Autologous Platelet Rich Plasma-A Biological Therapeutic Option for Retrocalcaneal Bursitis and its Associations
Article Information
Madhan Jeyaraman1*, Vishalkumar S Patel2, Hardik J Dhamshania1, Naveen Jeyaraman3, Preethi Selvaraj4
1Department of Orthopaedics, JJM Medical College, Davangere, Karnataka, India
2Department of Orthopaedics, Navodhaya Medical College and Research Institute, Raichur, Karnataka, India
3Department of Orthopaedics, Kasturba Medical College, Manipal, Karnataka, India
4Department of Community Medicine, SRM Medical College and Research Centre, Chennai, India
*Corresponding Author: Madhan Jeyaraman, Department of Orthopedics, JJM Medical College, Davangere, Karnataka, India
Received: 13 April 2019; Accepted: 24 April 2019; Published: 29 April 2019
Citation: Madhan Jeyaraman, Vishalkumar S Patel, Hardik J Dhamshania, Naveen Jeyaraman, Preethi Selvaraj. Autologous Platelet Rich Plasma-A Biological Therapeutic Option for Retrocalcaneal Bursitis and its Associations. Journal of Orthopaedics and Sports Medicine 1 (2019): 018-027.
View / Download Pdf Share at FacebookAbstract
Background: Retrocalcaneal bursitis is the inflammation of the bursa between the anterior aspect of the Achilles and posterior aspect of the calcaneum which is associated with achilles tendinitis, plantar fasciitis, calcaneal spurs, fibromyalgia and rheumatoid arthritis.
Objectives: This study is conducted to review a series of patients prospectively with symptomatic retrocalcaneal bursitis and its associations to determine if PRP injections (1) provide symptomatic relief, (2) improved VAS and AOFAS scores and (3) alleviation of need of surgery.
Materials and Methods: After screening of cases, 128 cases entered into the study and have been treated with an autologous platelet rich plasma injection with due pre and post procedural care. The cases are followed up on day 0, at the end of 1st week, 1st and 6th month for pain and range of movements. The patients are followed up for complications and the data were analyzed statistically.
Results: Out of 128 cases, 76 patients (59.37%) improved with 1st dose and a further 38 patients (29.68%) with a 2nd dose of autologous PRP injection with an interval of 3 weeks from the first dose. A total of 89.05% of patients, who got treated with autologous PRP injection, had a good clinical and functional outcome even at the end of 1 year of injections and presented with statistically significant results with a p value <0.001. No adverse reactions and serious complications are noted in the study participants.
Conclusion: The autologous PRP injection is considered superior in treatment of retrocalcaneal bursitis, which minimise the pain and improve the functional quality of life.
Keywords
Platelet rich plasma, Plantar fasciitis, Retrocalcaneal bursitis, Achilles tendinitis
Orthopaedics articles Orthopaedics Research articles Orthopaedics review articles Orthopaedics PubMed articles Orthopaedics PubMed Central articles Orthopaedics 2023 articles Orthopaedics 2024 articles Orthopaedics Scopus articles Orthopaedics impact factor journals Orthopaedics Scopus journals Orthopaedics PubMed journals Orthopaedics medical journals Orthopaedics free journals Orthopaedics best journals Orthopaedics top journals Orthopaedics free medical journals Orthopaedics famous journals Orthopaedics Google Scholar indexed journals Retrocalcaneal bursitis articles Retrocalcaneal bursitis Research articles Retrocalcaneal bursitis review articles Retrocalcaneal bursitis PubMed articles Retrocalcaneal bursitis PubMed Central articles Retrocalcaneal bursitis 2023 articles Retrocalcaneal bursitis 2024 articles Retrocalcaneal bursitis Scopus articles Retrocalcaneal bursitis impact factor journals Retrocalcaneal bursitis Scopus journals Retrocalcaneal bursitis PubMed journals Retrocalcaneal bursitis medical journals Retrocalcaneal bursitis free journals Retrocalcaneal bursitis best journals Retrocalcaneal bursitis top journals Retrocalcaneal bursitis free medical journals Retrocalcaneal bursitis famous journals Retrocalcaneal bursitis Google Scholar indexed journals Achilles tendinitis articles Achilles tendinitis Research articles Achilles tendinitis review articles Achilles tendinitis PubMed articles Achilles tendinitis PubMed Central articles Achilles tendinitis 2023 articles Achilles tendinitis 2024 articles Achilles tendinitis Scopus articles Achilles tendinitis impact factor journals Achilles tendinitis Scopus journals Achilles tendinitis PubMed journals Achilles tendinitis medical journals Achilles tendinitis free journals Achilles tendinitis best journals Achilles tendinitis top journals Achilles tendinitis free medical journals Achilles tendinitis famous journals Achilles tendinitis Google Scholar indexed journals Plantar fasciitis articles Plantar fasciitis Research articles Plantar fasciitis review articles Plantar fasciitis PubMed articles Plantar fasciitis PubMed Central articles Plantar fasciitis 2023 articles Plantar fasciitis 2024 articles Plantar fasciitis Scopus articles Plantar fasciitis impact factor journals Plantar fasciitis Scopus journals Plantar fasciitis PubMed journals Plantar fasciitis medical journals Plantar fasciitis free journals Plantar fasciitis best journals Plantar fasciitis top journals Plantar fasciitis free medical journals Plantar fasciitis famous journals Plantar fasciitis Google Scholar indexed journals Calcaneal spurs articles Calcaneal spurs Research articles Calcaneal spurs review articles Calcaneal spurs PubMed articles Calcaneal spurs PubMed Central articles Calcaneal spurs 2023 articles Calcaneal spurs 2024 articles Calcaneal spurs Scopus articles Calcaneal spurs impact factor journals Calcaneal spurs Scopus journals Calcaneal spurs PubMed journals Calcaneal spurs medical journals Calcaneal spurs free journals Calcaneal spurs best journals Calcaneal spurs top journals Calcaneal spurs free medical journals Calcaneal spurs famous journals Calcaneal spurs Google Scholar indexed journals Fibromyalgia articles Fibromyalgia Research articles Fibromyalgia review articles Fibromyalgia PubMed articles Fibromyalgia PubMed Central articles Fibromyalgia 2023 articles Fibromyalgia 2024 articles Fibromyalgia Scopus articles Fibromyalgia impact factor journals Fibromyalgia Scopus journals Fibromyalgia PubMed journals Fibromyalgia medical journals Fibromyalgia free journals Fibromyalgia best journals Fibromyalgia top journals Fibromyalgia free medical journals Fibromyalgia famous journals Fibromyalgia Google Scholar indexed journals Rheumatoid arthritis articles Rheumatoid arthritis Research articles Rheumatoid arthritis review articles Rheumatoid arthritis PubMed articles Rheumatoid arthritis PubMed Central articles Rheumatoid arthritis 2023 articles Rheumatoid arthritis 2024 articles Rheumatoid arthritis Scopus articles Rheumatoid arthritis impact factor journals Rheumatoid arthritis Scopus journals Rheumatoid arthritis PubMed journals Rheumatoid arthritis medical journals Rheumatoid arthritis free journals Rheumatoid arthritis best journals Rheumatoid arthritis top journals Rheumatoid arthritis free medical journals Rheumatoid arthritis famous journals Rheumatoid arthritis Google Scholar indexed journals Chondrocytes articles Chondrocytes Research articles Chondrocytes review articles Chondrocytes PubMed articles Chondrocytes PubMed Central articles Chondrocytes 2023 articles Chondrocytes 2024 articles Chondrocytes Scopus articles Chondrocytes impact factor journals Chondrocytes Scopus journals Chondrocytes PubMed journals Chondrocytes medical journals Chondrocytes free journals Chondrocytes best journals Chondrocytes top journals Chondrocytes free medical journals Chondrocytes famous journals Chondrocytes Google Scholar indexed journals Physical therapy articles Physical therapy Research articles Physical therapy review articles Physical therapy PubMed articles Physical therapy PubMed Central articles Physical therapy 2023 articles Physical therapy 2024 articles Physical therapy Scopus articles Physical therapy impact factor journals Physical therapy Scopus journals Physical therapy PubMed journals Physical therapy medical journals Physical therapy free journals Physical therapy best journals Physical therapy top journals Physical therapy free medical journals Physical therapy famous journals Physical therapy Google Scholar indexed journals Biological therapy articles Biological therapy Research articles Biological therapy review articles Biological therapy PubMed articles Biological therapy PubMed Central articles Biological therapy 2023 articles Biological therapy 2024 articles Biological therapy Scopus articles Biological therapy impact factor journals Biological therapy Scopus journals Biological therapy PubMed journals Biological therapy medical journals Biological therapy free journals Biological therapy best journals Biological therapy top journals Biological therapy free medical journals Biological therapy famous journals Biological therapy Google Scholar indexed journals Surgical management articles Surgical management Research articles Surgical management review articles Surgical management PubMed articles Surgical management PubMed Central articles Surgical management 2023 articles Surgical management 2024 articles Surgical management Scopus articles Surgical management impact factor journals Surgical management Scopus journals Surgical management PubMed journals Surgical management medical journals Surgical management free journals Surgical management best journals Surgical management top journals Surgical management free medical journals Surgical management famous journals Surgical management Google Scholar indexed journals Platelet-rich plasma articles Platelet-rich plasma Research articles Platelet-rich plasma review articles Platelet-rich plasma PubMed articles Platelet-rich plasma PubMed Central articles Platelet-rich plasma 2023 articles Platelet-rich plasma 2024 articles Platelet-rich plasma Scopus articles Platelet-rich plasma impact factor journals Platelet-rich plasma Scopus journals Platelet-rich plasma PubMed journals Platelet-rich plasma medical journals Platelet-rich plasma free journals Platelet-rich plasma best journals Platelet-rich plasma top journals Platelet-rich plasma free medical journals Platelet-rich plasma famous journals Platelet-rich plasma Google Scholar indexed journals Pain articles Pain Research articles Pain review articles Pain PubMed articles Pain PubMed Central articles Pain 2023 articles Pain 2024 articles Pain Scopus articles Pain impact factor journals Pain Scopus journals Pain PubMed journals Pain medical journals Pain free journals Pain best journals Pain top journals Pain free medical journals Pain famous journals Pain Google Scholar indexed journals Ankle joint articles Ankle joint Research articles Ankle joint review articles Ankle joint PubMed articles Ankle joint PubMed Central articles Ankle joint 2023 articles Ankle joint 2024 articles Ankle joint Scopus articles Ankle joint impact factor journals Ankle joint Scopus journals Ankle joint PubMed journals Ankle joint medical journals Ankle joint free journals Ankle joint best journals Ankle joint top journals Ankle joint free medical journals Ankle joint famous journals Ankle joint Google Scholar indexed journals PRP injection articles PRP injection Research articles PRP injection review articles PRP injection PubMed articles PRP injection PubMed Central articles PRP injection 2023 articles PRP injection 2024 articles PRP injection Scopus articles PRP injection impact factor journals PRP injection Scopus journals PRP injection PubMed journals PRP injection medical journals PRP injection free journals PRP injection best journals PRP injection top journals PRP injection free medical journals PRP injection famous journals PRP injection Google Scholar indexed journals
Article Details
1. Introduction
Retrocalcaneal bursitis is the inflammation of the bursa between the anterior aspect of the Achilles and posterior aspect of the calcaneum which is most commonly seen in professional athletes. Retrocalcaneal bursitis is also associated with achilles tendinitis, plantar fasciitis, calcaneal spurs, fibromyalgia and rheumatoid arthritis [1]. The embryological origin of the plantar fascia seems to be united with the Achilles tendon [2] and this connection comprises a layer of periosteal fibers that declines in thickness and elastic properties with aging [3]. The ubiquitous presence of hyaluronate within plantar fascia enables the gliding of fibrous bundles and acts as an an efficient shock absorber and also serving an anti-inflammatory purpose [4]. The chondrocytes found near the heel insertion expresses a cartilaginous metaplasia that gradually reduces the connection between the Achilles tendon and the plantar fascia, reducing PF elasticity as a consequence [5]. The strong correlation between the thickness of plantar fascia and Achilles paratenon suggest in the case of plantar fascia thickening the characteristics of Achilles tendon and paratenon should also be evaluated. The patients with retrocalcaneal bursitis and its associations are unaware of the need for prompt treatment to prevent further complications. The various modalities of management of retrocalcaneal bursitis are pharmacological management, physical therapy, biological therapy and surgical management.
1.1 Objectives
To prospectively review a series of patients who have been treated with biological treatment with autologous platelet rich plasma injections for symptomatic retrocalcaneal bursitis and its associations to determine if PRP injections (1) provide symptomatic relief, (2) improved the visual analogue scale (VAS) score and functional AOFAS scores and (3) alleviation of need of surgery.
2. Materials and Methods
- Health care setup-Tertiary care hospital
- Setting-JJM Medical College, Davangere, Karnataka.
- Duration of the study-November 2016 to June 2018
- Type of the study-Prospective study
- Level of evidence-Level IV
- Sample size-211
- Selection of cases-Among 211 retrocalcaneal bursitis cases, 37 cases failed to satisfy the inclusion criteria, 25 cases lost follow up and 21 cases declined to participate the study as in Figure 1. The remaining 128 cases were taken up for this study who were treated with autologous platelet rich plasma injection as per our study protocol.
- The clinical entities involved in this study were retrocalcaneal bursitis with achilles tendinitis (n=37), retrocalcaneal bursitis (n=51) and retrocalcaneal bursitis with plantar fasciitis (n=40).
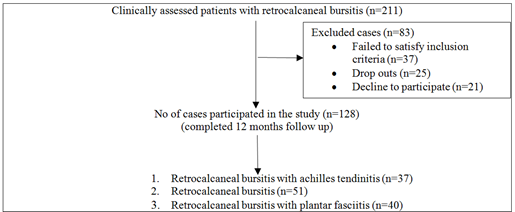
Figure 1: Patient’s selection.
2.1 Inclusion criteria
- Patients with retrocalcaneal bursitis with achilles tendinitis, retrocalcaneal bursitis and retrocalcaneal bursitis with plantar fasciitis who have taken conservative treatment without any improvement from past 6 months
- Patients with recalcitrant chronic retrocalcaneal bursitis without any improvement from past 6 months
- Patients who gave consent for treatment with autologous PRP injection as per our protocol
- Regular visits in the out-patient department.
2.2 Exclusion criteria
- Patients with haemoglobin <10 gm/dL and platelet count <105 /μL
- Patients with corticosteroid injection at treatment site within 1 month
- Patients with tendo-achilles rupture
- Patients with local infection at the site of the procedure, HIV, Hepatitis B or C, septicaemia and other systemic disorders
- Patients refusal for PRP treatment as per our protocol.
After getting institute ethical committee clearance and informed written consent from the patients enrolled in our study, they were subjected for thorough clinical examination and to investigate the duration of the disease and the nature of management taken prior to autologous platelet rich plasma treatment. The baseline investigations and radiographic analysis such as plain x ray and ultrasound examination of the pathological sites were analyzed. All the cases were investigated for the usage of NSAIDs 72 hours prior and local steroid infiltration 4 weeks prior to autologous PRP injection. 20 cc of venous blood was withdrawn in 3.8% sodium citrate vacutainers and subjected for 1st centrifugation at a rate of 3000 rpm for 10 minutes. Then the plasma was separated in plain vacutainers and subjected for 2nd centrifugation at a rate of 5000 rpm for 10 minutes. The resultant solution contain upper 2/3rd platelet poor plasma and lower 1/3rd platelet rich plasma. The procedure of platelet rich plasma preparation have been mentioned in Figure 2. Every 20 cc of venous blood yield 3-4 ml of platelet rich plasma solution. Before injecting PRP solution, add 10% of calcium chloride to PRP solution in the ratio of 1:10.
All the cases enrolled in the study were injected with 3-4 ml of autologous platelet rich plasma injection along the inflamed retrocalcaneal bursa, plantar fascia and achilles tendon. The techniques of injection of platelet rich plasma to retrocalcaneal bursitis and plantar fasciitis have been mentioned in figure 3 and 4. The sterile dressing and crepe bandage were applied at the injection site. The patients were trained for home based ankle exercises. All the patients were advised for protected weight bearing for minimum of 2 weeks and the pain was combated with ice pack application. The patients who came with recurrence of pain and symptoms were given with second dose of autologous PRP injection with a time interval of 3 weeks of first injection. The functional status and severity of pain around the ankle joint were charted according to VAS and AOFAS score both pre-procedurally on day 0 and post-procedurally at the end of 1st week, 1st and 6th month. All the cases were followed up for 1 year post injection to know the status of efficacy of autologous PRP injection.
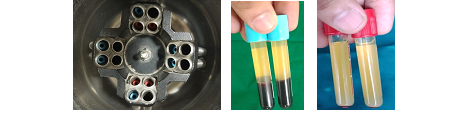
(a) (b) (c)
Figure 2: Platelet rich plasma preparation; (a) Process of differential centrifugation; (b) Image showing 1st centrifugation with separation of blood components; (c) Image showing 2nd centrifugation with upper 2/3rd of PPP and lower 1/3rd of PRP solution.

Figure 3: Technique of PRP injection to left retrocalcaneal bursitis.

Figure 4: Technique of PRP injection to right plantar fasciitis.
3. Results
The data obtained from the participants of the study were subjected to repeated measures ANOVA test and the following results are obtained. The demographic details (Table 1), the number of PRP injections given to alleviate the disease (Table 2), the statistical analysis (Table 3) and the complications (Table 4) have been discussed.
|
Disease |
Total |
Male |
Female |
Minimum age in years |
Maximum age in years |
Mean age in years |
|
Retrocalcaneal bursitis with achilles tendinitis |
37 |
22 (59.45%) |
15 (40.54%) |
32 |
69 |
51.15 |
|
Retrocalcaneal bursitis |
51 |
28 (54.90%) |
23 (45.09%) |
21 |
59 |
41.24 |
|
Retrocalcaneal bursitis with plantar fasciitis |
40 |
21 (52.50%) |
19 (47.50%) |
29 |
70 |
52.51 |
Table 1: Patients distribution after elimination.
Out of 128 cases, 71 cases (55.46%) were males and 57 cases (44.53%) were females. The mean age of patients participated in our study were 48.30 years with minimum age of 21 years and maximum age of 70 years.
|
Disease |
Total |
No of patients cured with 1st dose of autologous PRP (at end of 1st month follow up) |
No of patients cured with 2nd dose of autologous PRP |
No of patients with recalcitrant disease (at the end of 6th month follow up) |
No of recalcitrant disease patients cured at the end of 12th month |
|
Retrocalcaneal bursitis with achilles tendinitis |
37 |
23 (62.16%) |
11 (29.72%) |
3 (8.10%) |
2 (66.66%) |
|
Retrocalcaneal bursitis |
51 |
32 (62.74%) |
14 (27.45%) |
5 (9.80%) |
2 (40.00%) |
|
Retrocalcaneal bursitis with plantar fasciitis |
40 |
21 (52.50%) |
13 (32.50%) |
6 (15.00%) |
3 (50.00%) |
Table 2: Number of PRP injections.
|
Disorder |
Scoring |
Repeated measures ANOVA test (p value) |
|||
|
Pre procedure |
Post procedure |
||||
|
1st week |
1st month |
6th month |
|||
|
Retrocalcaneal bursitis with achilles tendinitis (n=37) |
VAS |
0.691 |
0.274 |
0.001 |
<0.001 |
|
AOFAS |
0.671 |
0.091 |
0.056 |
<0.001 |
|
|
Retrocalcaneal bursitis (n=51) |
VAS |
0.459 |
0.047 |
0.003 |
<0.001 |
|
AOFAS |
0.875 |
0.056 |
0.061 |
<0.001 |
|
|
Retrocalcaneal bursitis with plantar fasciitis (n=40) |
VAS |
0.513 |
0.261 |
0.024 |
<0.001 |
|
AOFAS |
0.677 |
0.287 |
0.047 |
<0.001 |
|
Table 3: p value of repeated measure ANOVA test.
Out of 128 cases, 76 patients (59.37%) reported pain relief with one dose of autologous PRP injection at the end of 1st month follow up and 38 patients (29.68%) reported pain relief after 2nd dose of injection which was given at the interval of 3 weeks from the first dose. 14 patients (10.93%) presented with recalcitrant disease after 6 months of first dose. All 14 recalcitrant cases have been given with one more dose of autologous PRP injection. Out of 14 cases, 7 patients got cured by the end of the 12th month follow up. At the end of the 12th month, 1 case (33.33%) of retrocalcaneal bursitis with achilles tendinitis, 3 cases (60.00%) of retrocalcaneal bursitis and 3 cases (50.00%) of retrocalcaneal bursitis with plantar fasciitis remained as recalcitrant disease. Overall, our study showed a statistically significant difference between pre-procedural and post-procedural scores in subjective (VAS) and functional (AOFAS) scoring system. The patients, who took autologous PRP injection, showed a statistically significant (p < 0.001) improvement in all three clinical entities included in the study.
|
Disease |
Total |
Pain |
Swelling |
Recurrence |
|
Retrocalcaneal bursitis with achilles tendinitis |
37 |
17 (45.94%) |
14 (37.83%) |
1 (2.70%) |
|
Retrocalcaneal bursitis |
51 |
29 (56.86%) |
19 (37.25%) |
3 (5.88%) |
|
Retrocalcaneal bursitis with plantar fasciitis |
40 |
17 (42.50%) |
13 (32.50%) |
3 (7.50%) |
|
Total no of cases |
128 |
63 (49.21%) |
46 (35.93%) |
7 (5.46%) |
Table 4: Complications.
The complications found in our patients were pain at the injection site in 63 cases (49.21%), swelling in 46 cases (35.93%) and recurrence of symptoms in 7 cases (5.46%). No other adverse reactions were noted in the patients participated in the study. All 7 recalcitrant cases were counselled for surgical management.
4. Discussion
There is a strong positive correlation and temporal association existing between the occurrence of plantar fasciitis, retrocalcaneal bursitis and achilles tendinopathy [1, 6].
4.1 Retrocalcaneal bursitis and Haglund deformity
Retrocalcaneal bursitis is the inflammation of the bursa between the anterior aspect of the Achilles and posterior aspect of the calcaneum. In some cases, retrocalcaneal bursitis may be caused by bursal impingement between the Achilles tendon and an excessively prominent posterosuperior aspect of the calcaneus (Haglund deformity). In Haglund disease, impingement occurs during ankle dorsiflexion. Retrocalcaneal bursitis is also associated with achilles tendinitis, plantar fasciitis, calcaneal spurs, fibromyalgia and rheumatoid arthritis. In retrocalcaneal bursitis, the pain is localized to anterior and 2 to 3 cm proximal to the achilles tendon insertion, pain with dorsiflexion and a bony prominence at achilles insertion [6].
4.2 Achilles tendinopathy
Achilles tendinopathy occurs in middle-aged and elderly patients with a tight heel cord. The mechanism of achilles tendinopathy is due to repetitive trauma leads to inflammation followed by cartilaginous and bony metaplasia, imbalance of dorsiflexors and plantar flexors, poor tendon blood supply, fluoroquinolone antibiotics and inflammatory arthropathy. The pathogenesis behind achilles tendinopathy is due to the abnormal vascularity 2 to 6 cm proximal to Achilles insertion in response to repetitive microscopic tearing of the tendon. The plain radiograph shows bone spur and intratendinous calcification. MRI shows disorganized tissue will show up as intrasubstance intermediate signal intensity and thickened tendons [6].
4.3 Plantar fasciitis
Plantar fasciitis is a chronic self-limiting condition due to overuse of plantar fascia, which is characterized by micro tears, the breakdown of collagen, and scarring. Between 4% and 7% of people have heel pain at any given time and about 80% of these cases are due to plantar fasciitis. The pain is usually most severe with the first steps of the day or following a period of rest. Pain is also frequently brought on by bending the foot and toes up towards the shin and may be worsened by a tight achilles tendon. In about a one-third of the population, both legs are affected. Most common site of abnormality in patients with plantar fasciitis is near the origin or enthesitis of the central band of plantar aponeurosis at medial plantar tubercle of calcaneus. Patient walk with an equinus gait to avoid placing pressure on painful heel. On examination, tenderness on the medial plantar calcaneal region as a sharp stabbing pain is felt. Passive ankle or first toe dorsiflexion elicits pain. When plantar fasciitis is bilateral, it is associated with rheumatoid arthritis, SLE and gout [7].
Platelet rich plasma, a potent “Orthobiologic”, is defined as the volume of supernatant containing plasma with platelet concentration of 105-106 above the baseline, which is a potent osteogenic, osteointegrative and osteorejuvenative agent [8]. The rationale behind platelet rich plasma in the management of retrocalcaneal bursitis and its associations are due to the interplay between histopromotive factors and rejuvenating micromolecules present in the platelets. The binding of growth factor to target cell receptor induces a signal transduction mechanism which produces chemotaxis, cell proliferation and osteoblastic differentiation [9]. The growth factors undergo tyrosine autophosphorylation to catabolise the further phosphorylation of other growth factors [10-12]. The half life of growth factors are from minutes to hours. The growth factors can exert an inhibitory effect once a certain amount of concentration is reached. Once activated, the platelet rich plasma forms a coagulum which contain growth factors. About 70% of growth factors are released from α granules of platelets within 10 minutes of the injection. These growth factors rejuvenate the diseased and degenerated tissues. The dose response relationship of platelet rich plasma follows a sigmoid shaped curve.
Ferrero G, et al. injected autologous PRP under ultrasound guidance for 30 achilles tendinopathy and 28 patellar tendinopathy cases. All the patients were evaluated with VISA scale. At the end of 6th month follow up, VISA score drastically improved from the baseline. Ultrasound evaluation showed an improvement in fibrillar texture of diseased and degenerated tendons. They concluded that autologous PRP as a therapeutic option for achilles and patellar tendinopathy with a great accuracy [13]. Venkatesh Gupta, Divya Bandari conducted a study on autologous platelet rich plasma injection in 60 cases of tennis elbow and 40 cases of plantar fasciitis. The results of autologous PRP injection have been evaluated with VAS, DASH and FHSQ scoring system. Both groups of patients were clinically and functionally evaluated after 4th and 8th week of initial PRP injection, which showed statistically significant improvement in pain and quality of life [14].
In this article, we considered autologous platelet rich plasma injection as the biological and minimally invasive therapeutic option for retrocalcaneal bursitis and its associations. Which show the functional improvement in 76 patients (59.37%) with 1st dose of autologous PRP injection and a further 38 patients (29.68%) with 2nd dose of autologous PRP injection with an interval of 3 weeks from the first dose. A total of 89.05% of patients, who got treated with autologous PRP injection, had a good clinical and functional outcome even at the end of 1 year of injections and presented with statistically significant results with a p value <0.001.
5. Limitation
- No comparison group was considered in the study
- Standardization of PRP injection protocol has to be figured out.
6. Conclusion
Though the literatures available for autologous PRP therapy for retrocalcaneal bursitis are very less, we tried evaluating the efficacy and durability of autologous PRP therapy for retrocalcaneal bursitis and its associations which proved to improve the quality of pain and functional quality of life. Hence, we conclude the biological therapeutics of platelet rich plasma for retrocalcaneal bursitis is more beneficial than other pharmacological modalities of treatment. Further RCT and meta analysis on PRP therapy for retrocalcaneal bursitis should come up which would guide the clinicians for better understanding of the disease and the treatment option.
Conflicts of Interest
Nil
Funding sources
Nil
Acknowledgements
None
References
- Pekala PA, Henry BM, Pekala JR, et al. The Achilles tendon and the retrocalcaneal bursa. Bone Joint Res 6 (2015): 446-451.
- Shaw HM, Vazquez OT, McGonagle D, et al. Development of the human Achilles tendon enthesis organ. J Anat 213 (2008): 718-724.
- Snow SW, Bohne WH, DiCarlo E, et al. Anatomy of the Achilles tendon and plantar fascia in relation to the calcaneus in various age groups. Foot Ankle Int 16 (1995): 418-421.
- Neuman MG, Nanau RM, Oruna L, et al. In vitro anti-inflammatory effects of hyaluronic acid in ethanol-induced damage in skin cells. J Pharm Pharm Sci 14 (2011): 425-437.
- Kim PJ, Martin E, Ballehr L, et al. Variability of insertion of the Achilles tendon on the calcaneus: an MRI study of younger subjects. J Foot Ankle Surg 50 (2011): 41-43.
- Jones DE. Retrocalcaneal Bursitis and Insertional Achilles Tendinitis. Sports Med Arthroscopy Rev 2 (1994): 301-309.
- Martin J O’Malley, Turner Vosseller J, Yang Gu. Successful Use of Platelet-Rich Plasma for Chronic Plantar Fasciitis. HSSJ 9 (2013): 129-133.
- Ramesh R, Madhan Jeyaraman, Prajwal GS. Autologous Platelet Rich Plasma Therapy in Orthopaedics-A Clinical Update. Nat J Clin Orthop 2 (2018): 33-36.
- Simpson AHR. Mills L. Noble B: The role of growth factors and related agents in accelerating farcture healing. J Bone Joint Surg Br 88 (2006): 701-705.
- Eduardo Anitua, Ramon Cugat, Mikel Sanchez. Platelet rich plasma in orthopaedics and sports medicine, Switzerland, Springer, (1st), Chapter 3 (2018): 47-64.
- Anitua E, Andia I, Ardanza B, et al. Autologus platelets as a source of proteins for healing and tissue regeneration. Thromb Haemost 91 (2004): 4-15.
- Sheth U, Simunovic N, Klein G, et al. Efficacy of autologous platelet rich plasma use for orthopaedic indications: a meta-analysis. J Bone Joint Surg Am 94 (2012): 298-307.
- Ferrero G, Fabbro E, Orlandi E, et al. Ultrasound-guided injection of platelet-rich plasma in chronic Achilles and patellar tendinopathy. Journal of Ultrasound 15 (2012): 260-266.
- Venkatesh Gupta, Divya Bandari. Autologous platelet rich plasma injection in tennis elbow and plantar fasciitis. Current Orthopedic Practice 27 (2016): 405-408.


 Impact Factor: * 4.3
Impact Factor: * 4.3 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 