Treatment of Pelvic Floor Hypertonic Disorders with top Flat Magnetic Stimulation in Women with Vestibulodynia: A Pilot Study
Article Information
Andrea Biondo1, Filippo Murina2, Irene Fusco3*
1Dr. Andrea Biondo’s clinic, gynecologist, Via XX Settembre, 69, Palermo, Italy
2Lower Genital Tract Disease Unit, V. Buzzi Hospital-University of the Study of Milan, Milan, Italy
3University of Florence, Florence, Italy
*Corresponding author: Irene Fusco, University of Florence, Florence, Italy. Tel: +39 3286853105.
Received: 27 May 2022; Accepted: 09 June 2022; Published: 16 June 2022
Citation: Andrea Biondo, Filippo Murina, Irene Fusco. Treatment of Pelvic Floor Hypertonic Disorders with top Flat Magnetic Stimulation in Women with Vestibulodynia: A Pilot Study. Journal of Women’s Health and Development 5 (2022): 175-184
View / Download Pdf Share at FacebookAbstract
Background: Vulvodynia is a popular disease that affects around the 15% of women.
Objectives: In this study we assess the effectiveness and the safeness of a new device that uses Top Flat Magnetic Stimulation for the management of the hypertone in women with vulvodynia.
Methods: PISQ-12 questionnaire for sexual function was used for the evaluation of patient’s vulvodynia improvements. Possible side effects were examined.
Results: In all women examined, the mean score of PISQ-12 significantly decrease from 27,4 (SD 9.6) before treatment session to 15,5 (SD 7.9) after the last session (p < .001), showing an improvement in vulvodynia symptoms. No Side effects were observed.
Conclusion: On the basis of our findings this new technology seems to be able to effectively treat the hypertone condition in vulvodynia disease.
Keywords
Hypertone; Pelvic floor muscle; Top Flat Magnetic Stimulation; Vulvodynia
Hypertone articles Hypertone Research articles Hypertone review articles Hypertone PubMed articles Hypertone PubMed Central articles Hypertone 2023 articles Hypertone 2024 articles Hypertone Scopus articles Hypertone impact factor journals Hypertone Scopus journals Hypertone PubMed journals Hypertone medical journals Hypertone free journals Hypertone best journals Hypertone top journals Hypertone free medical journals Hypertone famous journals Hypertone Google Scholar indexed journals Pelvic floor muscle articles Pelvic floor muscle Research articles Pelvic floor muscle review articles Pelvic floor muscle PubMed articles Pelvic floor muscle PubMed Central articles Pelvic floor muscle 2023 articles Pelvic floor muscle 2024 articles Pelvic floor muscle Scopus articles Pelvic floor muscle impact factor journals Pelvic floor muscle Scopus journals Pelvic floor muscle PubMed journals Pelvic floor muscle medical journals Pelvic floor muscle free journals Pelvic floor muscle best journals Pelvic floor muscle top journals Pelvic floor muscle free medical journals Pelvic floor muscle famous journals Pelvic floor muscle Google Scholar indexed journals Top Flat Magnetic Stimulation articles Top Flat Magnetic Stimulation Research articles Top Flat Magnetic Stimulation review articles Top Flat Magnetic Stimulation PubMed articles Top Flat Magnetic Stimulation PubMed Central articles Top Flat Magnetic Stimulation 2023 articles Top Flat Magnetic Stimulation 2024 articles Top Flat Magnetic Stimulation Scopus articles Top Flat Magnetic Stimulation impact factor journals Top Flat Magnetic Stimulation Scopus journals Top Flat Magnetic Stimulation PubMed journals Top Flat Magnetic Stimulation medical journals Top Flat Magnetic Stimulation free journals Top Flat Magnetic Stimulation best journals Top Flat Magnetic Stimulation top journals Top Flat Magnetic Stimulation free medical journals Top Flat Magnetic Stimulation famous journals Top Flat Magnetic Stimulation Google Scholar indexed journals Vulvodynia articles Vulvodynia Research articles Vulvodynia review articles Vulvodynia PubMed articles Vulvodynia PubMed Central articles Vulvodynia 2023 articles Vulvodynia 2024 articles Vulvodynia Scopus articles Vulvodynia impact factor journals Vulvodynia Scopus journals Vulvodynia PubMed journals Vulvodynia medical journals Vulvodynia free journals Vulvodynia best journals Vulvodynia top journals Vulvodynia free medical journals Vulvodynia famous journals Vulvodynia Google Scholar indexed journals infections articles infections Research articles infections review articles infections PubMed articles infections PubMed Central articles infections 2023 articles infections 2024 articles infections Scopus articles infections impact factor journals infections Scopus journals infections PubMed journals infections medical journals infections free journals infections best journals infections top journals infections free medical journals infections famous journals infections Google Scholar indexed journals vulvar dermatosis articles vulvar dermatosis Research articles vulvar dermatosis review articles vulvar dermatosis PubMed articles vulvar dermatosis PubMed Central articles vulvar dermatosis 2023 articles vulvar dermatosis 2024 articles vulvar dermatosis Scopus articles vulvar dermatosis impact factor journals vulvar dermatosis Scopus journals vulvar dermatosis PubMed journals vulvar dermatosis medical journals vulvar dermatosis free journals vulvar dermatosis best journals vulvar dermatosis top journals vulvar dermatosis free medical journals vulvar dermatosis famous journals vulvar dermatosis Google Scholar indexed journals painful intercourse articles painful intercourse Research articles painful intercourse review articles painful intercourse PubMed articles painful intercourse PubMed Central articles painful intercourse 2023 articles painful intercourse 2024 articles painful intercourse Scopus articles painful intercourse impact factor journals painful intercourse Scopus journals painful intercourse PubMed journals painful intercourse medical journals painful intercourse free journals painful intercourse best journals painful intercourse top journals painful intercourse free medical journals painful intercourse famous journals painful intercourse Google Scholar indexed journals dyspareunia articles dyspareunia Research articles dyspareunia review articles dyspareunia PubMed articles dyspareunia PubMed Central articles dyspareunia 2023 articles dyspareunia 2024 articles dyspareunia Scopus articles dyspareunia impact factor journals dyspareunia Scopus journals dyspareunia PubMed journals dyspareunia medical journals dyspareunia free journals dyspareunia best journals dyspareunia top journals dyspareunia free medical journals dyspareunia famous journals dyspareunia Google Scholar indexed journals neuropathic articles neuropathic Research articles neuropathic review articles neuropathic PubMed articles neuropathic PubMed Central articles neuropathic 2023 articles neuropathic 2024 articles neuropathic Scopus articles neuropathic impact factor journals neuropathic Scopus journals neuropathic PubMed journals neuropathic medical journals neuropathic free journals neuropathic best journals neuropathic top journals neuropathic free medical journals neuropathic famous journals neuropathic Google Scholar indexed journals polymorphisms articles polymorphisms Research articles polymorphisms review articles polymorphisms PubMed articles polymorphisms PubMed Central articles polymorphisms 2023 articles polymorphisms 2024 articles polymorphisms Scopus articles polymorphisms impact factor journals polymorphisms Scopus journals polymorphisms PubMed journals polymorphisms medical journals polymorphisms free journals polymorphisms best journals polymorphisms top journals polymorphisms free medical journals polymorphisms famous journals polymorphisms Google Scholar indexed journals
Article Details
1. Introduction
Vulvodynia represents a chronic pain syndrome affecting 12-15% of women in population based epidemiological studies [1]. Vulvar pain was divided into two categories by the 2015 Consensus and Terminology and Classification of Persistent Vulvar Pain and Vulvodynia [2]. The first one comprehends vulvar pain that is caused by a specific clearly recognizable disorder (e.g., infections or vulvar dermatosis). The second one comprehends vulvar pain that lasts at least 3 months and a specific cause cannot be clearly identified. The most recurrent manifestation of the disease (about 80%) is localized provoked vulvodynia at the vestibule, known as Vestibulodynia (VBD) [3]. Women with VBD often describe vulvar pain as a dyspareunia (difficult or painful intercourse), stinging, burning, rawness and irritation. Many women with VBD affirm that the vestibular area is touch sensitive and that the pain would increase from rubbing. They define their pain as “itching”, “burning” or “hot”. The responses pattern of VBD is indicative of sensory anomalies in the form of evoked pain, such us allodynia or hyperalgesia, suggesting sensitization, a neuropathic pain underlying manifestation [4]. Moreover, the discomfort caused by VBD is always associated with muscle hyperactivity of the pelvic floor [5]. This prolonged pattern can result in dysfunctional muscle hyperactivity, a tissue perfusion reduction, and a myofascial trigger points development, resulting in radiated or localized pain and / or intense tenderness. In the development and course of VBDU, factors such as hormonal disturbances, infections, neuroinflammation, gene polymorphisms or atopic disease, which interfere with psychogenic factors and inflammation, have been associated [6]. The great difficulty in identifying any type of "gold standard" treatment for VBD is that it is probably not a disease but rather a collection of different diseases, in which the common endpoint is pelvic floor hypertonic dysfunction and vestibular hypersensitivity. In case of nonresponses’ patients at the beginning of the treatment, a team of different health professionals, such as gynaecologists, physiotherapists and / or psychologists, dermatologists or sex therapists, may be needed to treat the complicated aspects of vulvodynia [7]. The recommended guidelines for the treatment of vulvodynia are mainly based on a restricted number of placebo-controlled Randomized Clinical Trials (RCTs), case series and expert opinion. A phased approach of modalities that address neural sensitization, pelvic floor dysfunction and psychosexual wholesomeness is suggested for the treatment of vulvodynia. There is significant evidence that Pelvic Floor Muscle (PFM) disorder is a relevant target of VBD treatment. Pelvic Floor Physical Therapy (PFPT) is able to improve proprioception, relaxation and muscle tone, aiming to rehabilitate the pelvic floor muscles. PFPT includes various techniques which can be provided alone or in combination; Among these manual therapy and EMG biofeedback represent the most common. A coherent effectiveness of PFPT was found in a systematic review concerning the treatment of VBD, which reveal in 71–80% of women, a significant improvement in pain. Notwithstanding, many patients can have some difficulties to apply PFPT for the severe introital pain, at least in the initial stages of treatment. Over the last few years, magnetic stimulation has been studied as an alternative treatment to electrical stimulation for urological diseases, clinical neuro-diagnostic applications and for the pelvic floor muscle Strengthening/ Pain/ Hypertonia as a safe and non-invasive method for chronic pelvic pain syndrome [9-14]. The purpose of this research was to evaluate the effectiveness and the safeness of a new device that uses Top Flat Magnetic Stimulation for vulvodynia management.
2. Materials and Methods
Subjects were suitable for this study if they were at least 18 years of age and with a VBD and moderate /severe hypertonic pelvic floor dysfunction diagnosis. The hypertonic pelvic floor diagnosis needed to be established by a physical exam documenting hypertonus of the levator ani complex by an experienced examiner. Furthermore, suitable individuals did not exhibit any other specific neurological diseases, pelvic organ prolapses, genital infections and were not in pregnancy or in menopausal status. Persons with pacemakers or metal implants were also excluded. All patients released a written informed consent and Institutional Review Board approval for the study was obtained. Procedures were performed using a non-invasive electromagnetic therapeutic device (DR ARNOLD, DEKA M.E.L.A. Calenzano, Italy) equipped with a main unit and a chair applicator planned for deep pelvic floor area therapy. DR ARNOLD can generate an electromagnetic field with a homogenous profile (TOP FMS-TOP Flat Magnetic Stimulation) optimised for the stimulation of pelvic area. At the initial stages of treatment, before each session, a gynaecologist or a trained operator set and adjusted the patient's position; patient's perineum is positioned in the center of the seat where the coil is placed to ensure a proper intensity of stimulation and to achieve a muscle contractions uniform distribution. With the use of subject device, the muscle work at the same intensity in all the area considered. A correct patient’s chair positioning is a key treatment aspect: first, it ensures patient comfort during the long-term treatment session and secondly, it allows the electromagnetic field to be centred on the patient's perineum. As showed in Figure 1, patient’s legs are perpendicularly flexed, thighs are parallel to the floor and feet are flat on the ground. According to the purposes of the treatment, the subject system is equipped with protocols for the hypertone reduction, which use mild stimulations (low frequency around 10 Hz) or high intensity and higher frequency contractions in order to improve patient’s pelvic floor tone. The intensities used during each treatment sessions reached up to 55-60%. All patients underwent to a total of 10 treatments with DR ARNOLD system. Sessions were performed twice a week for 5 consecutive weeks; each session lasted 28 minutes depending on the patient’s muscular condition. During the first couple of minutes all patients underwent a warm-up phase and the Overtone/Pain protocol (muscle work aimed to muscle inhibition a reduction of pain) was selected. Data were gathered at baseline and 45 days after the last treatment session. VBD was evaluated using the Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire (PISQ-12) [15] (see Appendix A). The PISQ-12 is a short-form of the PISQ-31 measure [16] and represents a measure of sexual function. The three domains of the PISQ-12 are: behavioural-emotive (items 1-4), physical (items 5-9) and partner-related (items 10-12). Answers are rated on a five-point Likert scale that range from 0 (always) to 4 (never) [17]; higher scores indicate improved sexual function. In this study PISQ-12’s questions number 7 and 8 were excluded as they concern urinary incontinence and prolapse of the genital organs which are included in the study exclusion criteria. For statistical analyses SPSS (IBM Corp., New York, USA) was used. Student t test was used for descriptive statistical analysis (means and ±SDs). A p< .05 is significant.

Figure 1: Representation of the correct patient’s position on DR ARNOLD’s chair. Courtesy of DEKA M.E.L.A company.
|
Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire (PISQ-12) |
|
|
Questions |
Response options |
|
Q1. How frequently do you feel sexual desire? This feeling may include wanting to have sex, planning to have sex feeling frustrated due to lack of sex, etc. |
0= Always |
|
1= Usually |
|
|
2= Sometimes |
|
|
3= Seldom |
|
|
4= Never |
|
|
Q2. Do you climax (have an orgasm) when having sexual intercourse with your partner? |
0= Always |
|
1= Usually |
|
|
2= Sometimes |
|
|
3= Seldom |
|
|
4= Never |
|
|
Q3. Do you feel sexually excited (turned on) when having sexual activity with your partner? |
0= Always |
|
1= Usually |
|
|
2= Sometimes |
|
|
3= Seldom |
|
|
4= Never |
|
|
Q4. How satisfied are you with the variety of sexual activities in your current sex life? |
0= Always |
|
1= Usually |
|
|
2= Sometimes |
|
|
3= Seldom |
|
|
4= Never |
|
|
Q5. Do you feel pain during sexual intercourse? |
0= Always |
|
1= Usually |
|
|
2= Sometimes |
|
|
3= Seldom |
|
|
4= Never |
|
|
Q6. Are you incontinent of urine (leak urine) with sexual activity? |
0= Always |
|
1= Usually |
|
|
2= Sometimes |
|
|
3= Seldom |
|
|
4= Never |
|
|
Q7. Does fear of incontinence (either stool or urine) restrict your sexual activity? |
0= Always |
|
1= Usually |
|
|
2= Sometimes |
|
|
3= Seldom |
|
|
4= Never |
|
|
Q8. Do you avoid sexual intercourse because of bulging in the vagina (either the bladder,rectum or vagina falling out?)? |
0= Always |
|
1= Usually |
|
|
2= Sometimes |
|
|
3= Seldom |
|
|
4= Never |
|
|
Q9. When you have sex with your partner, do you have negative emotional reactions such as fear, disgust, shame or guilt? |
0= Always |
|
1= Usually |
|
|
2= Sometimes |
|
|
3= Seldom |
|
|
4= Never |
|
|
Q10. Does your partner have a problem with erections that affects your sexual activity? |
0= Always |
|
1= Usually |
|
|
2= Sometimes |
|
|
3= Seldom |
|
|
4= Never |
|
|
Q11. Does your partner have a problem with premature ejaculation that affects your sexual activity? |
0= Always |
|
1= Usually |
|
|
2= Sometimes |
|
|
3= Seldom |
|
|
4= Never |
|
|
Q12. Compared to orgasms you have had in the past, how intense are the orgasms you have had in the past six months? |
0= Much less intense |
|
1= Less intense |
|
|
2= Same Intensity |
|
|
3= More intense |
|
|
4= Much more intense |
|
Appendix A
3. Results
Of 34 women meeting the inclusion criteria of the study (age mean 38.3 ± 11.9 years), all agreed to participate in the study, and no patients were lost to follow-up. Subjects showed PISQ-12 mean values significantly lower than the controls (p <.001). In all patients examined, the mean score of PISQ-12 significantly decrease from 27.4 (SD ±9.6) at baseline to 15.5 (SD 7.9), 45 days after the last treatment session (Table 1 and Figure 2).
|
Before Mean ±SD |
Post Mean ±SD |
Significance |
|
|
PISQ-12 Mean Score |
27.4±9.6 |
15.5±7.9 |
p<0,001 |
Table 1: Mean score of PISQ-12 evaluated before any treatment session and at 45 days after the last treatment session.
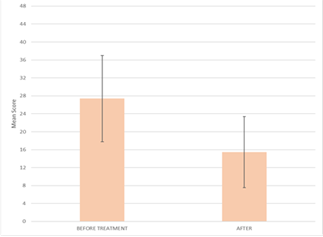
Figure 2: Histogram representation of PISQ-12 mean score evaluated before any treatment session and at 45 days after the last treatment session.
|
PISQ-12 domains |
Before |
Post |
|
Mean ±SD |
Mean ±SD |
|
|
Behavioral-emotive (items 1-4) |
10.4±4.6 |
5.9±3.8 |
|
Physical (items 5-9) |
12.4±3.9 |
6.5±3.1 |
|
Partner-Related (items 10-12) |
4.6±1.9 |
3.1±1.7 |
Table 2: Mean score of PISQ-12 three domains: behavioral-emotive (items 1 – 4), physical (items 5– 9) and partner-related (items 10 – 12), evaluated before any treatment session and at 45 days after the last treatment session.
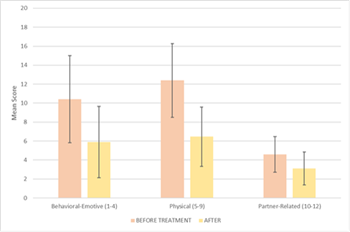
Figure 3: Histogram representation of PISQ-12 three domains: behavioral-emotive (items 1-4), physical (items 5-9) and partner-related (items 10-12), evaluated before any treatment session and at 45 days after the last treatment session.
As shown in Table 2 and Figure 3, each mean score variations of PISQ-12’s domains, evaluated before any treatment session and 45 days after the last treatment session, showed interesting and promising results: behavioral-emotive domain mean score decreases from 10.4 (SD 4.6) to 5.9 (SD 3.8), physical domain mean score decreases from 12.4 (SD 3.9) to 6.5 (SD 3.1), while partner-Related domain mean score decreases from 4.6 (SD ±1.9) to 3.1 (SD ±1.7). No adverse effects related to the treatment were observed.
4. Discussion
For all study subjects treated with electromagnetic therapeutic device DR ARNOLD, we observed that patients reported significantly improvement of vulvar pain as resulting of PISQ-12’s domains changes. The magnetic stimulator technology works by exerting a deep stimulation of the pelvic floor musculature and a recovery of neuromuscular control18. According to the scientific literature19-26 this technology can safely and effectively treat stress, urge and mixed urinary incontinence by pelvic floor muscle strengthening in a variety of patients. The device used in our study has also a specific protocol for muscle hypertonicity, making it suitable for the pelvic floor muscle dysfunction, with increased tone and difficulty in controlling and contracting the muscles that characterize the patients with VBD. Indeed, the overtone/pain protocol for hypertonic management uses lower frequencies (around 10 Hz) creating a homogeneous distribution of the electromagnetic field that does not create regions of different stimulation intensity avoiding an overstimulation of the already hypersensitive receptors and sensory nerves typical of vulvodynia condition. Another strength of this technology lies in the gradually increasing intensity of the electromagnetic fields and in the frequency of the impulses, which translate into a unique feature of the contractions. The goal of PFPT is to rehabilitate the correct function of tissues and the PFM, leading to a reduction of neural tension and vulvovaginal pain. In some instances, there is an improvement of patient’s sexual function. Many studies suggest a global multimode approach to PFPT, including the manual (stretching, massage, and myofascial trigger points) and assisted therapies (e.g. electromyographic biofeedback and vaginal dilators). Several studies show that greater number of women report significant intercourse pain improvements and sexual functioning following of multimodal PFPT. However, these approaches are operator-dependent and can be time-consuming with a potential limited compliance for many patients. For the above reasons, compared to the panorama of devices for the pelvic floor rehabilitation, our device introduces some important advantages: to stimulate the muscles, it does not need the use of a probe and thanks to the progressively proper emission of supplied energy, it allows patients to remain fully clothed in an ergonomic and comfortable seat. Finally, DR ARNOLD may be defined as an "educator" system as it makes the patient perceive the relaxation of the muscles involved in the treatment, making them acquire a greater awareness and autonomy to choose when to repeat the next treatment session. This new technology can also be combined with other pharmacological or physical methods [27]. Our future goal will be to increase the number of patient’s to better validate this innovative and non-invasive treatment modality for difficult pathologies such as that of vulvodynia. While the results of this study appear promising, it has several limitations. Firstly, the study was not controlled therefore introducing bias. Further limitations include the small patient numbers studied, and the relatively short duration of the follow-up of 45 days. Based on our findings this new technology seems to be able to effectively treat the PFM hypertonic dysfunction in VBD with a therapeutic program that must be personalized for each patient.
Funding
no external funding was provided.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data that support the study findings are available on request from the corresponding author.
Conflicts of Interest
no conflict of interest to declare.
Author Contributions
Conceptualization, F.M.; methodology, A.B; software, A.B; validation, A.B and F.M; formal analysis, A.B; investigation, F.M and A.B; resources, A.B; data curation, I.F and F.M; writing—original draft preparation, F.M.; writing-review and editing, F.M and I.F; visualization, A.B, I.F and F.M.; supervision, A.B, F.M and I.F ; project administration A.B ; funding acquisition, A.B; All authors have read and agreed to the published version of the manuscript.
References
- Bergeron S, Reed BD, Wesselmann U, et al. Vulvodynia. Review Nat Rev Dis Primers 6 (2020): 36.
- Edwards L. Vulvodynia. Review Clin Obstet Gynecol 58 (2015): 143-152.
- Graziottin A, Murina F, Gambini D, et al. Vulvar pain: The revealing scenario of leading comorbidities in 1183 cases. Eur J Obstet Gynecol Reprod Biol 252 (2020): 50-55.
- Murina F, Bianco V, Radici G, et al. Electrodiagnostic Functional Sensory Evaluation of Patients With Generalized Vulvodynia: A Pilot Study. J Low Genit Tract Dis 14 (2010): 221-224.
- Backman H, Widenbrant M, Bohm-Starke N, et al. Combined physical and psychosexual therapy for provoked vestibulodynia-an evaluation of a multidisciplinary treatment model. J Sex Res 45 (2008): 378-385.
- Dionisi B, Anglana F, Inghirami P, et al. Use of transcutaneous electrical stimulation and biofeedback for the treatment of vulvodynia (vulvar vestibular syndrome): result of 3 years of experience. Comparative Study Minerva Ginecol 60 (2008): 485-491.
- Davenport RB, Voutier CR, Veysey EC. Outcome Measurement Instruments for Provoked Vulvodynia: A Systematic Review. Review J Low Genit Tract Dis 22 (2018): 396-404.
- BJ Loflin, Westmoreland K, Williams TN. Vulvodynia: A Review of the Literature. J Pharm Technol 35 (2019): 11-24.
- Ghisu GP. Vulvodynia. Diagnostics and Management Strategies. D Praxis (Bern 1994). 108 (2019): 685-691.
- Waldinger MD, de Lint GJ, Venema PL, et al. Successful transcutaneous electrical nerve stimulation in two women with restless genital syndrome: the role of adelta- and C-nerve fibers Case. Reports J Sex Med 7 (2010): 1190-1199.
- Murina F, Felice R, Di Francesco S, et al. Vaginal diazepam plus transcutaneous electrical nerve stimulation to treat vestibulodynia: A randomized controlled trial. Eur J Obstet Gynecol Reprod Biol 228 (2018): 148-153.
- Galloway NT, El-Galley RE, Sand PK, et al. Extracorporeal magnetic innervation therapy for stress urinary incontinence. Clinical Trial Urology 53 (1999): 1108-1111.
- Yamanishi T, Sakakibara R, Uchiyama T, et al. Comparative study of the effects of magnetic versus electrical stimulation on inhibition of detrusor overactivity. Clinical Trial Urology 56 (2000): 777-781.
- Rowe E, Smith C, Laverick L, et al. A prospective, randomized, placebo controlled, double-blind study of pelvic electromagnetic therapy for the treatment of chronic pelvic pain syndrome with 1 year of followup. Clinical Trial J Urol 173 (2005): 2044-2047.
- Rogers RG, Coates KW, Kammerer-Doak D, et al. A short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12). Int Urogynecol J Pelvic Floor Dysfunct 14 (2003): 164-168
- Rogers RG, Kammerer-Doak D, Villarreal A, et al. A new instrument to measure sexual function in women with urinary incontinence or pelvic organ prolapse. Am J Obstet Gynecol 184 (2001): 552-558.
- Rogers RG, Coates KW, Kammerer-Doak D, et al. A short form of the pelvic organ Prolapse/Urinary incontinence sexual questionnaire (PISQ-12) Int Urogynecol J 15 (2004): 219.
- Yamanishi T, Suzuki T, Sato R, et al. Effects of magnetic stimulation on urodynamic stress incontinence refractory to pelvic floor muscle training in a randomized sham-controlled study. Randomized Controlled Trial Low Urin Tract Symptoms 11 (2019): 61-65.
- Yokoyama T, Fujita O, Nishiguchi J, et al. Extracorporeal magnetic innervation treatment for urinary incontinence. Clinical Trial Int J Urol 11 (2004): 602-606.
- Gilling PJ, Wilson LC, Westenberg AM, et al. A double-blind randomized controlled trial of electromagnetic stimulation of the pelvic ?oor vs sham therapy in the treatment of women with stress urinary incontinence. Randomized Controlled Trial BJU Int 103 (2009): 1386-1390.
- Unsal A, Saglam R, Cimentepe E. Extracorporeal magnetic stimulation for the treatment of stress and urge incontinence in women--results of 1-year follow-up. Comparative Study Scand J Urol Nephrol 37 (2003): 424-448.
- Yokoyama T, Inoue M, Fujita O, et al. Preliminary results of the effect of extracorporeal magnetic stimulation on urinary incontinence after radical prostatectomy: a pilot study. Comparative Study Urol Int 74 (2005): 224-228.
- Choe JH, Choo M-S, Lee K-S. Symptom change in women with overactive bladder after extracorporeal magnetic stimulation: a prospective trial. Clinical Trial Int Urogynecol J Pelvic Floor Dysfunct 18 (2007): 875-880.
- Vadalà M, Palmieri B, Malagoli A, et al. High-power Magnetotherapy: A New Weapon in Urinary Incontinence?. Observational Study Low Urin Tract Symptoms 10 (2018): 266-270.
- Chandi DD, Groenendijk PM, Venema PL. Functional extracorporeal magnetic stimulation as a treatment for female urinary incontinence: 'the chair'. BJU Int 93 (2004): 539-542.
- Cidranes D, Blanco E. Safety And Preliminary Efficacy of Magnetic Stimulation of Pelvic Floor with Hifem Technology in Urinary Incontinence. Medical & Clinical Research 3 (2018): 2577-2800.
- Rosen NO, Dawson SJ, Brooks M, et al. Treatment of Vulvodynia: Pharmacological and Non-Pharmacological Approaches. Review Drugs 79 (2019): 483-493.


 Impact Factor: * 1.1
Impact Factor: * 1.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 