symptoms. Access to the hospital’s computerized patient database was approved by the hospital ethics committee. All patients had endometriosis at different stages and were referred to the minimal access gynecology (endoscopic) department of the hospital for combined hysterolaparoscopy during the study period. Women with polycystic ovary syndrome; pelvic inflammatory disease; primary medical conditions, such as neurologic, psychiatric, gastrointestinal, urologic, and orthopedic diseases; and current use of drugs that can affect cognition and mood were excluded. The patient’s well-being and improvement of QoL were assessed by verbal questions on the absence of painful symptoms, fertility performance, and general mood during the follow-up visits or through electronic media. The variables considered for this study included age, type of pain-related symptoms (i.e., dysmenorrhea, dyspareunia, chronic pelvic pain, or urinary symptoms), general history, history of previous gynecologic surgery, mode of discovery, type of surgery, stage of endometriosis, postsurgical outcome, infertility, pregnancy outcome, and other ultrasound findings, such as the presence of polyps, septum, and adhesions. The grade or severity of endometriosis was based on the laparoscopy findings, using the principle of the rAFS score, including powder-burn black, red, white, yellow, dark blue, brown, or nonpigmented lesions. The size, depth, and location of these lesions were considered and categorized into four stages [19].
The decision for surgical management was based on the symptoms and signs suggestive of endometriosis, past medical history, ultrasound findings, and results of other investigative procedures, including magnetic resonance imaging (MRI), computed tomography (CT), and serum markers. The postsurgical follow-up lasted for at least 1–2 years (until December 2018, according to the date of surgery), depending on the major needs of the patients. Endometriosis was scored according to the revised American Fertility Society (rAFS) score [19, 41]. Those with infertility issues and who desired to bear a child (n = 445) were followed-up for 24 months; those who became pregnant were followed-up until term or the end of pregnancy. Those with complaints other than infertility, such as chronic pelvic pain, dysmenorrhea, dyspareunia, dysuria, and dyschezia, were followed-up for 12 months. During each visit, the patients underwent general gynecologic and ultrasound evaluations for disease recurrence. Those who did not follow-up for evaluation were contacted by direct electronic communication, such as email or telephone. All data were entered into SPSS version 24. The collected data were expressed as mean and standard deviation, frequency, percentage, or cumulative percentage. The associations among age, stage, laparoscopic surgical management, and fertility performance were assessed using the chi-square test for categorical data or the two-sample t-test for continuous variables. We adopted a multiple binary logistic regression model to determine the statistical relationship, using age as control. A P value <0.050 was considered to indicate a statistical significance.
3. Results
All 777 patients who underwent hysterolaparoscopy were evaluated in the final analysis. All patients were Caucasians, and the mean age of patients was 34.3 ± 5.1 years (range, 18–53 years). The mean age at menarche was 13.1 ± 1.4 years; the mean duration of menstruation was 5.9 ± 2.1 days; the average age at the onset of endometriosis-related symptoms was 29.1 ± 4.3 years; and the duration from the onset of symptoms to the diagnosis of endometriosis was 5.1 ± 2.9 years (Table 1). The surgical intervention confirmed the suspicion of endometriosis by various investigation methods. The staging was verified based on the intraoperative findings, using the rAFS score system; there were 15% (113/777) patients in stage 1, 31% (243/777) in stage 2, 34% (264/777) in stage 3, and 20% (157/777) in stage 4 (Table 1). The most frequently encountered complaints were dyspareunia 80% (621/777) and dysmenorrhea 74% (574/777). Among the 534 (69%) patients who initially complained of infertility, 49 declined to bear a child after the surgery (Figure 1). Some of the pain-related symptoms associated with endometriosis independently occurred, also sometimes in combination (Table 2 and Figure 2). Rectovaginal septum 59% (458/777) and the left ovary in 45% (349/777) are the most affected sites (Figure 3). The associations between the presenting painful complaints and the types of pain are illustrated in (Table 2). Also, the most likely descriptions were crushing pain for patients with dysmenorrhea and sharp pain for patients with dyspareunia. However, based on the statistical analyses, most of the patients with dysuria and dyschezia experienced all forms of pain (Table 2). Table 3 demonstrates the correlations and influence of the different sites of endometriosis on the symptoms of the patients. Notably, more complex symptomatology was seen when the right ovary was involved than when the left ovary was involved (Table 3).
In general, endometriosis rarely occurs on a single site within the abdominal cavity. It occurs at multiple sites most of the time, as seen in this study (Figure 4). This mixture of localization coupled with other yet to be established factors could influence the complexity of the symptoms of the disease. In general, endometriosis was suspected based on the medical history and investigative procedures, such as ultrasound, and was confirmed by surgery (Figure 5). The major surgical procedures, including laser carbon dioxide techniques, which were performed in this study, are shown in Figure 6. The incidence of previous gynecologic surgery was high at 44.4% (345/777). Nevertheless, in general, there was a significant improvement in the QoL at 12 months after surgery (Table 4). Table 5 illustrates how the various types of endometriosis-related painful symptoms affected the QoL. Regrettably, improvement was relatively less in the complaints of intestinal obstipation and hematochezia, whereas few acknowledged slight pains associated with dyschezia and dysuria (Table 5). Relapse of endometriosis was seen in 4.2% (33/777) (p=0.005). As shown in Figure 8, obtuse pain completely disappeared after surgery. With regard to fertility performance at the end of the 24 months of follow-up, 81.3% (370/455) (p=0.039) of women who desired to bear a child became pregnant. As shown in Figure 9, the rate of successful live birth was 94.2% (327/347) and that for pregnancy loss was 5.8%. Overall, there was gradual improvement in the QoL of women during follow-up, and every woman exhibited a significant level of improvement (p=0.0005) (Figures 10a and b). Moreover, hysterolaparoscopy had some influence on the success rate of fertility performance (Figure 11 and 12).
|
Patients’ age |
|||
|
Age (years) |
Frequency |
% |
Cumulative % |
|
18–25 |
27 |
3.47 |
3.5 |
|
26–31 |
155 |
19.9 |
29.5 |
|
32–37 |
349 |
44.9 |
74.4 |
|
38–43 |
172 |
22.1 |
96.5 |
|
44–53 |
27 |
3.4 |
100 |
|
Age at menarche (years) |
|||
|
8–11 |
76 |
9.8 |
9.8 |
|
12–15 |
664 |
85.5 |
95.3 |
|
16–20 |
37 |
4.7 |
100 |
|
Duration of menstruation (Days) |
|||
|
2–7 |
629 |
81.0 |
81 |
|
8–15 |
148 |
19.0 |
100 |
|
Age at the onset of symptoms (years) |
|||
|
15–20 |
16 |
2.1 |
2.1 |
|
21–25 |
136 |
17.0 |
19.1 |
|
26–30 |
345 |
44.4 |
63.5 |
|
31–35 |
228 |
29.3 |
92.5 |
|
36–40 |
47 |
6.1 |
98.5 |
|
41–43 |
7 |
0.9 |
100 |
|
Duration of symptoms before diagnosis |
|||
|
0–5 |
450 |
57.9 |
57.9 |
|
6–11 |
286 |
36.8 |
94.7 |
|
12–18 |
41 |
5.3 |
100 |
|
Stages of endometriosis (rARM) classification) |
|||
|
Stage 1 |
113 |
14.5 |
14.5 |
|
Stage 2 |
243 |
31.3 |
45.8 |
|
Stage 3 |
264 |
34.0 |
79.8 |
|
Stage 4 |
157 |
20.2 |
100.0 |
|
Total |
777 |
100.0 |
100.0 |
Table1: General characteristics of patients with endometriosis (N =777).
The figure shows the relative frequency / likelihood of each symptom contributing to endometriosis.
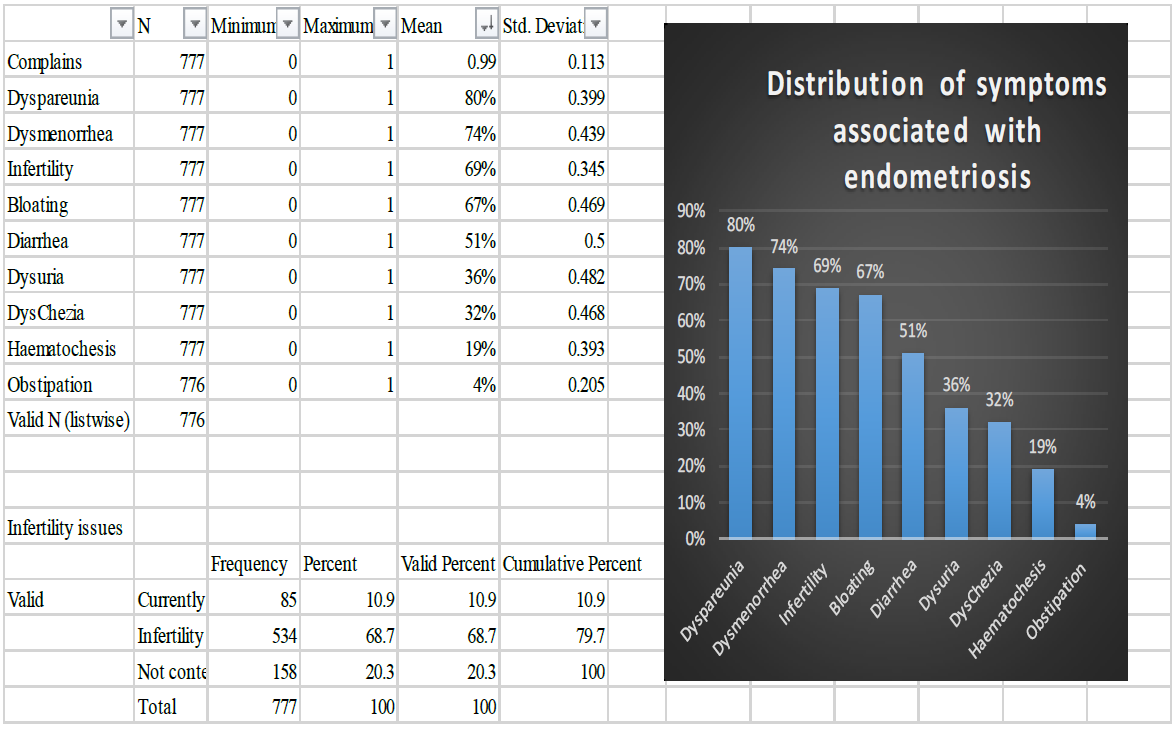
Figure 1: Descriptive distribution of endometriosis related symptoms (n=777).
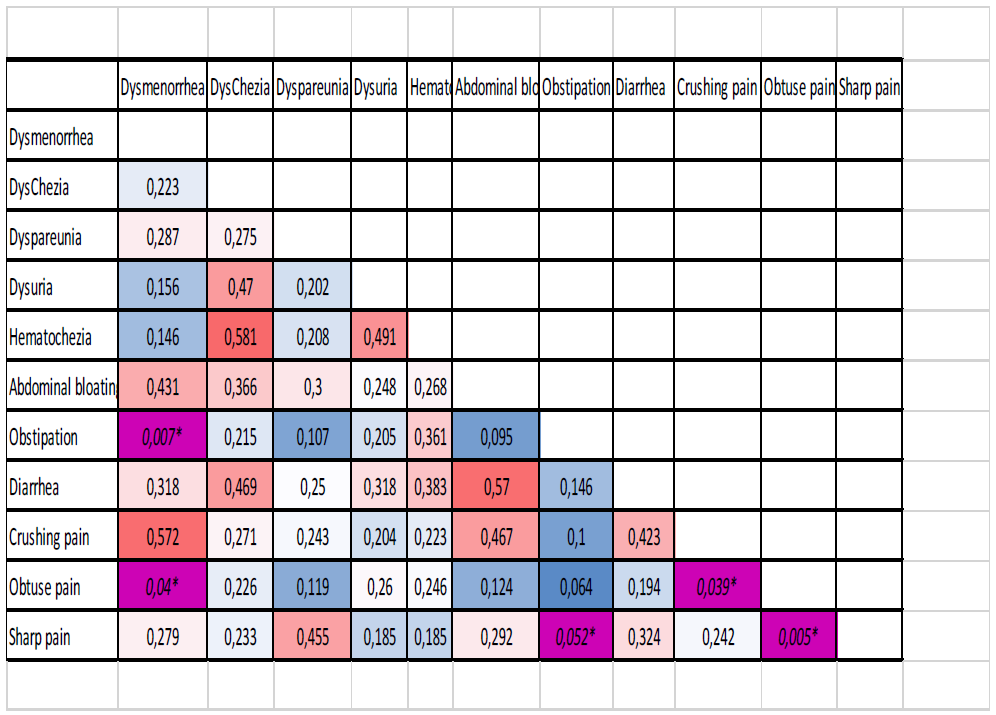
Table 2: The relationship between the type of pain and symptoms in patients with endometriosis (N =777).
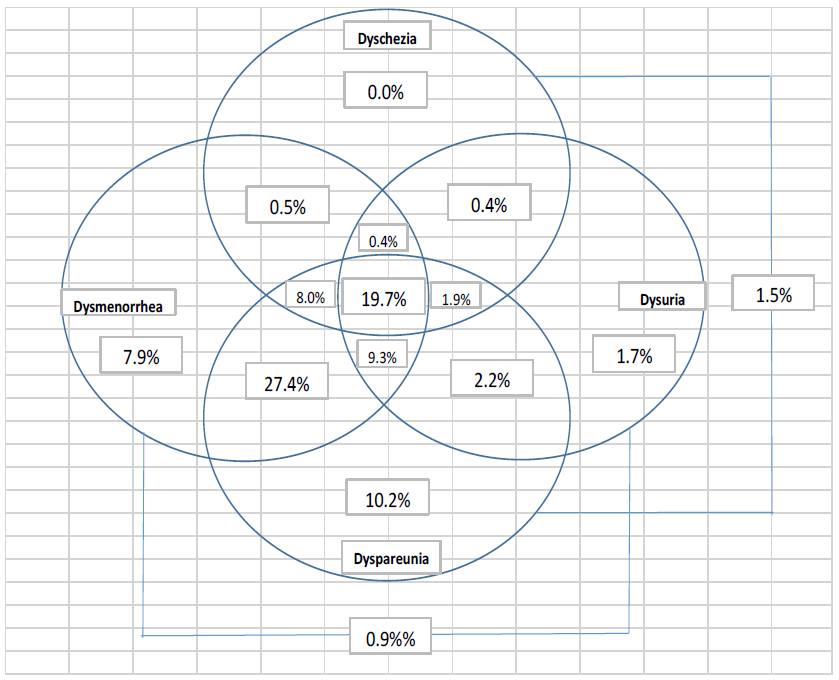
Figure 2: The prevalence and overlap of pain related symptoms in women with endometriosis, as diagnosed surgically among the women (n=777).
The figure shows the frequency / probability of occurrence of endometriosis on each body part
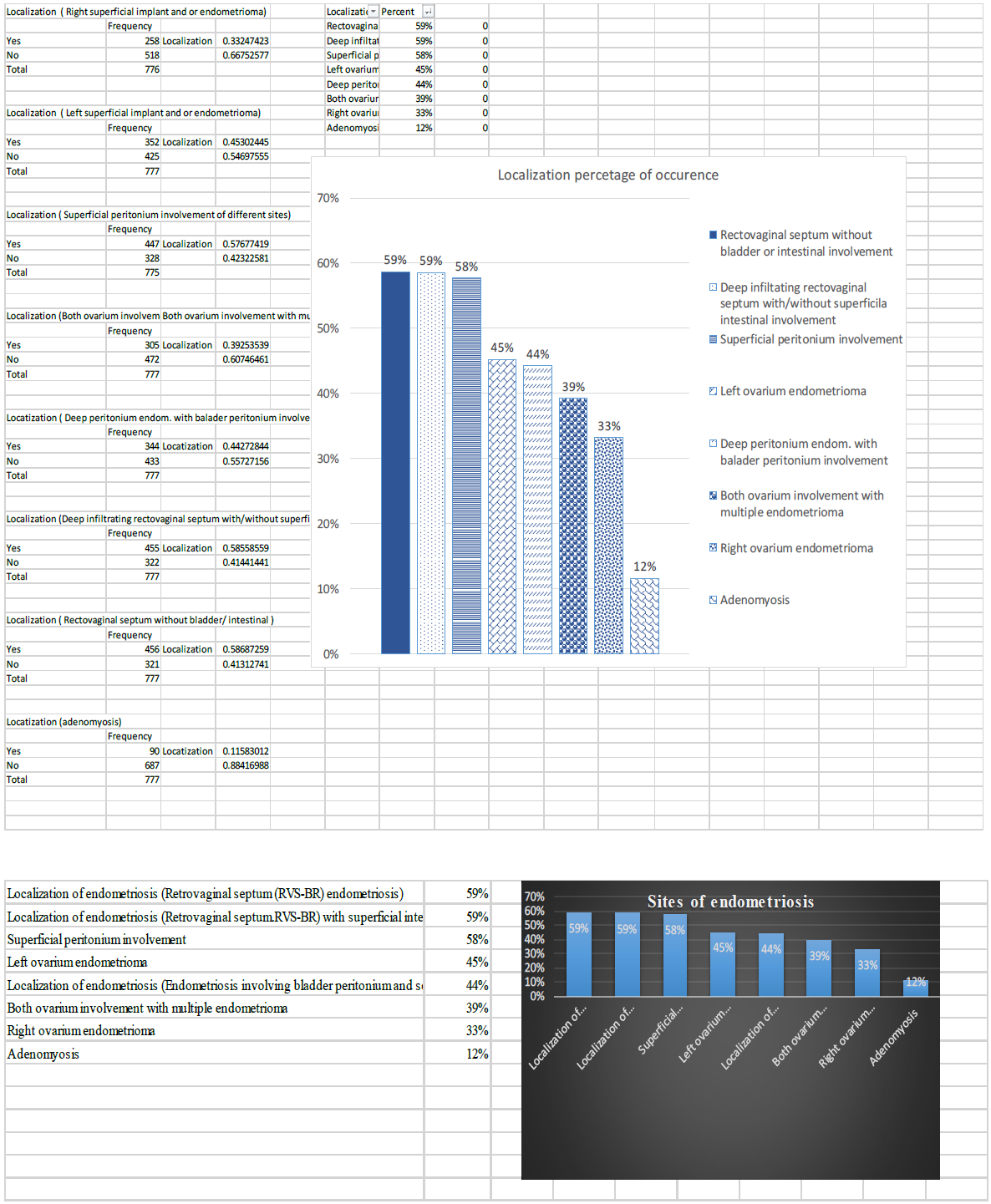
Figure 3: The commonest location of endometriosis among the women=777).
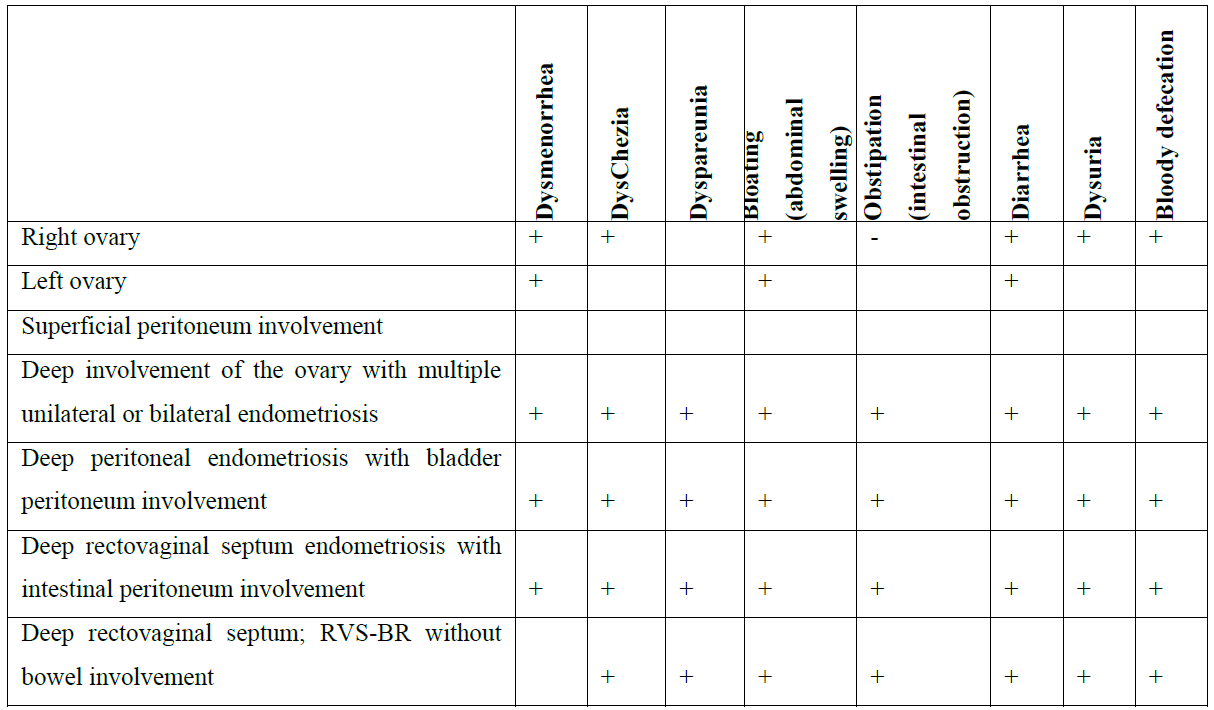
Table 3: The relationship between symptoms and localization of endometriosis (N = 777).
Bilateral superficial ovary endometriosis lesion (BSOE), bilateral ovary endometrioma (BDOE), Deep peritoneum endometriosis (RVS-B-R), Superficial peritoneum endometriosis (PE), Right superficial ovary lesion (RSOE), Right ovary endometrioma (RDOE), Left superficial ovary lesion (LSOE), Left ovary endometrioma (LDOE)
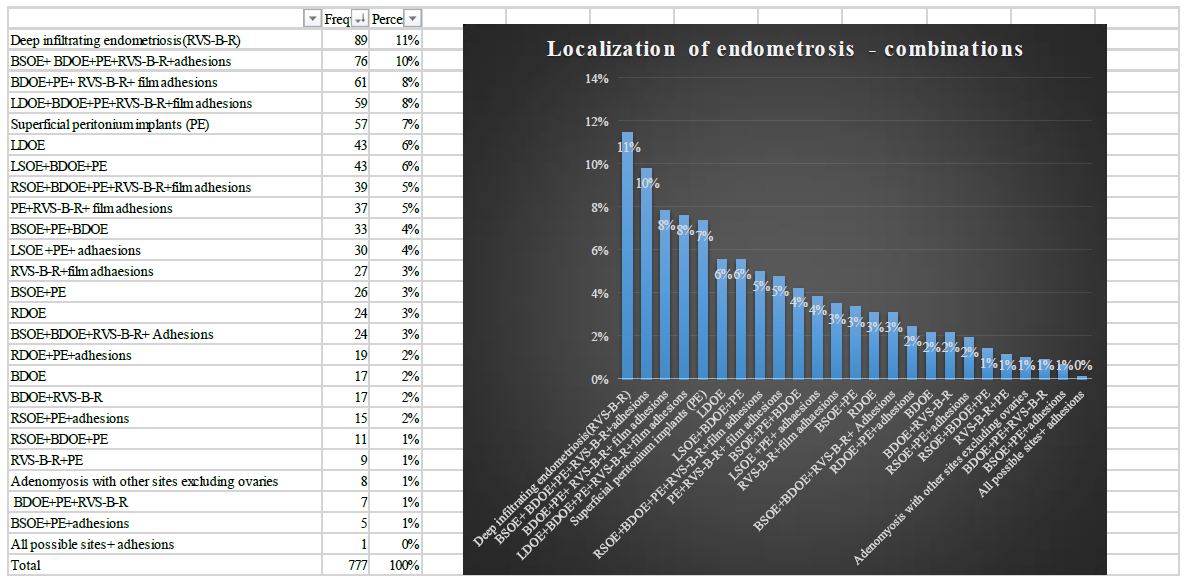
Figure 4: The commonest location combination of endometriosis among the women=777).
Distribution of methods used to detect endometriosis. It can be seen that in 91% of cases, Anamnesis + US + Laparoscopy and Anamnesis + Laparoscopy led to successful discovery
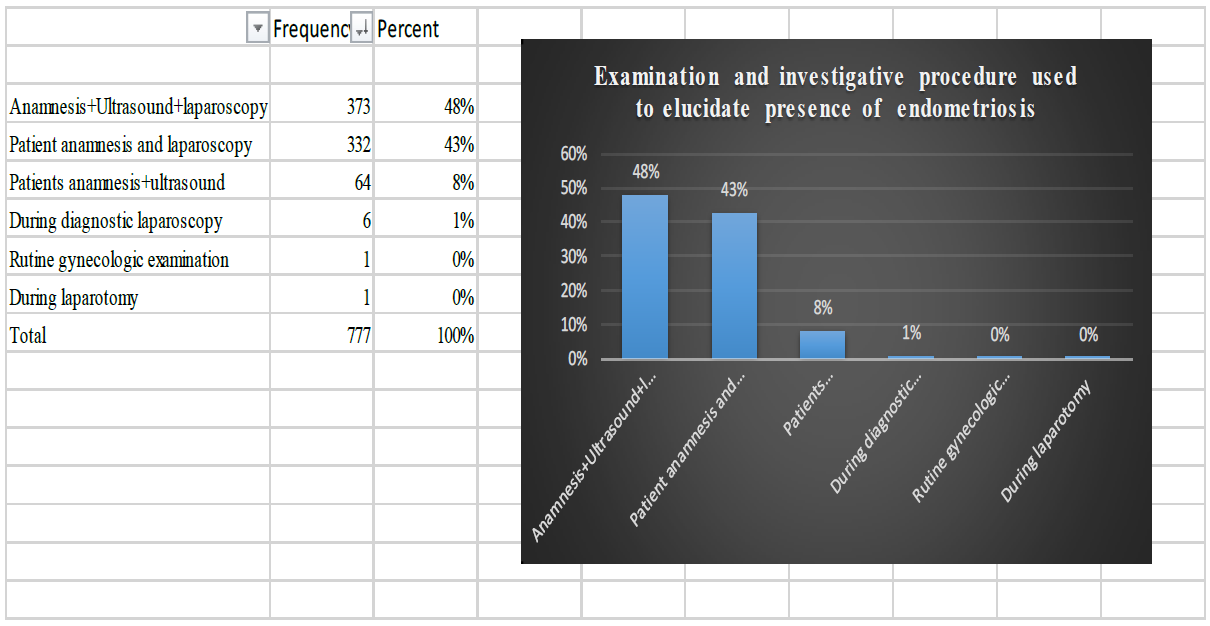
Figure 5: Mode of discovery of endometriosis in women (n=777).
The relative frequencies of the 15 types of surgery are shown in the figure. The most commonly used were EEPL + EEDL + AEOL (27%), or two of these 3 (EEPL + AEOL: 13%, EEPL + EEDL: 11%), or EEDL itself (11%)
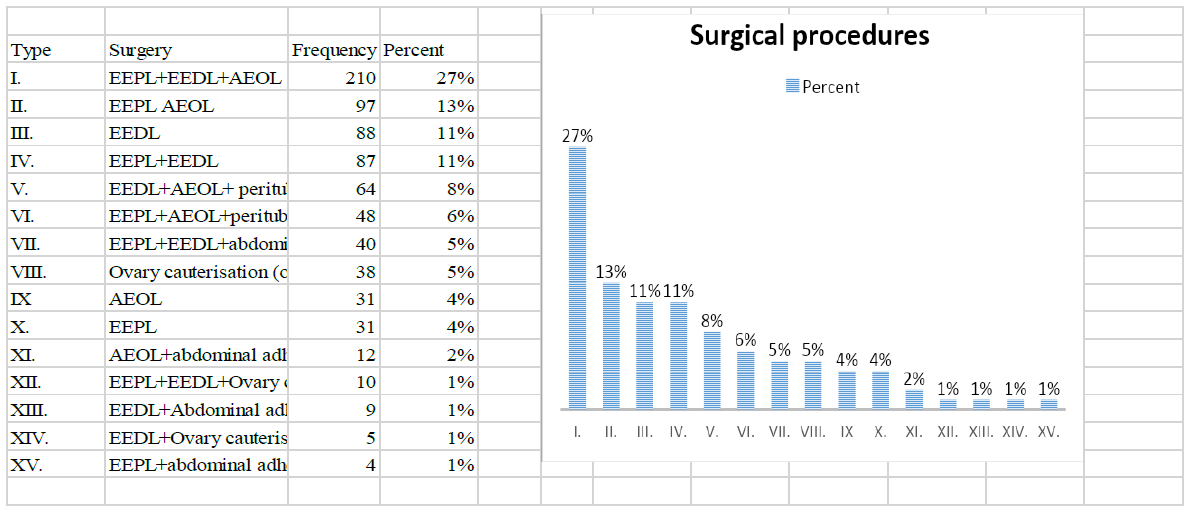
Figure 6: Laparoscopy surgery with patients with endometriosis including Co2 laser (n=774).
(Electrocoagulation excision peritoneal endometriosis lesion (EEPL), Electrocoagulation excision of deep endometriosis lesion (EEDL), Stripping of ovary endometrioma lesion (AEOL), Ovary cauterisation, Peritubal and/ or abdominal adhesiolysis)
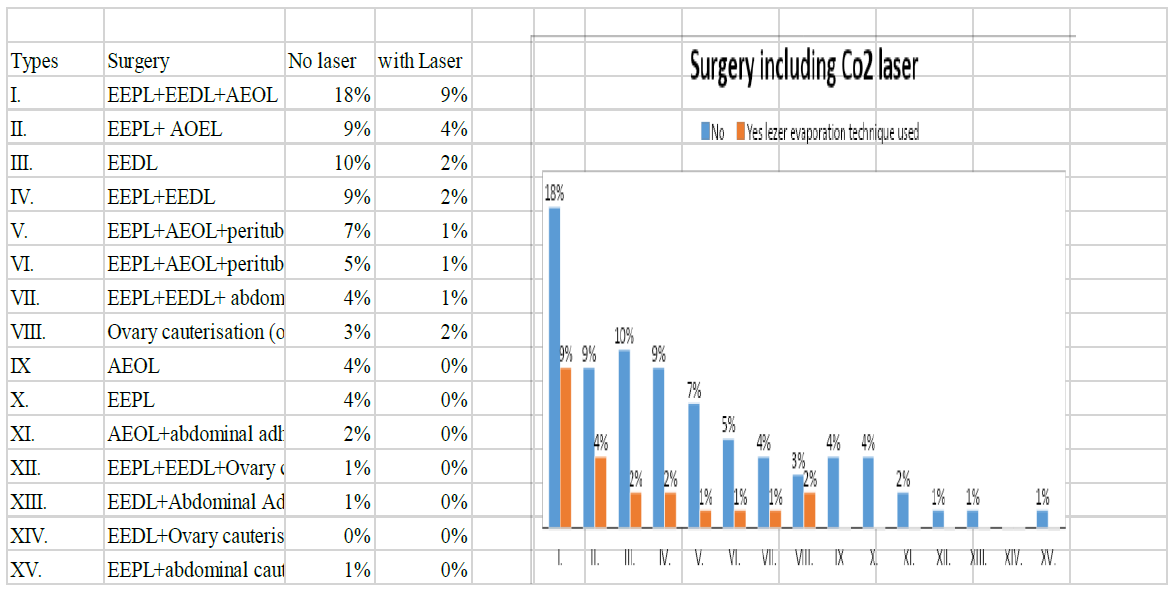
Figure 6: Laparoscopy surgery with patients with endometriosis including Co2 laser (n=774).
|
Time (months) |
Count |
Moderate |
Significant |
Complete |
Total |
Chi-Square test |
Value |
df |
Asymptotic significance (two-sided) |
|
First 3 months |
0 |
7 |
52 |
53 |
112 |
Pearson Chi- |
12.524a |
2 |
0.002 |
|
% within the first visit |
46.70% |
74.30% |
88.30% |
77.20% |
Likelihood ratio |
11.778 |
2 |
0.003 |
|
|
1 |
8 |
18 |
7 |
33 |
Linear by linear association |
11.697 |
1 |
0.001 |
|
|
% within first visit |
53.30% |
25.70% |
11.70% |
22.80% |
|||||
|
Total |
Count |
15 |
70 |
60 |
145 |
||||
|
% within first |
100.00% |
100.00% |
100.00% |
100.00% |
|||||
|
First 6 months |
0 |
4 |
52 |
55 |
111 |
Pearson Chi- |
9.988a |
2 |
0.007 |
|
% within the sixth visit |
40.00% |
75.30% |
84.60% |
77.10% |
Likelihood ratio |
8.701 |
2 |
0.013 |
|
|
1 |
6 |
17 |
10 |
33 |
Linear by linear association |
7.708 |
1 |
0.005 |
|
|
% within the sixth visit |
60.00% |
24.60% |
15.40% |
22.90% |
|||||
|
Total |
Count |
10 |
69 |
65 |
144 |
||||
|
% within the sixth visit |
100.00% |
100.00% |
100.00% |
100.00% |
|||||
|
First 12 months |
0 |
5 |
44 |
51 |
100 |
Pearson Chi- |
20.988a |
2 |
0 |
|
% within the 12th visit |
31.30% |
77.20% |
86.40% |
75.80% |
Likelihood ratio |
18.301 |
2 |
0 |
|
|
1 |
11 |
13 |
8 |
32 |
Linear by linear association |
15.966 |
1 |
0 |
|
|
% within the 12th visit |
68.80% |
22.80% |
13.60% |
24.20% |
|||||
|
Total |
Count |
16 |
57 |
59 |
132 |
||||
|
% within 12th |
100.00% |
100.00% |
100.00% |
100.00% |
|||||
|
One cell (16.7%) has an expected count of <5. The minimum expected count is 3.88. |
|||||||||
Table 4: Comparison of the improvements of symptoms after surgery across the different stages of follow-up in patients with endometriosis (N = 777).
|
First month visit |
Sixth month visit |
First year visit |
|
|
Dysmenorrhea |
<0.001 |
<0.001 |
<0.001 |
|
DysChezia |
<0.001 |
<0.001 |
<0.001 |
|
Dyspareunia |
<0.001 |
<0.001 |
<0.001 |
|
Bloating (abdominal swelling) |
<0.001 |
<0.001 |
<0.001 |
|
Obstipation (intestinal obstruction) |
0.585 |
0.700 |
0.701 |
|
Diarrhea |
<0.001 |
<0.001 |
<0.001 |
|
Dysuria |
<0.001 |
<0.001 |
<0.001 |
|
Bloody defecation |
<0.001 |
<0.001 |
<0.001 |
|
Crushing pain |
<0.001 |
<0.001 |
<0.001 |
|
Obtuse pain |
0.006 |
0.001 |
0.001 |
|
Sharp pain |
<0.001 |
<0.001 |
<0.001 |
Table 5: Improvement of the individual endometriosis-related symptoms and QoL within 12 months after surgery.
General well-being was measured on the following scales: Little improvement less than 50% Moderate im-provement of symptoms 50-60% significant improvement of symptoms 70-80% Complete improvement of symptoms 90-100% Replaced by the following mean values, I determined average well-being at 1 month, 6 months, and 1 year after surgery: 25%, 55%, 75%, and 95%.The chart clearly shows that patient well-being has increased for each symptom, so the positive effect of surgery has been confirmed
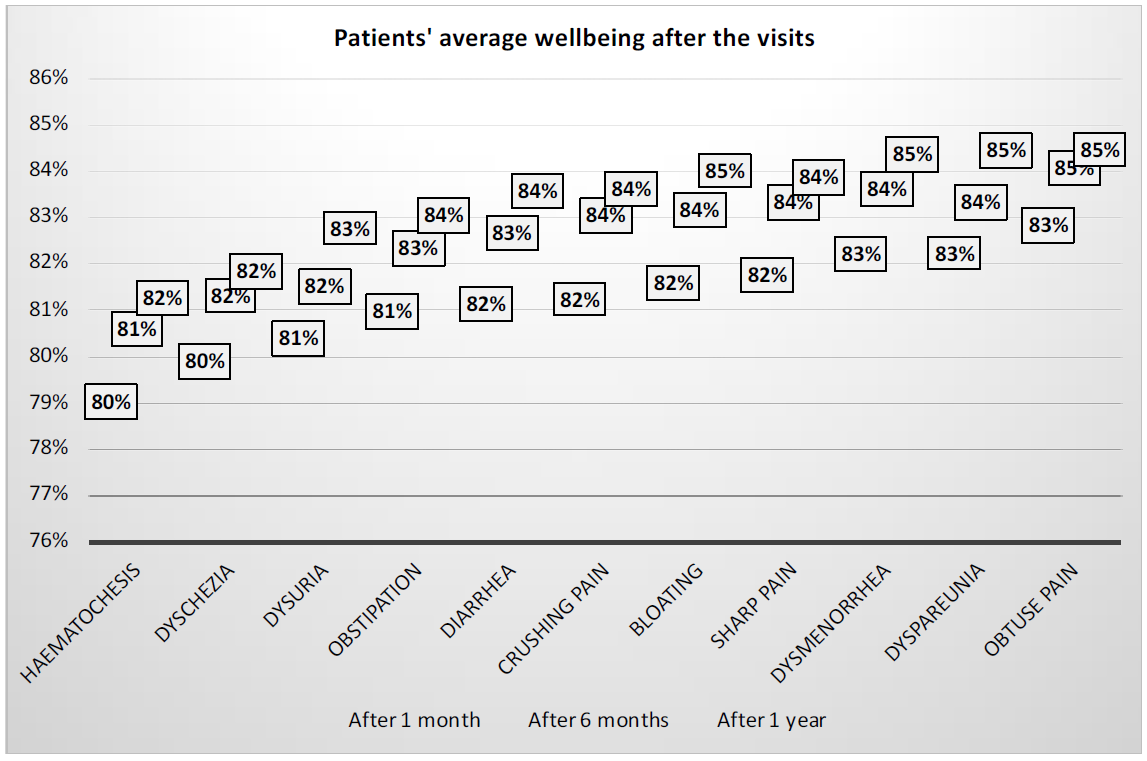
Figure 8: Surgical effect on the quality of life (QoL) during follow-up (n=777).
|
Chi-square test |
Value |
df |
Asymptotic Significance (2-sided) |
|
1 month |
31.847 |
3 |
<0.001 |
|
6 months |
30.302 |
2 |
<0.001 |
|
1 year |
33.51 |
2 |
<0.001 |
|
Beyond 1 year |
312.685 |
3 |
<0.001 |
There is a significant relationship between the rate of improvement and the time of visit (see table above), meaning that patients have reported an increasing improvement over time. The Moderate improvement rate alone decreased, but this also strengthens the improvement, as the other two improvement factors (Significant and Complete) were "at the expense of" the change. Significant and complete reported an improvement of 57-59% on the first visit, but this rate was 74-85% on the last visit (after 1 year)
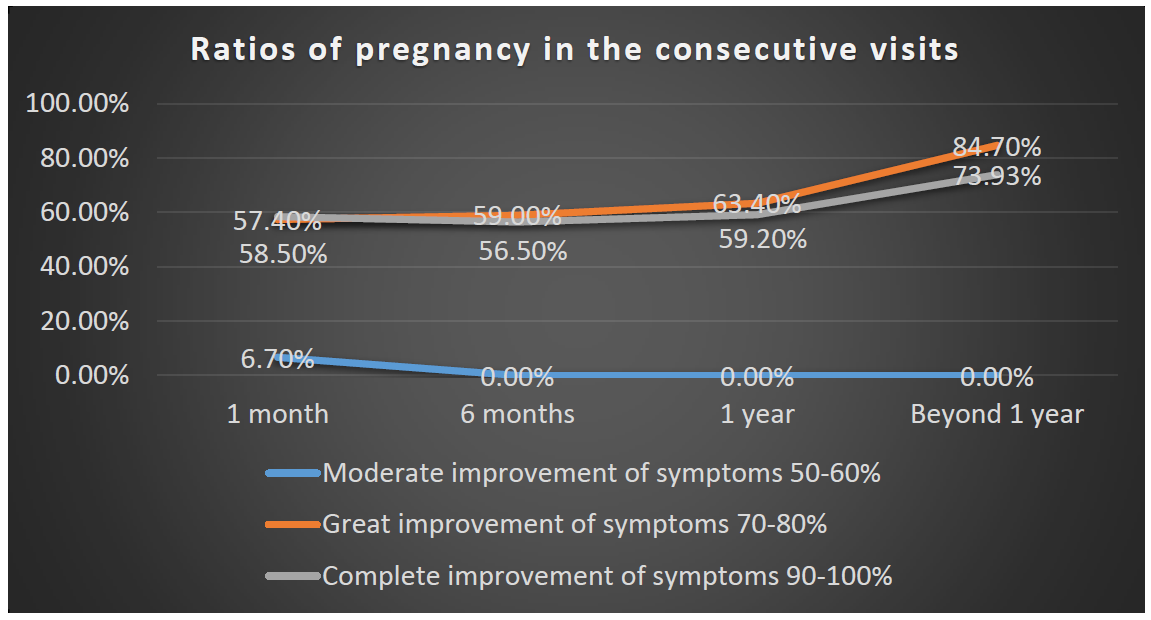
Figure 9: The relationship between women wellbeing to infertility performance post surgically (n=455).
Overall recovery was progressively higher over time, as evidenced by the increasing and increasing number of Significant and Complete improvements in subsequent visits
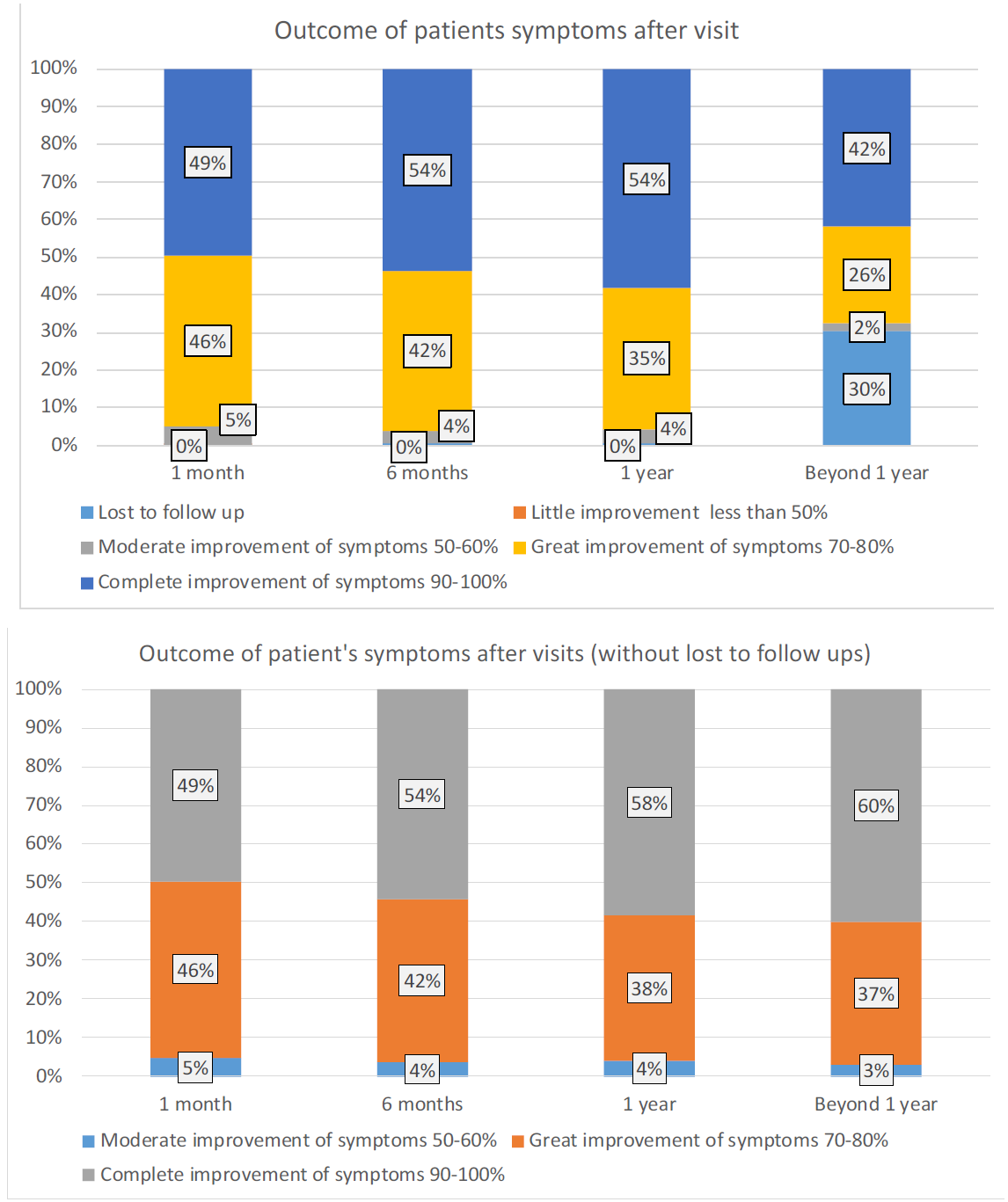
Figure 10a-1-2: Women wellbeing after the surgical management spreading within the 12 months follow-up period (n=777).
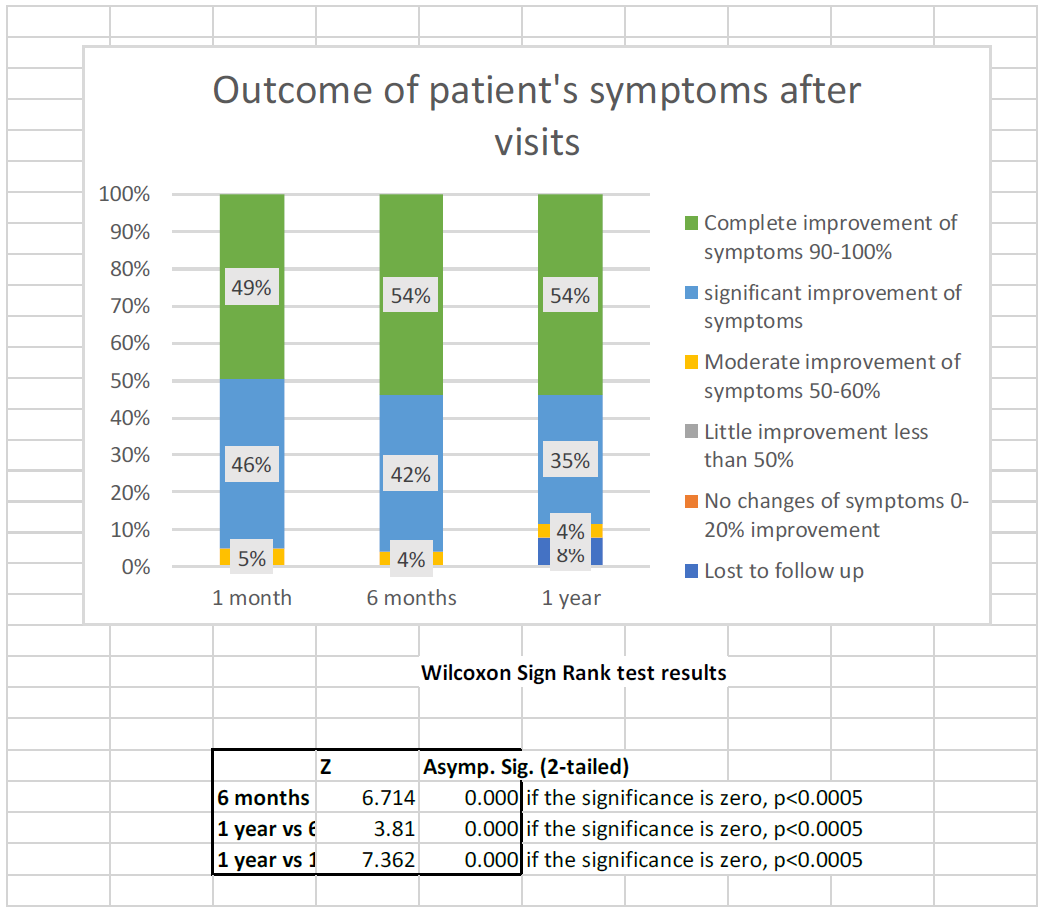
Figure 10b: Women wellbeing after the surgical management spreading within the 12 months follow-up period (n=777).
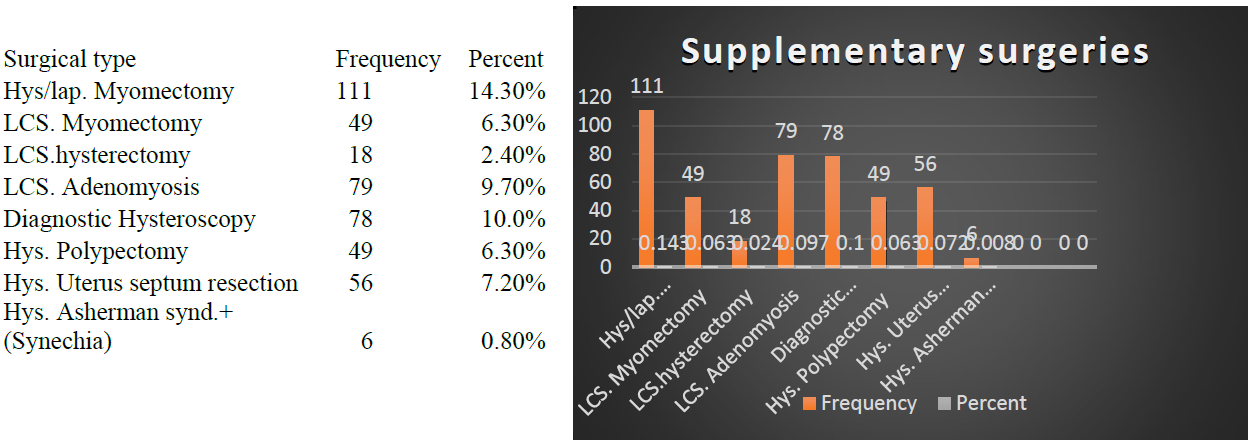
Figure 11: Other surgeries performed in addition to endometriosis in the women (n=777).
|
Visit |
Improvement |
Chi-square |
df |
Sig |
Odds ratio |
95% confidence interval |
|
|
Lower |
Upper |
||||||
|
1 month |
Little improvement less than 50% |
1.253 |
1 |
0.263 |
0.000 |
0.000 |
0.000 |
|
Moderate improvement of symptoms 50-60% |
30.418 |
1 |
<0.001 |
0.052 |
0.012 |
0.220 |
|
|
Significant improvement of symptoms 70-80% |
0.823 |
1 |
0.364 |
1.152 |
0.849 |
1.562 |
|
|
Complete improvement of symptoms 90-100% |
2.125 |
1 |
0.145 |
1.254 |
0.925 |
1.702 |
|
|
6 months |
Moderate improvement of symptoms 50-60% |
29.912 |
1 |
<0.001 |
0.000 |
0.000 |
0.000 |
|
Significant improvement of symptoms 70-80% |
2.342 |
1 |
0.126 |
1.272 |
0.935 |
1.731 |
|
|
Complete improvement of symptoms 90-100% |
0.224 |
1 |
0.636 |
1.076 |
0.793 |
1.461 |
|
|
1 year |
Moderate improvement of symptoms 50-60% |
32.478 |
1 |
<0.001 |
0.000 |
0.000 |
0.000 |
|
Significant improvement of symptoms 70-80% |
3.519 |
1 |
0.061 |
1.371 |
0.986 |
1.908 |
|
|
Complete improvement of symptoms 90-100% |
0.077 |
1 |
0.782 |
1.047 |
0.758 |
1.445 |
|
|
Beyond 1 year |
Moderate improvement of symptoms 50-60% |
13.988 |
1 |
<0.001 |
0.000 |
0.000 |
0.000 |
|
Significant improvement of symptoms 70-80% |
86.37 |
1 |
<0.001 |
6.850 |
4.411 |
10.637 |
|
|
Complete improvement of symptoms 90-100% |
65.441 |
1 |
<0.001 |
3.837 |
2.749 |
5.356 |
|
pregnancy and their confidence intervals. In pregnancy, the significant difference between the first, second and third visit was for Moderate improvement (OR = 0.052), which further showed that the patient was more likely not to become pregnant. But a significantly higher rate was reported during the one-year visit. During a one-year visit, the odds ratio of pregnancy is the highest for those who have an odds ratio of pregnancy and their confidence intervals. In pregnancy, the significant difference between the first, second and third visit was for Moderate improvement (OR = 0.052), which further showed that the patient was more likely not to become pregnant. But a significantly higher rate was reported during the one-year visit. During a one-year visit, the odds ratio for pregnancy is highest for those who report significant improvement (6,850), but for pregnancy significant improvement was reported (6,850) but pregnancy
Table 6: This table illustrates post-surgical patient’s wellbeing and Quality offline in a table from (n=777).
4. Discussion
Endometriosis has existed for centuries but had a hidden toll. The insignificant attention to the disease has led to the affectation of an estimated population of 176 million women worldwide, about 10% of whom are women in the reproductive age. Endometriosis, the second most common gynecologic disease, has gained the needed attention and momentum only in the past two decades. This study highlighted some of the positive effects of early and timely hysterolaparoscopy in alleviating a patient’s agony and improving QoL. Endometriosis affects women in the prime of their lives and can affect teens and young women who are either in their reproductive or active working age. Because the diagnosis could be delayed, it can affect women’s sexual, social, work, and general life; some even endure a life of constant debilitating pains and infertility [13]. The other reported consequences were broken homes, loss of jobs, and economic burden, all of which can lead to miserable lifestyles of drinking alcohol, smoking cigarettes, and using illicit drugs [1, 20]. The economic burden to individuals and society is enormous [20]. In 2012, an endometriosis survey in the United Kingdom showed that about 1.6 million women were affected, with an estimated financial burden of £10.6 billion. In Australia, approximately 550,000 women were affected, costing £2.75 billion. In the United States, approximately 7.6 million women were affected, with financial implications of about £52.1 billion per year, due to loss of work and healthcare [21, 22]. The accurate prevalence and subsequent economic burden in Hungary remain unknown, although a multicenter study by Bokor A et al estimated a population of approximately 184.223 women affected, with an estimated cost of €1.6 billion per year [23, 24]. Similar to other countries, Hungary has a very complex healthcare system financing. Today, in addition to the public health sector operatives, privately operated healthcare services are becoming very relevant. More so, out of pocket in the healthcare system is very predominant. In this regard, it is difficult to estimate public healthcare financing [25]. Our center is a privately operated hospital that specializes in minimally invasive surgical procedures. The medical and hospital bills, which exclude preoperative investigative costs, are approximately €1.558 and are mainly financed by out of pocket means or by a private insurance policy of the patient. This cost is estimated to be close to almost four times the minimum wage for workers (€460) in the country. The highlighted cost implication shows the level of possible financial stress on patients affected with endometriosis. The estimated financial burden does not include the series of pain regulating medications, consultation, loss of working hours lost due to symptoms, and disease-related complaints.
In this study, the socioeconomic well-being, QoL, and other beneficial effects of expert laparoscopic management of women with endometriosis were evaluated. The combined hysterolaparoscopy enabled thorough and simultaneous evaluation and treatment of other abnormalities that may negatively influence QoL; these abnormalities included bleeding disorders, fibroid cramps, and anatomical deformity that may impair fertility (i.e., subseptum uteri, polyps, Asherman disease, synechia, and adhesions) [26-28]. The mean age of the patients and the duration of diagnosis in this study were similar to those in other studies [24, 29]. Interestingly, the left side of the lower pelvis seemed to be more involved, compared with the right side, probably owing to the intraabdominal fluid circulation pattern, which is in a clockwise direction and stops at the pouch of Douglas at the rectosigmoid level. This fluid that contains cells and tissues and originates from retrograde menstruation, as well other fluids from obstetrics and gynecologic interventions, takes relatively long to settle and digest. This may enhance the possibility of implantation of endometriotic cells or tissues in association with other predisposing factors [18]. Moreover, similar to a study conducted by Flores I et al. and Moammar Al-Jefout et al., this study found a possible direct association of endometriosis with dysmenorrhea, dyspareunia, chronic pelvic pain, and infertility [29–31]. Endometriosis can affect women in several ways; for example, coitus-associated pain could lead to avoidance of intercourse and, ultimately, negatively affect fertility, as shown by other studies [16, 32, 33]. Therefore, the high incidence of dyspareunia (80%) could support the relatively high number of infertility cases (69%). However, during the follow-up period, 9.66% of women opted out of the desire for a child due to various reasons. Similar to a study by Erhong Z et al., this study showed that of the 455 women with infertility, 70.1% had primary infertility and 29.9% had secondary infertility at the end of the follow-up period. After 2 years, 81.3% of patients in all stages of endometriosis became pregnant. In this study, the rate of successful live birth was 94.2%. Similarly, P Kuivasaari et al. reported that the rates of pregnancy and live birth were 81.6% and 43.7%, respectively, in stage I/II endometriosis and 56.7% and 40.3%, respectively, in stage III/IV endometriosis after 1–4 IVF/ICSI treatment cycles [15, 40]. The individualized surgical expertise approach in this center may have influenced the fertility performance in this study. Based on our outcome, the success rate was not significantly influenced by the stage of endometriosis. Moreover, the fertility performance was satisfactory and within an acceptable level; this can lead to an exceptional level of relief of the burden to many families in the society. The other serious challenge faced by women in this study was the presence of pain-related symptoms, such as dysmenorrhea, dyspareunia, dyschezia, dysuria, and abdominal discomfort. Considering the symptoms and complaints of our study population, endometriosis clearly and tremendously lowered the QoL of women; these findings were similar to those reported by Monga et al. and others about QoL, which is relatively low among couples with endometriosis [1, 16, 34].
With regard to the QoL, close to 95% of women had substantial and complete resolution of symptoms at 1 month postoperatively. This outcome was relatively an improvement of the findings in a similar study by Ferrero et al. and in other related studies on the improvement of women’s QoL and sexual performance after laparoscopic surgical treatment for endometriosis [15, 17, 32, 37]. In addition, there was gradual improvement by the sixth month of follow-up, with 96% of women being symptom-free or having significantly improved QoL. Moreover, there was a consistent progressive relief of symptoms, even after the last 12 months of follow-up. The number attached to a particular pain-related symptom directly indicates the degree of improvement after surgery, as illustrated in Table 4. Overall, combined hysterolaparoscopy for the management of endometriosis had remarkable positive effects on the QoL, regardless of stage. Compared with previous studies on the subject matter, we recorded a more remarkable outcome in all indices of a patient’s needs [3, 9, 14, 33]. Given these, radical laparoscopic surgery plays an important role in the treatment of endometriosis, as similarly reported by Mabrouk et al. in 2012 in a study about radical laparoscopic excision of deep infiltrating endometriosis [35]. Similarly, other studies have supported the assertion that laparoscopic treatment of endometriosis significantly relieved women of symptoms, such as dysmenorrhea, dyspareunia, pelvic pain, dyschezia, and dysuria [14, 36].
A relatively similar study was done by Garry et al. on 57 patients with stage III to IV endometriosis and who were analyzed prospectively using Short Form 12 (SF12) and Euro QoL (EQ-5D) questionnaires and were followed-up for 4 months. In 2003, Abbott et al. analyzed 176 women within a longer follow-up period after surgery. In those previous studies, there was a relative improvement in the QoL [37, 38]. In this study, the rate of recurrence with minor challenges was very small at 4.2%. The analysis showed that disease relapse was strictly dependent on the expertise of the surgery. An unanticipated observation was that almost half of the women have previously received other forms of gynecologic intervention before the discovery of the endometriosis. This observation raised questions and indicated a strong suspicion for the likelihood of the association between implantation theory and endometriosis, as shown in Figure 7. Further studies may be required to prove any possible association between these scenarios. Unlike other studies, this study showed that the pattern of localization of endometriosis did not vary according to the geographic location, ethnicity, and socioeconomic status of the patient. Moreover, similar to other studies, this study showed that the most common sites were deep infiltrating rectovaginal septum endometriosis, left ovarian fossa and endometrioma, and right ovarium fossa and endometrioma [19, 32, 39]. Only 10.6% of the women requested for medical treatment a few months after surgery, because of their anticipation for prolonged relapse of the disease but mainly for contraception purposes. The incidence of resectable rectosigmoid deep infiltrating endometriosis was 5.1%, whereas that for deep bladder infiltrating endometriosis that prompted bladder resection was 0.9%. The rate of endometriosis in other sites was 1.0%. Among the women analyzed, none developed endometrioid carcinoma based on the histologic reports [37]. Although laparoscopy is the gold standard for the diagnosis of endometriosis, we cannot overemphasize the value of thorough and critical history taking, physical examination, ultrasound, CT, and MRI in unveiling the diagnosis [1, 2, 14, 40]. In the final analysis, histology examination was performed in all cases to finalize the diagnosis. Staging and classification were based on rAFS (1985) [19, 27, 34]. One of the limitations of this study was its retrospective design. The information derived from the patient’s history was from the hospital database, postsurgery visit reports, and direct electronic communications. The level of suffering before surgery was ascertained by their postsurgery response. Overwhelmingly, although health professionals have placed a relatively high alert on women with chronic pain and other related problems, many studies have shown the importance and benefits of timely and expert laparoscopic management [26, 35, 38]. Further improvement in women’s well-being and QoL may be achieved with the help of combined hysterolaparoscopy [40, 41]. Surgical procedures beyond the scope of the laparoscopy were done, with the aid of hysteroscopy as to address intrauterine pathologies affecting women.
Finally, emphasizing the prevalence of endometriosis and the need for a careful examination of patients with chronic lower abdominal discomfort and/or infertility is essential in today's society and for healthcare providers. Initiation of a broader awareness campaign can provide appropriate support for early combined hysterolaparoscopy, which can reduce prolonged pain and financial stress, improve the quality of life and socio-economic well-being of women with endometriosis.
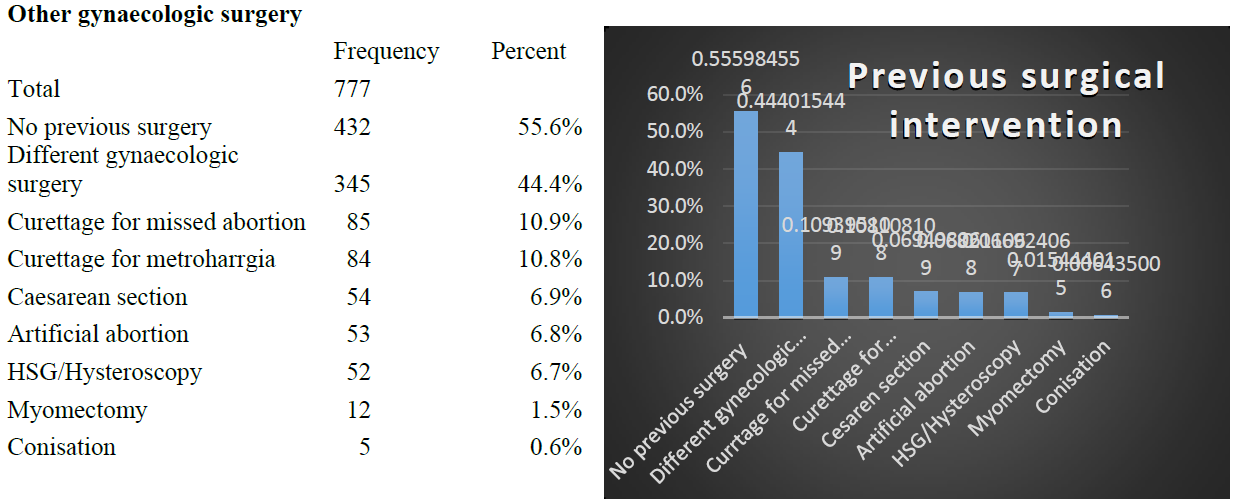
Figure 7: The incidence of other previous gynaecological surgery prior to unset of symptoms in women (n=777).
More than half of the patients (55.6%) had no surgical history, 44.4% had Different gynecologic surgery, 1 in 9 patients (10.9%) had Curettage for missed abortion and Curettage for metroharrgia (10.8%). Caesarean section (6.9%), artificial abortion (6.8%) and HSG / Hysteroscopy (6.7%) were low. Myomectomy and conisation were negligible
Author Contributions
Conceptualization, E.A.A. and K.M.; methodology, F.I., E.A.A.; software, K.Z.; validation, E.A.A., K.M. and F.I.; formal analysis, E.A.A.; investigation, E.A.A.; resources, P.S.; data curation, T.I.; writing—original draft preparation, K.Á.; writing—review and editing, E.A.A.; visualization, K.M.; supervision, K.M.; project administration, K.Á.; funding acquisition, E.A.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
We acknowledge the administrative staff and the hospital’s technical and statistical group, and the general staff of the endoscopic unit and the IVF unit of the hospital for their enormous support in making this article possible.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Nnoaham KE, Hummelshoj L, Webster P, d’Hooghe T, de Cicco Nardone F, de Cicco Nardone C, et al. World Endometriosis Research Foundation Global Study of Women's Health consortium. Impact of endometriosis on quality of life and work productivity: a multicenter study across ten countries. Fertil Steril 96 (2011): 366-373.
- D'Hooghe TM, Mihalyi AM, Simsa P, Kyama CK, Peeraer K, De Loecker P, et al. Why we need a noninvasive diagnostic test for minimal to mild endometriosis with a high sensitivity. Gynecol Obstet Invest 62 (2006): 136-138.
- Pundir J, Omanwa K, Kovoor E, Pundir V, Lancaster G, Barton-Smith P. Laparoscopic excision versus ablation for endometriosis-associated pain: an updated systematic review and meta-analysis. J Minim Invas Gynecol 24 (2017): 747-756.
- Yeung PP, Shwayder J, Pasic RP. Laparoscopic management of endometrisosis: comprehensive review of best evidence. J Minim Invas Gynecol 16 (2009): 269-281.
- Nardo LG, Moustafa M, Beynon DG. Laparoscopic treatment of pelvic pain associated with minimal and mild endometriosis with use of the Helica Thermal Coagulator. Fertil Steril 83 (2005): 735-738.
- Nezhat C, Nezhat F, Nezhat C. Endometriosis: ancient disease, ancient treatments. Fertil Steril 98 (2012): S1-S62.
- Macer ML, Taylor HS. Endometriosis and infertility: a review of the pathogenesis and treatment of endometriosis-associated infertility. Obstet Gynecol Clin North Am 39 (2012): 535-549.
- Nakahara K, Saito H, Saito T, Ito M, Ohta N, Sakai N, et al. Incidence of apoptotic bodies in membrana granulosa of the patients participating in an in vitro fertilization program. Fertil Steril 67 (1997): 302-308.
- Halis G, Mechsner S, Ebert AD. The diagnosis and treatment of deep infiltrating endometriosis. Dtsch Arztebl Int 107 (2010): 446-455.
- Shifren JL, Tseng JF, Zaloudek CJ, Ryan IP, Meng YG, Ferrara N, et al. Ovarian steroid regulation of vascular endothelial growth factor in human endometrium: implication for angiogenesis during the menstrual cycle and in the pathogenesis of endometriosis. J Clin Endocrinol Metab 81 (1996): 3112-3118.
- Pouly JL, Drolet J, Canis M, Boughazine S, Mage G, Bruhat MA, et al. Laparoscopic treatment of symptomatic endometriosis. Hum Reprod 11 (1996): 67-88.
- Sinaii N, Plumb K, Cotton L, Lambert A, Kennedy S, Zondervan K, et al. Differences in characteristics among 1,000 women with endometriosis based on extent of disease. Fertil Steril 89 (2008): 538-545.
- Hadfield R, Mardon H, Barlow D, Kennedy S. Delay in the diagnosis of endometriosis: a survey of women from the USA and the UK. Hum Reprod 11 (1996): 878-880.
- Donnez J, Jadoul P, Donnez O, Squifflet J, Donnez J. Laparoscopic excision of rectovaginal and retrocervical endometriotic lesions. Atlas of operative laparoscopy and hysteroscopy. Informa UK Ltd (2007): 63-75.
- Kuivasaari P, Hippeläinen M, Anttila M, Heinonen S. Effect of endometriosis on IVF/ICSI outcome: stage III/IV endometriosis worsens cumulative pregnancy and live-born rates. Hum Reprod 20 (2005): 3130-3135.
- Monga M, Alexandrescu B, Katz SE, Stein M, Ganiats T. Impact of infertility on quality of life, marital adjustment, and sexual function. Urology 63 (2004): 126-130.
- Ferrero S, Abbamonte LH, Giordano M, Ragni N, Remorgida V. Deep dyspareunia and sex life after laparoscopic excision of endometriosis. Hum Reprod 22 (2006): 1142-1148.
- Levitt DG, Levitt MD. Quantitative modeling of the physiology of ascites in portal hypertension. BMC Gastroenterol 12 (2012): 26.
- Andrews WC, Buttram Jr VC, Behrman SJ, Carmichael E, Cohen MR, Dmowski P, et al. Revised American fertility society classification of endometriosis: 1985. Fertil Steril 43 (1985): 351-352.
- Moradi M, Parker M, Sneddon A, Lopez V, Ellwood D. Impact of endometriosis on women's lives: a qualitative study. BMC Womens Health 14 (2014): 123.
- Helen N. Endometriosis diagnosis survey 2011: Endometriosis UK. Available from: www.endometriosis- org. Registered Charity No. 1035810.
- University College London Hospitals. General Information about Endometriosis. Accessed February (2014).
- Bokor A. Endometriosis prevalence in Hungary. Hungarian Healthcare System–Role of the University. Hospitals. Budapest: Semmelweis University Faculty of Medicine.
- Simoens S, Dunselman G, Dirksen C, Hummelshoj L, Bokor A, Brandes I, et al. The burden of endometriosis: costs and quality of life of women with endometriosis and treated in referral centres. Hum Reprod 27 (2012): 1292-1299.
- World Health Organization. The world health report - health systems financing: the path to universal coverage 2010. Available from: http://www.who.int/whr/2010/en/index.html. Cited May 20 2014, 2010. Geneva: The World Health Organization.
- Fritzer N, Tammaa A, Salzer H, Hudelist G. Effects of surgical excision of endometriosis regarding quality of life and psychological well-being: a review. Womens Health (Lond). Lond: Women's Health 8 (2012): 427-435.
- Seracchioli R, Manuzzi L, Mabrouk M, Solfrini S, Frascà C, Manferrari F, et al. A multidisciplinary, minimally invasive approach for complicated deep infiltrating endometriosis. Fertil Steril 93 (2010): 1007.e1-1007.e3.
- Yap C, Furness S, Farquhar C. Pre and post operative medical therapy for endometriosis Surgery. Cochrane Database Syst Rev 3 (2004): CD003678.
- Flores I, Abreu S, Abac S, Fourquet J, Laboy J, Ríos-Bedoya C. Self-reported prevalence of endometriosis and its symptoms among Puerto Rican women. Int J Gynecol Obstet 100 (2008): 257-261.
- Al-Jefout M, Alnawaiseh N, Yaghi S, Alqaisi A. Prevalence of endometriosis and its symptoms among young Jordanian women with chronic pelvic pain refractory to conventional therapy. J Obstet Gynaecol Can 40 (2018): 165-170.
- Chapron C, Fauconnier A, Dubuisson JB, Barakat H, Vieira M, Bréart G. Deep infiltrating endometriosis: relation between severity of dysmenorrhoea and extent of disease. Hum Reprod 18 (2003): 760-766.
- Tomar GS, Parmar H, Gupta S. Endometriosis in infertility; prevalence, clinical profile, and diagnosis. Int J Med Health Res ISSN 3 (2017): 2454-9142.
- Jia SZ, Leng JH, Shi JH, Sun PR, Lang JH. Health-related quality of life in women with endometriosis: a systematic review. J Ovarian Res 5 (2012): 29.
- Chapron C, Dubuisson JB, Fritel X, Fernandez B, Poncelet C, Béguin S, et al. Operative management of deep endometriosis infiltrating the uterosacral ligaments. J Am Assoc Gynecol Laparosc 6 (1999): 31-37.
- Mabrouk M, Montanari G, Guerrini M, Villa G, Solfrini S, Vicenzi C, et al. Does laparoscopic management of deep infiltrating endometriosis improve quality of life? A prospective study. Health Qual Life Outcomes 9 (2011): 98.
- Sampson JA. Peritoneal endometriosis due to the menstrual dissemination of endometrial tissue into the peritoneal cavity. Am J Obstet Gynecol 14 (1927): 422-469.
- Garry R, Clayton R, Hawe J. The effect of endometriosis and its radical laparoscopic excision on quality of life indicators. BJOG 107 (2000): 44-54.
- Abbott JA, Hawe J, Clayton RD, Garry R. The effects and effectiveness of laparoscopic excision of endometriosis: a prospective study with 2–5 year follow-up. Hum Reprod 18 (2003): 1922-1927.
- Kristensen J, Kjer JJ. Laparoscopic laser resection of rectovaginal pouch and rectovaginal septum endometriosis: the impact on pelvic pain and quality of life. Acta 86 (2007): 1467-1471.
- Zhang E, Zhang Y, Fang L, Li Q, Gu J. Combined hysterolaparoscopy for the diagnosis of female infertility: a retrospective study of 132 patients in China. Mater Sociomed 26 (2014): 156-157.
- Tomassetti C, Geysenbergh B, Meuleman C, Timmerman D, Fieuws S, D’Hooghe External validation of the endometriosis fertility index (EFI) staging system for predicting non-ART pregnancy after endometriosis surgery. Hum Reprod 28 (2013): 1280-1288.


 Impact Factor: * 1.1
Impact Factor: * 1.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 