Transitional Cell Carcinoma: Impact of Life Style on Grading of Tumor
Article Information
Md. Mashiur Arefin1, Homayra Tahseen Hossain2
1Assistant Professor, Department of Urology, Rajshahi Medical College, Rajshahi, Bangladesh
2Associate Professor, Department of Medicine, Popular Medical College, Dhaka, Bangladesh
*Corresponding Author: Department of Urology, Rajshahi Medical College, Rajshahi, Bangladesh
Received: 14 June 2023; Accepted: 27 June 2023; Published: 13 July 2023
Citation: Md. Mashiur Arefin, Homayra Tahseen Hossain. Transitional Cell Carcinoma: Impact of Life Style on Grading of Tumor. Journal of Cancer Science and Clinical Therapeutics. 7 (2023): 141-145.
View / Download Pdf Share at FacebookAbstract
Background: Transitional cell carcinoma (TCC) is a common type of bladder cancer, predominantly affecting males exposed to certain chemical products and is strongly associated with tobacco consumption. Understanding the clinicopathological correlation and tumor grading in TCC is essential for effective management and prognosis.
Objective: This study is to examine the correlation between the impact of lifestyle and tumor grading in Transitional cell carcinoma (TCC).
Methods: A descriptive and cross-sectional retrospective study was conducted at Rajshahi Medical College Hospital, Bangladesh. A total of 144 cases of histologically confirmed TCC diagnosed between January 2019 and January 2021 were included. Patient records from the Department of Urology was analyzed, including demographic data, tobacco consumption, symptoms, and organ involvement. Tumour grading was assessed based on histopathological analysis.
Results: The majority of TCC cases were found in males (77.8%) compared to females (22.2%). Tobacco consumption was strongly associated with TCC, with a rate of 68.8%. Tumour grading revealed that 59% of cases were classified as low grades, while 41% were classified as high grades. High-grade TCC was more prevalent in males aged 50 to 69 years, particularly among smokers residing in rural areas engaged in cultivation.
Conclusion: This study provides insights into the clinicopathological characteristics of TCC, emphasizing the association with tobacco consumption and the predominance of high-grade tumours in specific demographic groups. These findings contribute to the understanding of TCC and may aid in the development of targeted prevention and treatment strategies for better patient outcomes. Further research is warranted to explore additional factors influencing TCC development and progression.
Keywords
Transitional cell carcinoma, urothelial cancer, lifestyle, grading, correlation
Transitional cell carcinoma articles, urothelial cancer articles, lifestyle articles, grading articles, correlation articles
Transitional cell carcinoma articles Transitional cell carcinoma Research articles Transitional cell carcinoma review articles Transitional cell carcinoma PubMed articles Transitional cell carcinoma PubMed Central articles Transitional cell carcinoma 2023 articles Transitional cell carcinoma 2024 articles Transitional cell carcinoma Scopus articles Transitional cell carcinoma impact factor journals Transitional cell carcinoma Scopus journals Transitional cell carcinoma PubMed journals Transitional cell carcinoma medical journals Transitional cell carcinoma free journals Transitional cell carcinoma best journals Transitional cell carcinoma top journals Transitional cell carcinoma free medical journals Transitional cell carcinoma famous journals Transitional cell carcinoma Google Scholar indexed journals urothelial cancer articles urothelial cancer Research articles urothelial cancer review articles urothelial cancer PubMed articles urothelial cancer PubMed Central articles urothelial cancer 2023 articles urothelial cancer 2024 articles urothelial cancer Scopus articles urothelial cancer impact factor journals urothelial cancer Scopus journals urothelial cancer PubMed journals urothelial cancer medical journals urothelial cancer free journals urothelial cancer best journals urothelial cancer top journals urothelial cancer free medical journals urothelial cancer famous journals urothelial cancer Google Scholar indexed journals lifestyle articles lifestyle Research articles lifestyle review articles lifestyle PubMed articles lifestyle PubMed Central articles lifestyle 2023 articles lifestyle 2024 articles lifestyle Scopus articles lifestyle impact factor journals lifestyle Scopus journals lifestyle PubMed journals lifestyle medical journals lifestyle free journals lifestyle best journals lifestyle top journals lifestyle free medical journals lifestyle famous journals lifestyle Google Scholar indexed journals grading articles grading Research articles grading review articles grading PubMed articles grading PubMed Central articles grading 2023 articles grading 2024 articles grading Scopus articles grading impact factor journals grading Scopus journals grading PubMed journals grading medical journals grading free journals grading best journals grading top journals grading free medical journals grading famous journals grading Google Scholar indexed journals correlation articles correlation Research articles correlation review articles correlation PubMed articles correlation PubMed Central articles correlation 2023 articles correlation 2024 articles correlation Scopus articles correlation impact factor journals correlation Scopus journals correlation PubMed journals correlation medical journals correlation free journals correlation best journals correlation top journals correlation free medical journals correlation famous journals correlation Google Scholar indexed journals malignant tumor articles malignant tumor Research articles malignant tumor review articles malignant tumor PubMed articles malignant tumor PubMed Central articles malignant tumor 2023 articles malignant tumor 2024 articles malignant tumor Scopus articles malignant tumor impact factor journals malignant tumor Scopus journals malignant tumor PubMed journals malignant tumor medical journals malignant tumor free journals malignant tumor best journals malignant tumor top journals malignant tumor free medical journals malignant tumor famous journals malignant tumor Google Scholar indexed journals epithelial cells articles epithelial cells Research articles epithelial cells review articles epithelial cells PubMed articles epithelial cells PubMed Central articles epithelial cells 2023 articles epithelial cells 2024 articles epithelial cells Scopus articles epithelial cells impact factor journals epithelial cells Scopus journals epithelial cells PubMed journals epithelial cells medical journals epithelial cells free journals epithelial cells best journals epithelial cells top journals epithelial cells free medical journals epithelial cells famous journals epithelial cells Google Scholar indexed journals histopathological analysis articles histopathological analysis Research articles histopathological analysis review articles histopathological analysis PubMed articles histopathological analysis PubMed Central articles histopathological analysis 2023 articles histopathological analysis 2024 articles histopathological analysis Scopus articles histopathological analysis impact factor journals histopathological analysis Scopus journals histopathological analysis PubMed journals histopathological analysis medical journals histopathological analysis free journals histopathological analysis best journals histopathological analysis top journals histopathological analysis free medical journals histopathological analysis famous journals histopathological analysis Google Scholar indexed journals prostate cancers articles prostate cancers Research articles prostate cancers review articles prostate cancers PubMed articles prostate cancers PubMed Central articles prostate cancers 2023 articles prostate cancers 2024 articles prostate cancers Scopus articles prostate cancers impact factor journals prostate cancers Scopus journals prostate cancers PubMed journals prostate cancers medical journals prostate cancers free journals prostate cancers best journals prostate cancers top journals prostate cancers free medical journals prostate cancers famous journals prostate cancers Google Scholar indexed journals adenocarcinoma articles adenocarcinoma Research articles adenocarcinoma review articles adenocarcinoma PubMed articles adenocarcinoma PubMed Central articles adenocarcinoma 2023 articles adenocarcinoma 2024 articles adenocarcinoma Scopus articles adenocarcinoma impact factor journals adenocarcinoma Scopus journals adenocarcinoma PubMed journals adenocarcinoma medical journals adenocarcinoma free journals adenocarcinoma best journals adenocarcinoma top journals adenocarcinoma free medical journals adenocarcinoma famous journals adenocarcinoma Google Scholar indexed journals
Article Details
1. Introduction
Transitional cell carcinoma is a malignant tumor arising from transitional epithelial cells that line the urinary bladder [1]. Urothelial cancer is the 10th most common cancer and 2nd most common cancer among urological cancer worldwide, with approximately over 549,393 new cases and 199922 death per year [2]. The incidence of bladder cancer is more in men than women and approximately three-fourths of sufferers are male [3]. Bladder cancer strikes one in five persons worldwide before they are 75 years of age. It is estimated that the worldwide prevalence of this condition ranges from 1 in 10 in South and Central Asia and Middle Africa to 1 in 2.5 in Australia and New Zealand [4]. Ninety percent of all occurrences of bladder cancer are due to Transitional cell carcinoma (TCC), whereas only 5% are due to squamous cell carcinoma, and the remaining 5% include rare subtypes such as adenocarcinoma, sarcoma, and metastatic urothelial cancer [5]. It is very difficult to compare the data of underdeveloped nations that do not have functional cancer registries with developed countries with excellent technological support systems and functional cancer registries [6, 7]. So, the frequency of urological cancers shows significant variations in different parts of the world [8]. Kidney and bladder cancers show a statically significant positive association with socio-economic deprivation, on the other hand, prostate and testicular cancers show an opposite relationship [9]. Kidney and bladder cancers had a higher incidence rate in rural areas, while prostate cancers are higher in metro areas [10]. WHO classifies urothelial carcinoma as low-grade urothelial carcinoma (LGUC) and high-grade urothelial carcinoma (HGUC) based on its cell morphology and histological structure [3, 11]. Transitional cell carcinoma is strongly associated with tobacco consumption about 50-65% of all cases [5]. Other risk factors are exposure to polycyclic aromatic hydrocarbons, benzene products, phenacetin, certain chemotherapeutic agents like cyclophosphamide and similar products. The association is not clear but it’s implicated with Caffeine and artificial sweeteners [12]. 75% of urothelial bladder cancer is confined to the mucosa (non-muscle invasive bladder cancer: NMIBCa) and 25-30% are muscle invasive (muscle-invasive bladder cancer: MIBCa) at diagnosis [13].
Transurethral resection of the bladder tumour (TURBT) is the treatment of choice for NMIBCa and radical cystectomy is the choice for MIBCa and high-grade tumours. To prevent progression and recurrence, intravesical installations of chemotherapeutic agents or BCG along with TURBT are a choice. Despite the improvement of surgical and perioperative agents, long-term survival rates remained unchanged [13].
2. Materials and Methods
This descriptive and cross-sectional retrospective study focused on histologically proven cases of Transitional cell carcinoma (TCC) within urological malignancies at Rajshahi Medical College Hospital (RMCH) from January 2019 to January 2021. Patient records pertaining to the diagnosis of TCC in the urogenital system were retrieved from the Department of Urology at RMCH. Patient biodata, including age, sex, habits, symptoms, and affected organs, were extracted and analyzed. Statistical analysis was conducted using STATA 14. The study utilized anonymized data for statistical analysis, thereby waiving the need for patient consent regarding ethical considerations.
3. Results
During our study, we collected a total of 144 cases of Transitional cell carcinoma in the Department of Urology at Rajshahi medical college, Bangladesh, diagnosed by histopathology. The sex distribution of these cancers was male (112) 77.8% and female (32) 22.2%. The association between tobacco consumption and transitional cell carcinoma is very high (tobacco consumption rate 68.8%). In the case of TCC, the low grade is 85(59%) and the high grade is 59(41%) and males are more common (77.8%). Among all the TCC, upper tract TCC was seven in numbers and urethral was three, high-grade TCC is more common in male patients at age of 50 to 69 years who are smokers and reside in rural areas and cultivators. Male suffers more from high-grade tumour (46.4%) than female (21.9%). The mean age of a high-grade tumour is 59.5 years with a Creatinine level of 1.4 and haemoglobin is 10.5 gm/dl. The mean age of low-grade tumours is 65.5 years with a Creatinine level of 1.2 and haemoglobin is 10.6 gm/dl.
|
Sex |
High grade |
Low grade |
Total |
Total |
|
No.% |
No.% |
No. |
% |
|
|
Female |
7(11.9%) |
25(29.4%) |
32 |
22.2% |
|
Male |
52(88.1%) |
60(70.6%) |
112 |
77.8% |
|
Total |
59(100%) |
85(100%) |
144 |
100% |
Pearson chi2(1) =6.2042 pr =0.013
Table 1: Grading of TCC among populations.
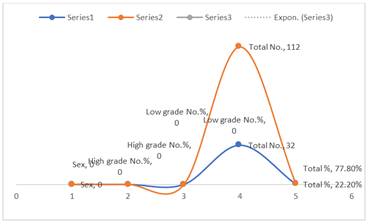
Figure 1: The low-grade tumour is more than the high-grade tumour.
|
Occupation |
High grade |
Low grade |
Total |
Total |
|
No. % |
No. % |
No. |
% |
|
|
Business |
17(28.8%) |
17(20%) |
34 |
23.6% |
|
Cultivator |
22(37.3%) |
39(45.9%) |
61 |
42.4% |
|
Employee |
13(22%) |
5(5.9%) |
18 |
12.5% |
|
House maker |
7(11.9%) |
24(28.2%) |
31 |
21.5% |
|
Total |
59(100%) |
85(100%) |
144 |
100% |
Pearson chi2(3) =13.3568 pr =0.004
Table 2: Occupational Impact on TCC.
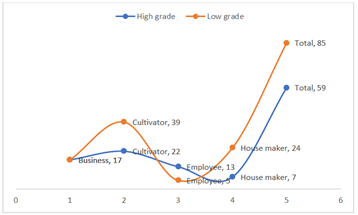
Figure 2: Cultivators are more sufferer.
|
Urban/Rural |
High grade |
Low grade |
Total |
Total |
|
No. % |
No. % |
No. |
% |
|
|
Rural |
32(54.2%) |
54(63.5%) |
86 |
59.7% |
|
Urban |
27(45.8%) |
31(36.5%) |
58 |
40.3% |
|
Total |
59(100%) |
85(100%) |
144 |
100% |
Pearson chi2(1) =1.2501 pr =0.264
Table 3: Impact of habitant on TCC.

Figure 3: People living in rural areas suffer more.
|
Tobacco consumer or not |
High grade |
Low grade |
Total |
Total |
|
No. % |
No. % |
No. |
% |
|
|
No |
12(20.3%) |
33(38.8%) |
45 |
31.3% |
|
Yes |
47(79.7%) |
52(61.2%) |
99 |
68.8% |
|
Total |
59(100%) |
85(100%) |
144 |
100% |
Pearson chi2(1) =5.5386 pr = 0.019
Table 4: Association between tobacco consumption and grading of TCC.
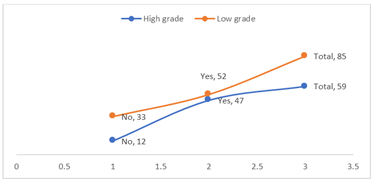
Figure 4: Tobacco consumers have more TCC than non-tobacco consumers.
|
Age |
High grade |
Low grade |
Total |
Total |
|
No. % |
No. % |
No. |
% |
|
|
25-49 years |
11(18.6%) |
3(3.5%) |
14 |
9.7% |
|
50-69 years |
31(52.5%) |
47(55.3%) |
78 |
54.2% |
|
70 years and above |
17(28.8%) |
35(41.2%) |
52 |
36.1% |
|
Total |
59(100%) |
85(100%) |
144 |
100% |
Pearson chi2(2) =9.7062 pr= 0.008
Table 5: Grading of TCC in the age group.
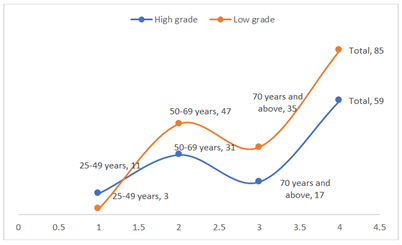
Figure 5: The age group (52-69) suffers more.
|
Variable |
Obs |
Mean |
Standard deviation |
|
|
High |
Age |
59 |
59.5 |
13.5 |
|
Creatinine |
59 |
1.4 |
0.5 |
|
|
Haemoglobin |
59 |
10.5 |
1.9 |
|
|
Low |
Age |
85 |
65.5 |
10.7 |
|
Creatinine |
85 |
1.2 |
0.3 |
|
|
Haemoglobin |
85 |
10.6 |
1.4 |
Table 6: Correlation between grading of TCC and age, haemoglobin & creatinine level of patients.
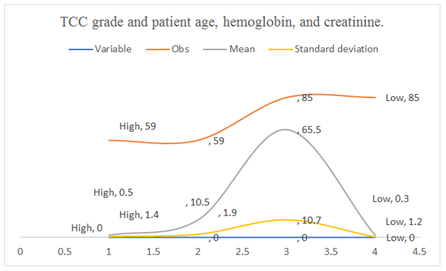
Figure 6: High-grade tumours average 59.5 years old with 1.4 Creatinine and 10.5 gm/dl haemoglobin. Low-grade tumours average 65.5 years old with 1.2 Creatinine and 10.6 gm/dl haemoglobin.
4. Discussion
Due to their worldwide frequency, urological malignancies are a real public health problem [14]. Urological malignancies are remarkably increasing in the ageing population [15]. Some lifestyle habits, such as smoking, physical activity, nutrition, sexual activity and personal hygiene are modifiable factors influencing the development and progression of urological cancers [16]. In GLOBOCAN 2020, Bangladesh shows prostate cancer ranks 17, bladder cancer 18, kidney cancer 20, ca-penis 27 and testicular cancer 30th position [2]. In this study, most of the sufferers are from the 50-69 years age group from rural areas with a habit of tobacco consumption and occupation by cultivation. Because this part of the country has the least industrial but more agricultural development. Among them, low-grade tumours are more common. But in the tobacco consumer group, high-grade tumours are common. Urothelial cancer is 4th most common cancer in men and 8th most common cancer in women in the Western world [17]. In Indian data, Genito-urinary systems formed 17.48% of all cancers in male patients, among them carcinoma prostate at 40.71% and urinary bladder cancer at 30.49% [18]. About 50-65% of all bladder cancers are due to tobacco consumption and 20% are for occupational and environmental toxins. Bladder cancer is a prime candidate for preventable cancer, with 81% of cases having known risk factors [5]. There are lots of etiological risk factors for bladder cancers i.e.: male gender, older age, hereditary and genetic factors, tobacco, environmental and occupational exposures, alcohol, red meat, obesity, pathogens like Schistosomiasis etc.
Beta-naphthylamine and polycyclic aromatic hydrocarbons, both found in tobacco, are known carcinogens. Inflammation induced by these particles ultimately leads to DNA adduction and permanent genetic mutation. In which oncogenes are activated or tumour suppressor genes are downregulated to promote carcinogenesis [5]. The second most common modifiable risk factor for bladder cancer is exposure to carcinogens in the workplace and the environment. Aromatic amines, polycyclic aromatic hydrocarbons, and chlorinated hydrocarbons are all known carcinogens that can be found in a wide range of commonplace materials like paint, metal, rubber, and petroleum products. Firefighters, cosmetologists, and farmers who use fungicides also face a higher risk [5]. According to the results of a large Chilean prospective observational study, being exposed to arsenic raises the risk of bladder cancer [19]. Other study indicated that the chance of developing bladder cancer was greatly enhanced by smoking in combination with exposure to extremely low amounts of arsenic (0.5 g/L) [20]. Nitrates and disinfection byproducts in municipal water supplies, as well as dietary elements like selenium and zinc, have all been linked to an increased risk of bladder cancer [21]. Chinese herbal products containing aristolochic acid found naturally in many plants belonging to the genus Aristolochia are a potent carcinogen for bladder cancer [22].
In our study all the urothelial cancers are transitional cell carcinoma, no other subtypes are detected. But in an Indian study [18], it was 97.71%. The male is more preponderance and the male-female ratio was 3.6:1, which is similar to China, Togo and the Western world [23, 8, 5]. But in India, it was 6.4:1 [18] and in Korea 5.68:1 [6]. There were significant differences in bladder cancer incidence rates in urban and rural areas. Incidence in rural areas is 59.7% is much higher than in urban areas 40.3% which is similar to a study by Adam John Gadzinski [10]. But in China [23] urban people suffer more. In this study, the most common age group is between 50 to 69 years of age and the mean age is 63 with a standard deviation of 12.1, which is similar to another study [17, 24, 5]. But a study from Africa [8] observes in much lower age group. Among the occupational status of the patients, cultivators are suffering more from urothelial cancer. This may be due to prolonged exposure to fungicides, arsenic and socioeconomic deprivation. Smokers are suffering more from urothelial cancer about 68.8%, among them 79.7% are high-grade tumours which is similar to other studies [5, 6, 18].
5. Conclusion
In this study, all of the urothelial malignancies are in the form of transitional cell carcinoma. Most of the sufferers are in the elderly age group at the age of 50-69 years age group who lived in rural areas and are tobacco consumers and cultivators. Men had a higher incidence rate than Women. In African countries, squamous cell carcinoma of the bladder is found due to the prevalence of Schistosomiasis and the affected are the younger age group. Most of the TCC is low grade and NMIBCa, and TURBT with intravesical therapy have a large impact on survival. But in the case of high-grade and MIBCa, radical cystectomy is the gold standard but is associated with morbidity and decreased quality of life. Metastatic TCC is a highly lethal disease with a limited survival rate. As most urological cancers are linked with modifiable risk factors, the incidence rate of these cancers can be reduced by improving public awareness and the healthcare system. Early diagnosis and treatment are the keys to improving urological cancer survival.
Conflicts of Interest
There are no conflicts of interest.
Financial Support and Sponsorship
Nil.
Informed Consent Statement
Not applicable.
References
- Putri RA, Imelda L, Delyuzar L. The Correlation of Tumor Budding Index with Grading of Infiltrating Urothelial Carcinoma. Int J Sci Res Publ IJSRP 11 (2021): 441-445.
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians 68 (2018): 394-424.
- Humphrey PA, Moch H, Cubilla AL, et al. The 2016 WHO classification of tumours of the urinary system and male genital organs-part B: prostate and bladder tumours. European urology 70 (2016): 106-119.
- Richters A, Aben KK, Kiemeney LA. The global burden of urinary bladder cancer: an update. World journal of urology 38 (2020): 1895-1904.
- Saginala K, Barsouk A, Aluru JS, et al. Epidemiology of bladder cancer. Medical sciences 8 (2020): 15.
- Joung JY, Lim J, Oh CM, et al. Current trends in the incidence and survival rate of urological cancers in Korea. Cancer research and treatment: official Journal of Korean Cancer Association 49 (2017): 607-615.
- Rébillard X, Grosclaude P, Leone N, et al. Projection of incidence and mortality from urological cancer in France in 2012. Progress in urology 23 (2013): S57-S65.
- Darré T, Amégbor K, Kpatcha M, et al. Urological cancers in Togo: histoepidemiological profile apropos of 678 cases. J Afr cancer 6 (2014): 27-31.
- Forman D. Cancer Incidence by Deprivation, England, 1995–2004. National Cancer Intelligence Network (2008).
- Gadzinski AJ, Gore JL, Odisho AY, et al. Urological malignancy incidence rates over time by county rurality (2020).
- Eble JL, Sauter G, Epstein JI. Pathology and Genetics of Tumours of the Urinary System and Male Genital Organs: WHO Classification of Tumours, Volume 7. World Health Organization (2004).
- Metts MC, Metts JC, Milito SJ, et al. Bladder cancer: a review of diagnosis and management. Journal of the National Medical Association 92 (2000): 285.
- Dobruch J, Oszczudlowski M. Bladder cancer: current challenges and future directions. Medicina 57 (2021): 749.
- Dy GW, Gore JL, Forouzanfar MH, et al. Global burden of urologic cancers, 1990–2013. European urology 71 (2017): 437-446.
- Yaméogo CA, Ouédraogo AS, Ouattara A, et al. Urological Cancers in Burkina Faso: Epidemiological and Anatomopathological Aspects of 2204 Cases. Open Journal of Urology 10 (2020): 111-122.
- Emilio S, Luigi V, Riccardo B, et al. Lifestyle in urology: Cancer. Urologia Journal 86 (2019): 105-114.
- Parkin DM, Whelan SL, Ferlay J, et al. Cancer incidence in five continents volume VIII. IARC scientific publication (2002).
- Yuvaraja TB, Waigankar S, Bakshi G, et al. Genitourinary cancers: Summary of Indian data. South Asian Journal of Cancer (2016): 122-124.
- Marshall G, Ferreccio C, Yuan Y, et al. Fifty-year study of lung and bladder cancer mortality in Chile related to arsenic in drinking water. Journal of the National Cancer Institute 99 (2007): 920-928.
- Kurttio P, Pukkala E, Kahelin H, et al. Arsenic concentrations in well water and risk of bladder and kidney cancer in Finland. Environmental Health Perspectives 107 (1999): 705-710.
- Meliker JR, Nriagu JO. Arsenic in drinking water and bladder cancer: review of epidemiological evidence. Trace Metals and other Contaminants in the Environment 9 (2007): 551-584.
- Nortier JL, Martinez MC, Schmeiser HH, et al. Urothelial carcinoma associated with the use of a Chinese herb (Aristolochia fangchi). New England Journal of Medicine 342 (2000): 1686-1692.
- Pang C, Guan Y, Li H, et al. Urologic cancer in China. Japanese journal of clinical oncology 46 (2016): 497-501.
- Bowa K, Kachimba JS, Labib MA, et al. The changing pattern of urological cancers in Zambia. Medical Journal of Zambia 35 (2008).


 Impact Factor: * 4.1
Impact Factor: * 4.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 